Abstract
Background
Mirabegron is a human β3-adrenoceptor agonist for the treatment of overactive bladder. The pharmacokinetic profile of mirabegron has been extensively characterized in healthy Caucasian subjects.
Objective
The objective of this study was to evaluate the pharmacokinetics, dose-proportionality, and tolerability of mirabegron following single and multiple oral doses in healthy Japanese male subjects. The results were compared with those reported in non-Japanese (primarily Caucasian) subjects.
Methods
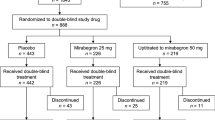
Two studies were conducted. In a single-blind, randomized, placebo-controlled, parallel-group, single- and multiple-ascending dose study (Study 1), mirabegron oral controlled absorption system (OCAS) tablets were administered at single doses of 50, 100, 200, 300, and 400 mg, with eight subjects (six active, two placebo) per dose group (Part I), and once daily for 7 days at 100 and 200 mg with 12 subjects (eight active, four placebo) per group (Part II). In an open-label, three-period, single-ascending dose study (Study 2), mirabegron OCAS was administered to 12 subjects at 25, 50, and 100 mg in an intra-subject dose-escalation design. Plasma and/or urine samples were collected up to 72 h after the first and last dose and analyzed for mirabegron. Pharmacokinetic parameters were determined using non-compartmental methods. Tolerability assessments included physical examinations, vital signs, 12-lead electrocardiogram, clinical laboratory tests (biochemistry, hematology, and urinalysis), and adverse event (AE) monitoring.
Results
Forty and 24 young male subjects completed Part I and II, respectively, of Study 1. Twelve young males completed Study 2. After single oral doses (25–400 mg), maximum plasma concentrations (C max) were reached at approximately 2.8–4.0 h postdose. Plasma exposure (C max and area under the plasma concentration–time curve) of mirabegron increased more than dose proportionally at single doses of 25–100 mg and approximately dose proportionally at high doses of 300 and 400 mg. A more than dose proportional increase in plasma exposure was noted in the body of the same individual. Mirabegron accumulated twofold upon once-daily dosing relative to single-dose data. Steady state was reached within 7 days. Mirabegron was generally well-tolerated at single doses up to 400 mg and multiple doses up to 200 mg. The AE with the highest incidence was increased pulse rate at 400 mg in Study 1.
Conclusions
Mirabegron OCAS exhibits similar single- and multiple-dose pharmacokinetic characteristics and deviations from dose proportionality in healthy Japanese male subjects compared with those observed in non-Japanese (primarily Caucasian) subjects in previous studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Mirabegron is an agonist of the human β3-adrenoceptor, discovered by Astellas Pharma Inc. in Japan [1]. β3-Adrenoceptors have been shown to play a role in the relaxation of the urinary bladder detrusor smooth muscle [2]. Mirabegron relaxes the detrusor smooth muscle during the storage phase of the urinary bladder fill-void cycle by activation of β3-adrenoceptor, which increases bladder capacity [1, 3]. Mirabegron has been approved in Japan, the USA, and the EU for the treatment of overactive bladder (OAB) [4, 5] and is the first of a new class of oral compounds with a different mode of action than antimuscarinic medications, the current mainstay treatment for patients with OAB [6].
The pharmacokinetic profile of mirabegron after single and multiple oral doses has been reported in cohorts of Western, primarily Caucasian, healthy adult subjects [7, 8]. Mirabegron demonstrated a greater than dose-proportional increase in maximum plasma concentration (C max) and area under the plasma concentration–time curve (AUC) after single and multiple oral doses, which was due to an increase in absolute bioavailability with increasing dose (from 25 % at 25 mg to 40 % at 100 mg) [7, 8]. Mirabegron was cleared by multiple mechanisms (renal and possibly biliary excretion of unchanged drug, and metabolism by multiple enzymes), with no single predominating clearance pathway [9]. In vitro studies suggested a role for the polymorphic cytochrome P450 (CYP) 2D6 enzyme in the oxidative metabolism of mirabegron, in addition to CYP3A [10], although in vivo results indicated that these isozymes play a limited role in the overall elimination [11, 12]. In addition, body weight is an important consideration when comparing different ethnic populations, as body weight has been shown to affect mirabegron pharmacokinetics [8].
