Abstract
Background and Objective
Current methods are not designed to relate the incidence of individual adverse events reported in clinical trials to the plurality of adverse events accumulated in spontaneous reporting databases during real-world use. We have previously reported on a pharmacological class-effect query of clinical trial data defined by a disproportionality analysis of the US Food and Drug Administration Adverse Event Reporting System (FAERS) post-marketing data. The aim of the current analysis was to apply a dopamine D2-based pharmacological class-effect query to clinical trial safety data of an atypical antipsychotic tested across different patient populations.
Methods
Patient-level adverse event data (n = 4400) from controlled clinical trials of the antipsychotic risperidone in schizophrenia, bipolar disorder, Alzheimer’s disease psychosis, and autism were obtained through the Yale University Open Data Access (YODA) project. An Empirical Bayes Geometric Mean analysis was performed, and a three-fold threshold incidence level was applied to determine if a preferred term met criteria for being an antipsychotic class-related adverse event.
Results
In pooled data from seven trials of adult schizophrenia, class-specific adverse events were identified in 49% of patients treated with risperidone; in 49% of risperidone-treated patients in two trials in adolescent schizophrenia; in 65% of risperidone-treated patients in four trials in adult bipolar disorder; in 50% of risperidone-treated patients in two trials in adolescent schizophrenia; in 36% of risperidone-treated patients in one trial in Alzheimer’s disease; and in 94% of risperidone-treated patients in one trial in autism.
Conclusions
The cumulative curves of class-specific adverse events in risperidone clinical trials of schizophrenia were similar to those first reported for other atypical antipsychotic drugs. However, the class-specific adverse event curves were notably lower for Alzheimer’s disease and higher for autism, suggesting that the diagnostic indication may have an important effect on the cumulative class-specific side-effect burden.
Similar content being viewed by others
Patient-level adverse event data were analyzed for 4400 patients in randomized placebo-controlled trials of the antipsychotic risperidone in schizophrenia, bipolar disorder, and Alzheimer’s disease psychosis. |
Adverse events of risperidone that were class specific (to the class of dopamine D2 antipsychotics) showed notable between-diagnosis differences in prevalence (e.g., lower for Alzheimer’s disease psychosis; higher for autism), suggesting that the diagnostic indication may have an important effect on the cumulative class-specific side-effect burden. |
1 Introduction
Schizophrenia is a chronic illness characterized by acute exacerbations of psychosis and progressive impairment in functioning and quality of life [1]. Despite evidence from studies that indicate more than one-third of all patients with a diagnosis of schizophrenia either discontinue their medication or do not take their medication as prescribed [2], treatment guidelines recommend maintenance therapy with antipsychotic medication because of the frequency of recurrent psychotic episodes and hospitalization [3]. Non-adherence has been identified as, by far, the biggest preventable risk factor for relapse and rehospitalization [3], and adverse events (AEs) have consistently been found to be the most common reason for discontinuing antipsychotic medication [4]. As a recent meta-analysis of 92 relapse prevention trials noted [5]: “effectiveness needs to be put into the context of tolerability, especially during long-term treatment. However, adverse effect outcomes [are] only partially and inconsistently reported, not allowing a detailed benefit-to-risk assessment.”
In addition to tolerability and adherence considerations, quite a few class-related safety events with health effects are associated with first-generation and second-generation antipsychotics acting via a dopamine D2 mechanism of action (MOA; “D2 antipsychotics”). These include prolactinemia, extrapyramidal side effects, and an array of adverse metabolic effects including impaired glucose tolerance, higher rates of diabetes mellitus, increased insulin resistance, elevated lipid levels, and obesity [6,7,8,9,10,11,12]. Of note, D2 antipsychotics appear to have effects on lipid metabolism and glucose regulation that are independent of body weight [13,14,15]. It is well established that schizophrenia is associated with increased cardiovascular mortality, and iatrogenic metabolic syndrome caused by D2 antipsychotics is likely to contribute to this increased mortality risk [16].