As part of the clinical development program in Japan, we conducted two studies using single doses of mirabegron 25–400 mg and multiple doses of 100 and 200 mg/day in healthy Japanese male subjects to evaluate the pharmacokinetics, dose-proportionality, and tolerability of mirabegron after single and multiple oral doses. The pharmacokinetic results obtained in Japanese subjects in these studies were subsequently compared with those previously reported for non-Japanese (primarily Caucasian) healthy male subjects.
2 Methods
Both studies were conducted in accordance with the ethical principles based on the Declaration of Helsinki [13] and Good Clinical Practice [14], as defined by the Ministerial Ordinance concerning the standards for the implementation of clinical studies on pharmaceutical products, and the regulations stipulated in the Japanese Pharmaceutical Affairs Law. The studies were conducted at two centers and approved by institutional review boards.
2.1 Subjects
Subjects were eligible for inclusion in the studies if they met the following criteria: for Study 1, males aged 20–44 years inclusive, with a body weight of 50.0 to <80.0 kg and a body mass index (BMI) of 18.5 to <25.0 kg/m2; for Study 2, males aged 20–44 years inclusive, with a body weight of 50.0 to <80.0 kg and a BMI of 17.6 to <26.4 kg/m2. Major exclusion criteria for both studies were current or previous hepatic, renal, heart, respiratory, or gastrointestinal disease or cerebrovascular disorder; concurrent or previous malignant tumor; upper gastrointestinal disease within 7 days prior to the start of the study (Study 2 only); any clinically significant deviation from normal in physical examination, vital signs, electrocardiogram (ECG) or clinical laboratory determinations; history of drug allergy; history of hypersensitivity to β-adrenoceptor agonists or exposure to study drug (Study 2 only); prior exposure to long-term medication (at least 28 days; Study 1 only), any investigational drug within 120 days, or prescription or over-the-counter medications within 1 week prior to the start of the study. In both studies, concomitant medication was not allowed throughout the duration of the study. All subjects provided written informed consent before screening.
2.2 Study Designs
Study 1 was a single-blind, randomized, placebo-controlled, parallel group, single- and multiple-dose escalation study in 64 healthy male subjects to assess the single- and multiple dose pharmacokinetics and tolerability of mirabegron, formulated as a sustained release tablet using the oral controlled absorption system (OCAS) technology [15]. The study consisted of two parts. In Part I, each subject received a single oral dose of mirabegron [50, 100, 200, 300 (as 100 + 200 mg tablet), or 400 mg (as 2 × 200 mg tablet)] or matching placebo (n = 6 active, n = 2 placebo) with 200 mL of water. Subjects were fasted overnight prior to dosing and remained fasted until 4 h postdose. In Part II, each subject received a single oral dose of mirabegron (100 or 200 mg) or matching placebo (n = 8 active, n = 4 placebo) with 200 mL of water, followed by a 2-day washout period and once-daily oral doses for 7 days (Days 4–10). Dosing occurred within 30 min to 1 h after breakfast and no additional food was served until 4 h postdose. Subjects were admitted to the clinical site on the day before dosing (Day −1) and were confined until discharge on Day 4 (Part I) or Day 13 (Part II). Subjects underwent a post-study visit 4 days after the last administration or after early discontinuation.