The efficacy of the current antipsychotic class of medications primarily relies on antagonist activity at D2 receptors, which is frequently associated with substantial disruption of motor, metabolic, and endocrine systems related to D2 receptor blockade and downstream consequences. The second-generation D2-binding antipsychotics are largely distinguished from first-generation antipsychotics by having additional antagonist activity at the serotonin 5-HT2A receptor, which disinhibits dopamine neurons, stimulating dopamine release that is hypothesized to result in competitive modulation of the antagonist D2 receptor activity of second-generation antipsychotic drugs such as risperidone.
ntipsychotics with non-D2 MOAs are in development [17, 18], which highlights the potential value of having a method for differentiating class-effect AEs based on the specific MOA classification of a drug (e.g., D2 vs non-D2).
Accurate and comprehensive assessment of the benefit-risk characteristics of antipsychotics (or any class of drugs) is limited by the fact that the total number of patients enrolled in all phases of a clinical development program is many orders of magnitude smaller than the number of patients who will be treated over the marketed life span of a given drug. The incidence of individual preferred terms (PTs) for adverse drug reactions (ADRs) reported in clinical trials are low relative to the occurrence of ADRs attributed to a pharmacological class during real-world use of a drug in the post-marketing period. Therefore, new approaches are needed to facilitate analyses of AEs in clinical studies relative to the pharmacological class effects seen in real-world use.
Since the late 1990s with the introduction of Medical Dictionary for Regulatory Activities (MedDRA) terminology, reporting of ADRs has been organized into five hierarchical levels including PTs, while standardized medical queries have facilitated the analysis of drug safety issues in clinical development [19, 20]. The development of a systematic and standardized nosology with broad international support was a crucial advance in facilitating effective understanding and communication of ADRs in the pharmacovigilance setting.
The authors have previously reported [21] a Bayesian disproportionality analytic strategy for identifying class-specific AEs for the class of antipsychotic drugs acting via the D2 receptor, utilizing US Food and Drug Administration Adverse Event Reporting System (FAERS) post-marketing data. This analytic strategy is a mechanism-based ontology utilizing a classificatory approach that represents an alternative method of summarizing safety data that is complementary to the current two methods: use of the MedDRA system-organ-class ontology and use of standardized medical queries. Furthermore, the authors presented pilot class-effect AE data for ulotaront, a novel trace amine-associated receptor 1 (TAAR1) agonist with 5-HT1A agonist activity, which acts via a non-D2 TAAR1 mechanism that exhibits a markedly different cumulative side-effect burden profile when compared with D2 antipsychotics, using this FAERS-based methodology.
Here, we apply the D2 class-effect query defined by FAERS, to the Yale University Open Data Access (YODA) risperidone clinical trials database. We sought to replicate the class-effect query of schizophrenia clinical trials using an independent data set, and to determine the applicability of this pharmacological class-effect query approach to clinical trials evaluating efficacy and safety in diagnoses other than schizophrenia (bipolar disorder, Alzheimer’s disease, psychosis, and autism).
2 Methods
We established a query of class-related antipsychotic AEs based on real-world AE data. A detailed description of the procedures utilized in the Empirical Bayes Geometric Mean (EBGM) analysis are provided in a previous publication [21]. In brief, PTs associated with a pool of 30 antipsychotics were identified and ranked by EBGM disproportionality analysis of the FAERS data. The FAERS data were accessed by Empirica™ Signal, Oracle’s pharmacovigilance software (version 8.1.1, release 2020Q2; Oracle Inc., Redwood City, CA, USA). The FAERS data included all pre-1997 spontaneous reporting system data, adverse event reporting system data through August 2012, and FAERS data from August 2012 to June 2020.
The current data set consisted of patient-level AE data from patients with schizophrenia, bipolar disorder, autism, or Alzheimer’s disease who received risperidone in 17 controlled clinical trials. These data were obtained through the YODA project [22].
2.1 Statistical Methods
Patient-level AE data from the 17 randomized, double-blind, placebo-controlled clinical trials of risperidone were sorted by PT according to their FAERS-EBGM ranking for the antipsychotic class [see 21]. The aim was to utilize the post-marketing FAERS data to characterize the total burden of class-related AEs for risperidone (vs placebo) in adult schizophrenia (seven trials), adolescent schizophrenia (two trials), adult bipolar disorder (four trials), and Alzheimer’s disease, psychosis, and autistic disorder (one trial each). The proportion of patients in each diagnostic group having an AE, taking risperidone or placebo, was plotted as a cumulative function of each PT’s class-related disproportional reporting in a real-world reporting FAERS database. Cumulative AE curves, as a proportion of all patients, and as a proportion of all patients reporting an AE, were used to describe the AE profiles as a cumulative function of each PT’s class-related disproportional reporting relative to real-world reporting in the FAERS database. In the current YODA data set (Table 1), the same EBGM three-fold threshold level [21] was applied to determine if a PT met criteria for being an antipsychotic class-related AE.
3 Results
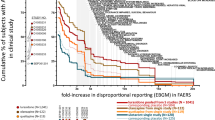
Patient-level AE data were analyzed for 4400 patients, including 2117 patients in seven clinical trials of adult patients with a diagnosis of schizophrenia, 439 patients in two trials in adolescent schizophrenia, 1251 patients in four clinical trials of adult patients with a diagnosis of bipolar disorder, 491 patients in two clinical trials of Alzheimer’s disease, and 102 patients in a trial of childhood autism. Figure 1 displays the cumulative proportion of patients with adult schizophrenia having an AE taking risperidone or placebo at or above the three-fold disproportional reporting threshold for each PT in FAERS. In Fig. 1, the x-axis is the fold increase in disproportional reporting of each PT calculated from the original pooled antipsychotic class in the FAERS database [21]. The y-axis is the cumulative proportion of patients in risperidone clinical trials with AEs that meet the three-fold EBGM threshold. The curve in Fig. 1 represents the cumulative AE burden (rising from right to left) across PTs in the class of antipsychotics. The proportion of subjects having an AE at or above the three-fold threshold is shown for individual studies is shown adjacent to the y-axis in Fig. 1. Overall, approximately 49% of patients treated with risperidone had AEs with PTs having EBGM values of threefold or greater, compared with 43% of the placebo patients. For two of the three placebo-controlled studies, the risperidone arm was associated with greater class-effect AEs than the corresponding placebo arms of the individual studies. The drug treatment arms of individual studies had larger EGBM50 values for drug treatment arms versus placebo arms, indicating a greater class specificity to the AEs associated with risperidone treatment versus the corresponding placebo treatment.
Class-specific adverse event (AE) burden in clinical trials of risperidone in adult schizophrenia [32–38]. Cumulative percent of patients (y-axis) with AEs taking risperidone or placebo that met the three-fold antipsychotic class-specific disproportional reporting based on the Empirical Bayes Geometric Mean (EBGM) analysis of post-marketing pharmacovigilance data [US Food and Drug Administration Adverse Event Reporting System (FAERS)]. The x-axis is the fold increase in disproportional reporting for each Preferred Term (PT) [21]
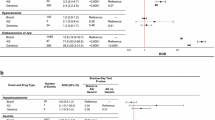
A total of 439 patients were randomized to risperidone (n = 385) or placebo (n = 54) in the pool of two clinical trials [24, 25] of adolescent patients with a diagnosis of schizophrenia (red curves in Fig. 2). Approximately 49% of patients treated with risperidone had AEs that met the three-fold EBGM threshold, compared with 28% of the placebo patients. A total of 1533 patients were exposed to risperidone in the pool of four clinical trials [28-31] of adult patients with a diagnosis of bipolar disorder (teal curves in Fig. 2). Approximately 65% of patients treated with risperidone had AEs with PTs having EBGM values of three-fold or greater. A total of 491 patients were randomized to risperidone (n = 245) or placebo (n = 246) in clinical trials [26, 27] of Alzheimer’s disease (green curves in Fig. 2). Approximately 36% of patients treated with risperidone had AEs with PTs having EBGM values of three-fold or greater, compared with 28% of placebo patients. A total of 102 patients were randomized to risperidone (n = 49) or placebo (n = 53) in clinical trials [23] of childhood patients with a diagnosis of autism. Approximately 94% of patients treated with risperidone had AEs with PTs having EBGM values of three-fold or greater, compared with 70% of placebo-treated patients. Cumulative AE curves for each of the individual studies are shown in Figs. 1–11 of the Electronic Supplementary Material.