Study 2 was a single-dose, open-label, three-period, intra-subject dose-escalation study in 12 healthy male subjects to assess the dose proportionality of the mirabegron OCAS. Each subject received escalating single doses of mirabegron 25, 50 and 100 (as 2 × 50 mg tablet) mg with 150 mL of water in three separate treatment periods, with a washout period of at least 12 days between treatments. Subjects were fasted overnight prior to dosing and remained fasted until 4 h postdose. Subjects were admitted to the clinical site on the day before dosing (Day −1) and were confined until discharge on Day 4 of each treatment period. Subjects underwent a post-study visit within 13–17 days after the last administration or after early discontinuation.
2.3 Sample Collection and Analysis
In Study 1, blood samples for plasma mirabegron concentrations were collected into tubes containing sodium-EDTA as anticoagulant and sodium fluoride as stabilizer at predose and 0.5, 1, 2, 3, 4, 5, 6, 8, 10, 12, 14, 24, 36, 48, and 72 h postdose in Part I, and at predose and 0.5, 1, 2, 3, 4, 5, 6, 8, 10, 12, 14, 24, 36, 48, and 72 h postdose on Days 1 and 10, and predose on Days 5, 6, 7, 8, and 9 of Part II. In Study 2, blood samples for plasma mirabegron concentrations were collected into tubes containing sodium-heparin as anticoagulant and sodium fluoride as stabilizer at predose and at 0.5, 1, 2, 3, 4, 5, 6, 8, 10, 12, 14, 24, 36, 48, and 72 h postdose in all periods. In Part I and Part II (Days 1 and 10) of Study 1, urine samples for measurement of unchanged mirabegron were collected within 12 h prior to dosing (Part I and Day 1 of Part II) and from 0 to 12, 12 to 24, 24 to 36, 36 to 48, and 48 to 72 h postdose.
Plasma was collected by centrifugation and plasma and urine samples were stored at −65 °C or below and −20 °C or below, respectively, until analysis. Liquid–liquid extraction was used to extract mirabegron from plasma constituents. Urine samples were diluted prior to analysis. Samples were assayed by validated liquid chromatography analytical methods coupled with tandem mass spectrometric detection (LC–MS/MS) using an atmospheric pressure chemical ionization interface, as described previously with minor modifications [16]. The calibration ranges were 1.0–500 ng/mL in plasma and 2.0–1,000 ng/mL in urine for Study 1, and 0.2–100 ng/mL in plasma for Study 2. In the bioanalytical method validation studies, within-run precision of quality control (QC) standards was less than 5.8 % for plasma and less than 7.2 % for urine. The within-run accuracy (relative error) of the assays over the QC range ranged from −5.0 to 10.0 % for plasma and from −6.9 to 13.0 % for urine.
2.4 Pharmacokinetic Analysis
Concentration data of mirabegron in plasma and urine were analyzed by non-compartmental methods using SAS® version 8.2 (SAS Institute, Cary, NC, USA), or WinNonlin Professional® version 5.0.1 (Study 1) or 5.2.1 (Study 2) (CERTARA, St. Louis, MO, USA). The following pharmacokinetic parameters were obtained as applicable and as appropriate for each study [17]: C max; time to reach C max (t max); AUC (obtained by the linear-logarithmic trapezoidal method) from time zero to 24 h (AUC24) and AUC from time zero to infinity (AUC∞) after single-dose administration, and AUC during a dosage interval (AUCτ); terminal elimination half-life (t ½β); apparent total body clearance from plasma after oral administration (CL/F); apparent volume of distribution during terminal phase after non-intravenous administration (V z/F); cumulative percentage of unchanged drug excreted into the urine (Ae%) up to 72 h postdose; and renal clearance (CLR). Actual sampling times were used in all calculations involving sampling times, and nominal sampling times were used for the mean concentration–time figures.
2.5 Tolerability Assessments
Tolerability was assessed based on physical examinations, vital signs (axillary body temperature, supine blood pressure, and supine pulse rate), resting 12-lead ECGs, standard clinical laboratory tests (hematology, blood biochemistry, urinalysis), and adverse event (AE) monitoring. Clinically significant adverse changes in any tolerability assessment, including symptoms and signs, vital signs, ECGs, and clinical laboratory tests, were considered AEs. AEs were collected from the time of dosing until the end of the study. The causal relationships for all AEs were categorized by the investigator as probable, possible, or not related.
2.6 Statistical Methods
Tolerability data were evaluated descriptively, and AEs were described in their entirety. All randomized subjects who received at least one dose of study drug were included in the tolerability analyses. Summary statistics were calculated for all pharmacokinetic parameters by dose. All subjects who received at least one dose of study drug and had at least one mirabegron plasma concentration measured were included in the pharmacokinetic analysis.
In both studies, dose-proportionality was examined for natural log transformed C max and AUC∞ using a power model [18]. The following model was used: ln(pharmacokinetic parameter) = β0 + β1·ln(dose), where β0 is the intercept and β1 is the slope of the model. Dose proportionality was concluded if the 95 % confidence interval (CI) for β1 included 1 [19]. To assess accumulation of mirabegron with multiple dosing (Study 1), 90 % CIs around the geometric mean ratio (GMR) of mirabegron C max and AUCτ on Day 10 versus C max and AUC24 on Day 1 were constructed. To evaluate if mirabegron demonstrates linear pharmacokinetics with time during repeated administration, 90 % CIs around the GMR for mirabegron AUCτ on Day 10 versus AUC∞ on Day 1 were constructed. For linear pharmacokinetics with time, the AUCτ at steady state is equal to the AUC∞ following a single dose (i.e., a ratio of 1) [20]. The MIXED procedure of SAS® version 8.2 was used for all statistical analyses, with subjects as a random effect in Study 2.
3 Results
3.1 Study Population
The disposition of the subjects in Study 1 and their characteristics are summarized in Table 1. A total of 64 healthy male subjects (40 in Part I and 24 in Part II) were randomized to study treatment and all completed the study. In Study 2, 12 healthy male subjects were enrolled and all completed the study. Their mean age was 29.7 years (range 22–37), with a mean body weight of 59.8 kg (range 54.9–73.1) and a mean BMI of 21.1 kg/m2 (range 19.2–23.4). In both studies, none of the subjects received a concomitant medication during the treatment periods.
3.2 Pharmacokinetics of Mirabegron
3.2.1 Single Dose
The mean plasma concentrations of mirabegron for 72 h after single oral doses of 50–400 mg in Study 1 Part I and 25–100 mg mirabegron in Study 2 are shown in Fig. 1. A summary of the pharmacokinetic parameters is shown in Table 2. Following single-dose administration of mirabegron 25–400 mg in the fasting state, mean t max values ranged from 2.8 to 4.0 h postdose across the tested dose range (Table 2). After reaching t max, mirabegron plasma concentrations exhibited an apparent biphasic decline, with a mean t ½β ranging from 23.9 to 36.4 h in Study 1, and 28.6 to 32.9 h in Study 2. In both studies, mirabegron C max and AUC∞ increased more than proportionally with dose (Figs. 2, 3). For Study 2 (25–100 mg), the mean estimates of the parameter β1 in the power model were 1.501 for ln(C max) (95 % CI 1.146–1.856) and 1.342 for ln(AUC∞) (95 % CI 1.102–1.583). Neither of the CIs included 1, indicating a non-proportional increase in exposure with increasing dose. These slope estimates result in a predicted 2.8-fold increase in C max and a 2.5-fold increase in AUC∞ for every twofold increase in dose within the range of 25–100 mg. Similar estimates for β1 were obtained in Study 1 Part I (50–400 mg), with mean estimates for β1 of 1.501 (95 % CI 1.222–1.781) for C max and 1.260 (95 % CI 1.120–1.400) for AUC∞. However, visual assessment of scatter plots of dose-adjusted C max and AUC∞ (Fig. 2) suggests a more than dose-proportional increase in mirabegron C max and AUC∞ in the 50 and 100 mg doses, but a dose-dependent increase at high doses, i.e., in the 300 and 400 mg groups. In both studies, mean estimates of CL/F and V z/F decreased with increasing dose, whereas t max and t ½β were independent of dose across the tested dose range. In Study 1 Part I, Ae% was dose-dependent with mean values ranging from 7.20 % after 50 mg to 14.6 % after 300 mg. CLR appeared to show no dose dependency, with mean values ranging from 9.91 to 15.2 L/h.