Class-specific adverse event (AE) burden in clinical trials of risperidone in adult and adolescent schizophrenia, adult bipolar disorder, Alzheimer’s disease, and child and adolescent autism [27–42]. Cumulative percent of patients (y-axis) with AEs taking risperidone or placebo that met the three-fold antipsychotic class-specific disproportional reporting based on the Empirical Bayes Geometric Mean (EBGM) analysis of post-marketing pharmacovigilance data [US Food and Drug Administration Adverse Event Reporting System (FAERS)]. The x axis is the fold increase in disproportional reporting for each Preferred Term (PT) [21]
4 Discussion
Here, we demonstrate the applicability of a D2-based pharmacological class-effect query to historical clinical trial data collected with risperidone, including risperidone clinical trial data outside of the primary indication of schizophrenia for which antipsychotics are primarily used. The results reported here found that approximately half of the AEs experienced in schizophrenia clinical trials of risperidone were antipsychotic class-specific effects. The antipsychotic class-specific AEs for risperidone, displayed graphically, were qualitatively similar to the cumulative curves of class-specific AEs that the authors have previously reported for other atypical antipsychotic drugs [21]. The proportion of risperidone AEs that were class specific were also similar for risperidone studies of the bipolar disorder diagnosis. However, the proportion of class-specific effects, and the resulting cumulative class-effect curves, were notably higher for risperidone in a clinical trial of autism, and notably lower in two clinical trials of Alzheimer’s disease.
The concept of a pharmacologically defined class-effect query was first reported by the authors [21] in the identification of class-specific AEs for antipsychotic drugs acting via the D2 receptor. The class-effect query utilizes a Bayesian disproportionality analysis of the post-marketing FAERS database. To accomplish this, a total of 3.89 million PTs were identified in FAERS reporting of 30 marketed typical and atypical antipsychotics, and PTs having an EBGM above a three-fold criterion level were categorized as being “class-specific” antipsychotic AEs. The class-effect query is a data-analytic approach to define the clinically relevant mechanism-based terms and represents a third approach to summarize safety data that is complementary to the current two methods for summarizing safety data in drug trials, standardized medical queries and the (MedDRA) system-organ-class ontology.
The class-effect PTs include terms that are likely the result of the underlying conditions in the post-marketing database (referred to as indication bias, or here as indication-related PTs). In this work, the cumulative AE curves are influenced by PTs reflecting a possible indication bias. For example, in the schizophrenia trials in Fig. 1, the largest single “step” increase in incidence for placebo occurs for agitation at EGBM value of 4×. Agitation as an AE is likely owing to a lack of efficacy in the treatment of the underlying diagnosis of schizophrenia, rather than as a result of drug treatment. In the pooled schizophrenia studies, the cumulative curve stepped from 16% of subjects to 33% of subjects treated with placebo, whereas risperidone curve stepped from 30 to 40%, as would be expected for a greater incidence of agitation in subjects treated with placebo relative to risperidone.
The drug-treatment curves are generally above the placebo-treatment curves, suggesting that the side-effect burden is outpacing the lack-of-efficacy burden in the randomized controlled trials, at least when viewed through the lens of AE reporting in clinical trials for schizophrenia. The accumulation of AEs in clinical trials comparing drug versus placebo might be used to evaluate the balance of benefit (reduced incidence for indication-related PTs) versus risk (increased incidence of PTs for class effects). For example, the cumulative curves for placebo would rise due to an increased incidence of indication-related PTs (e.g., psychotic disorder-related symptoms), while the cumulative curves for a drug treatment arm would rise due to an increased incidence of class-effect PTs (e.g., extrapyramidal disorder). Conversely, the drug treatment arm would be lowered by increased efficacy (lower incidence) on PTs for the underlying disorder. If the drug’s side-effect burden curve is above its corresponding placebo curve, this indicates ‘the drug is associated with a greater side-effect burden than placebo, and that the lower-than-placebo incidence of AEs for indication-related PTs does not overcome the greater incidence of class-effect AEs’. However, if a drug’s cumulative curve lies below that of placebo, this indicates that placebo was associated with more harm to the patient (low incidence on indication-related PTs) and drug treatment lacked the expected class-effect burden (low incidence on other class-effect PTs). This portrayal allows one to visualize the risk to a patient in taking versus not taking a drug. Future trial designs and analysis plans might be proposed, where the degree of separation between the class-effect curves for drug treatment versus placebo treatment is utilized as an index of the balance of benefit versus risk.
The cumulative class-specific side-effect curves for risperidone appeared different for different patient populations, most notably, rates of class-specific AEs were lowest in clinical trials of Alzheimer’s disease, and highest in clinical trials of autism. In Alzheimer’s disease studies, agitation with a large (EGBM 4×) “step” increase in incidence was a likely a disease-related PT. In contrast, somnolence with a large (EGBM 3×) “step” increase in incidence compared with placebo was likely a drug-related class-effect PT. The cumulative side-effect curve for adolescents with autism were markedly more elevated than the curves observed for Alzheimer’s disease. These discordant results demonstrate the extent to which non-drug factors can override the cumulative side-effect trends in drug-related, D2 class-specific AEs previously reported for atypical antipsychotic drugs [21]. The reasons for the difference are likely owing to the lower daily doses used in the Alzheimer’s disease versus autism studies (1.0–1.5 mg vs 2.0–3.0 mg; despite a lower weight in adolescents with autism), and the possible reduction in reporting of AEs in patients with dementia compared with rates reported by adolescents with autism (and their parents/guardians).
In addition to the effects of dose, diagnosis, and other patient-related variables, limitations on the generation of reliable cumulative class-effect curves based on controlled clinical trials include the qualitative nature of safety data, rather than the availability of quantitative metrics that lend themselves to hypotheses that may be statistically tested. Additional research is needed to evaluate the potential for novel safety analyses to be incorporated in measures of benefit/risk in the clinical development of novel therapeutics.
5 Conclusions
Application of a novel class-effect query of the YODA risperidone clinical trials database found that the cumulative curves of class-specific AEs were similar to the curves that the authors have previously reported for other atypical antipsychotic drugs for the indication of schizophrenia. The class-specific AE curves were notably different for other diagnoses (lower for Alzheimer’s disease psychosis; higher for autism), suggesting that the diagnostic indication may have an important effect on the cumulative class-specific side-effect burden.
References
Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet. 2016;388(10039):86–97. https://doi.org/10.1016/S0140-6736(15)01121-6.
Correll CU, Rubio JM, Kane JM. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry. 2018;17:149–60. https://doi.org/10.1002/wps.20516.
Correll CU, Martin A, Patel C, Benson C, Goulding R, Kern-Sliwa J, et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. NPJ Schizophr. 2022;8:5. https://doi.org/10.1038/s41537-021-00192-x.
Alvarez-Jimenez M, Priede A, Hetrick SE, Bendall S, Killackey E, Parker AG, et al. Risk factors for relapse following treatment for first episode psychosis: a systematic review and meta-analysis of longitudinal studies. Schizophr Res. 2012;139:116–28. https://doi.org/10.1016/j.schres.2012.05.007.
Ostuzzi G, Bertolini F, Tedeschi F, Vita G, Brambilla P, Del Fabro L, et al. Oral and long-acting antipsychotics for relapse prevention in schizophrenia-spectrum disorders: a network meta-analysis of 92 randomized trials including 22,645 participants. World Psychiatry. 2022;21:295–307. https://doi.org/10.1002/wps.20972.
Ryan MC, Collins P, Thakore JH. Impaired fasting glucose tolerance in first-episode, drug-naïve patients with schizophrenia. Am J Psychiatry. 2003;160:284–9. https://doi.org/10.1176/appi.ajp.160.2.284.
Cohn TA, Remington G, Zipursky RB, Azad A, Connolly P, Wolever TM. Insulin resistance and adiponectin levels in drug-free patients with schizophrenia: a preliminary report. Can J Psychiatry. 2006;51:382–6. https://doi.org/10.1177/070674370605100608.
Fernandez-Egea E, Bernardo M, Donner T, Conget I, Parellada E, Justicia A, et al. Metabolic profile of antipsychotic-naive individuals with non-affective psychosis. Br J Psychiatry. 2009;194:434–8. https://doi.org/10.1192/bjp.bp.108.052605.
Anjum S, Bathla M, Panchal S, Singh GP, Singh M. Metabolic syndrome in drug naïve schizophrenic patients. Diabetes Metab Syndr. 2018;12:135–40. https://doi.org/10.1016/j.dsx.2017.11.006.
Verma SK, Subramaniam M, Liew A, Poon LY. Metabolic risk factors in drug-naive patients with first-episode psychosis. J Clin Psychiatry. 2009;70:997–1000. https://doi.org/10.4088/JCP.08m04508.
Kirkpatrick B, Miller BJ, Garcia-Rizo C, Fernandez-Egea E, Bernardo M. Is abnormal glucose tolerance in antipsychotic-naive patients with nonaffective psychosis confounded by poor health habits? Schizophr Bull. 2012;38:280–4. https://doi.org/10.1093/schbul/sbq058.
Saddichha S, Manjunatha N, Ameen S, Akhtar S. Diabetes and schizophrenia: effect of disease or drug? Results from a randomized, double-blind, controlled prospective study in first-episode schizophrenia. Acta Psychiatr Scand. 2008;117:342–7. https://doi.org/10.1111/j.1600-0447.2008.01158.x.
Henderson DC, Vincenzi B, Andrea NV, Ulloa M, Copeland PM. Pathophysiological mechanisms of increased cardiometabolic risk in people with schizophrenia and other severe mental illnesses. Lancet Psychiatry. 2015;2(5):452–64. https://doi.org/10.1016/S2215-0366(15)00115-7.
Houseknecht KL, Robertson AS, Zavadoski W, Gibbs EM, Johnson DE, Rollema H. Acute effects of atypical antipsychotics on whole-body insulin resistance in rats: implications for adverse metabolic effects. Neuropsychopharmacol. 2007;32(2):289–97. https://doi.org/10.1038/sj.npp.1301209.
Newcomer JW, Haupt DW, Fucetola R, Melson AK, Schweiger JA, Cooper BP, et al. Abnormalities in glucose regulation during antipsychotic treatment in schizophrenia. Arch Gen Psychiatry. 2002;59:337–45. https://doi.org/10.1001/archpsyc.59.4.337.
Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425–48. https://doi.org/10.1146/annurev-clinpsy-032813-153657.
Koblan KS, Kent J, Hopkins SC, Krystal JH, Cheng H, Goldman R, et al. A non-D2-receptor-binding drug for the treatment of schizophrenia. N Engl J Med. 2020;382:1497–506. https://doi.org/10.1056/NEJMoa1911772.
Dedic N, Dworak H, Zeni C, Rutigliano G, Howes OD. Therapeutic potential of TAAR1 agonists in schizophrenia: evidence from preclinical models and clinical studies. Int J Mol Sci. 2021;22:13185. https://doi.org/10.3390/ijms222413185.
Brown EG, Wood L, Wood S. The medical dictionary for regulatory activities (MedDRA). Drug Saf. 1999;20:109–17. https://doi.org/10.2165/00002018-199920020-00002.
Bousquet C, Lagier G, Lillo-Le Louët A, Le Beller C, Venot A, Jaulent MC. Appraisal of the MedDRA conceptual structure for describing and grouping adverse drug reactions. Drug Saf. 2005;28:19–34. https://doi.org/10.2165/00002018-200528010-00002.
Hopkins SC, Ogirala A, Worden M, Koblan KS. Depicting safety profile of the TAAR1 agonist ulotaront relative to reactions anticipated for a dopamine D2-based pharmacological class in FAERS. Clin Drug Investig. 2021;41:1067–73. https://doi.org/10.1007/s40261-021-01094-7.
Kuntz RE, Antman EM, Califf RM, Ingelfinger JR, Krumholz HM, Ommaya A, et al. Individual patient-level data sharing for continuous learning: a strategy for trial data sharing. NAM Perspect. 2019. https://doi.org/10.31478/201906b.
A double-blind, placebo-controlled study of risperidone in children and adolescents with autistic disorder. https://yoda.yale.edu/sites/default/files/ris-usa-150_csr_synopsis.pdf. Accessed 14 Oct 2022.
A randomized, double-blind, placebo-controlled clinical study of the efficacy and safety of risperidone for the treatment of schizophrenia in adolescents. https://yoda.yale.edu/sites/default/files/nct00088075.pdf. Accessed 14 Oct 2022.
The efficacy and safety of risperidone in adolescents with schizophrenia: a comparison of two dose ranges of risperidone. https://yoda.yale.edu/sites/default/files/nct00034749.pdf. Accessed 14 Oct 2022.
Efficacy and safety of a flexible dose of risperidone versus placebo in the treatment of psychosis of Alzheimer’s disease. https://yoda.yale.edu/sites/default/files/ris-int-83_csr_synopsis.pdf. Accessed 14 Oct 2022.
Efficacy and safety of a flexible dose of risperidone versus placebo in the treatment of psychosis of Alzheimer’s disease. https://yoda.yale.edu/sites/default/files/nct00034762.pdf. Accessed 14 Oct 2022.
A randomized, double-blind, placebo-controlled study to explore the efficacy and safety of risperidone long-acting intramuscular injectable in the prevention of mood episodes in bipolar I disorder, with open-label extension. https://yoda.yale.edu/sites/default/files/nct00132678.pdf. Accessed 14 Oct 2022.
A randomized, double-blind, placebo- and active-controlled, parallel-group study to evaluate the efficacy and safety of risperidone long-acting injectable for the prevention of mood episodes in the treatment of subjects with bipolar I disorder. https://yoda.yale.edu/sites/default/files/nct00391222.pdf. Accessed 14 Oct 2022.
The efficacy and safety of flexible dose ranges of risperidone versus placebo or haloperidol in the treatment of manic episodes associated with bipolar I disorder. https://yoda.yale.edu/sites/default/files/nct00253162.pdf. Accessed 14 Oct 2022.
The safety and efficacy of risperdal (risperidone) versus placebo versus haloperidol as add-on therapy to mood stabilizers in the treatment of the manic phase of bipolar disorder. https://yoda.yale.edu/sites/default/files/nct00253149.pdf. Accessed 14 Oct 2022.
A Canadian multicenter placebo-controlled study of fixed doses of risperidone and haloperidol in the treatment of chronic schizophrenic patients. https://yoda.yale.edu/sites/default/files/nct00249132.pdf. Accessed 14 Oct 2022.
Risperidone depot (microspheres) in the treatment of subjects with schizophrenia or schizoaffective disorder: an open-label follow-up trial of RIS-INT-62 and RIS-INT-85. yoda.yale.edu/sites/default/files/nct00495118.pdf. Accessed 14 Oct 2022.
CONSTATRE: Risperdal® Consta® trial of relapse prevention and effectiveness. https://yoda.yale.edu/sites/default/files/nct00216476.pdf. Accessed 14 Oct 2022.
Early versus late initiation of treatment with Risperdal Consta in subjects with schizophrenia after an acute episode: CSR summary not yet available. https://yoda.yale.edu/nct00216671-early-versus-late-initiation-treatment-risperdal-consta-subjects-schizophrenia-after. Accessed 14 Oct 2022.
Risperidone depot (microspheres) in the treatment of subjects with schizophrenia or schizoaffective disorder: an open-label follow-up trial of RIS-INT-62 and RIS-INT-85. https://yoda.yale.edu/sites/default/files/nct00495118.pdf. Accessed 14 Oct 2022.
Risperidone versus haloperidol versus placebo in the treatment of schizophrenia. https://yoda.yale.edu/sites/default/files/ris-usa-1_csr_synopsis.pdf. Accessed 14 Oct 2022.
The safety and efficacy of risperidone 8 mg qd and 4 mg qd compared to placebo in the treatment of schizophrenia. yoda.yale.edu/sites/default/files/ris-usa-72_csr_synopsis.pdf. Accessed 14 Oct 2022.
Acknowledgements
This study, carried out under YODA Project 2021-4575, used data obtained from the Yale University Open Data Access Project, which has an agreement with Janssen Research & Development, LLC. The interpretation and reporting of research using this data are solely the responsibility of the authors and does not necessarily represent the official views of the Yale University Open Data Access Project or Janssen Research & Development, LLC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Authors’ Contributions
SCH: conceptualization, writing, and methodology; AO: methodology, formal analysis, and data curation; MAW: validation, resources, and writing; and KSK: conceptualization and writing.
Funding
This study was funded by Sunovion Pharmaceuticals Inc.
Conflicts of interest
Seth C. Hopkins, Ajay Ogirala, Courtney Zeni, Mary Alice Worden, and Kenneth S. Koblan are employees of Sunovion Pharmaceuticals Inc.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The datasets analyzed in the current study are available from the Yale University Open Data Access (YODA) project. The data are available upon appropriate request filed with Yale University, 25 Science Park-3rd Floor, 150 Munson St, New Haven, CT 06511, USA.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hopkins, S.C., Ogirala, A., Zeni, C. et al. Depicting Risperidone Safety Profiles in Clinical Trials Across Different Diagnoses Using a Dopamine D2-Based Pharmacological Class Effect Query Defined by FAERS. Clin Drug Investig 42, 1113–1121 (2022). https://doi.org/10.1007/s40261-022-01218-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-022-01218-7