Dose-normalized AUC∞ (a) and C max (b) after single oral administration of mirabegron oral controlled absorption system 50, 100, 200, 300 and 400 mg in healthy male subjects in Study 1 Part I. Individual data are presented. AUC ∞ area under the plasma concentration–time curve from time zero to infinity, C max maximum plasma concentration
Dose-normalized AUC∞ (a) and C max (b) after single oral administration of mirabegron oral controlled absorption system 25, 50, and 100 mg in healthy male subjects in Study 2. Individual data are presented. AUC ∞ area under the plasma concentration–time curve from time zero to infinity, C max maximum plasma concentration
3.2.2 Multiple Dose
Mean plasma concentrations after single doses (Day 1) and multiple doses (Days 4–10) of mirabegron 100 and 200 mg in Study 1 are shown in Fig. 4. A summary of the pharmacokinetic parameters of mirabegron on Days 1 and 10 in Study 1 is shown in Table 3. After multiple doses of 100 and 200 mg, mirabegron plasma concentrations were visually assessed to be at steady state within 7 days (Fig. 4). The GMR of AUCτ on Day 10 to AUC24 on Day 1 was 2.12 (90 % CI 1.74–2.58) in the 100 mg group and 1.75 (90 % CI 1.44–2.14) in the 200 mg group, indicating that mirabegron accumulates approximately twofold with once-daily dosing. The GMR for C max was 1.55 and 0.91 on Day 10 compared with Day 1 for the 100 and 200 mg dose, respectively. The GMR of AUCτ on Day 10 to AUC∞ on Day 1 was 1.28 (90 % CI 1.08–1.52) in the 100 mg group and 1.18 (90 % CI 0.99–1.40) in the 200 mg group. The CI for the 100 mg dose did not include 1, suggesting that mirabegron exhibits non-linear pharmacokinetics over time at a 100 mg but not a 200 mg dose. Consistent with these results, the mean CL/F decreased with repeat dosing compared with single-dose administration. Mean values for t max, t ½β, and CLR were similar between Days 10 and 1, indicating that there were no obvious changes in the elimination and CLR of mirabegron.
3.3 Tolerability
In Study 1 Part I, 12 AEs were reported by eight (20 %) of the 40 subjects, and nine of these were considered by the investigator to be related to study drug. The AEs were all mild in intensity and occurred in one (17 %), three (50 %), and four (67 %) subjects in the 100, 300, and 400 mg groups, respectively. No AEs were observed in the placebo, 50 or 200 mg groups. The most common AEs (reported by ≥2 subjects) were increased pulse rate and increased blood amylase. Pulse rates exceeding 100 beats/min at 4–6 h after dosing occurred in three of six subjects in the 400 mg group. One of these three subjects with increased heart rate also developed palpitations at 3 h after dosing. There were no episodes of clinically significant increases in pulse rate or palpitations in other dose groups. Pulse rate tended to increase in a dose-dependent manner at 6 h postdose in the 200 mg and higher dose groups compared with the placebo group. Increases in blood amylase that were considered AEs by the investigator, occurred in two of six subjects in the 300 mg group and one of six subjects in the 100 mg group. In Part II, eight AEs were reported by five (21 %) of the 24 subjects, and two of these were considered by the investigator to be related to study drug. The AEs occurred in two (25 %), two (25 %), and one (12.5 %) subjects in the placebo, 100, and 200 mg groups, respectively. All AEs were mild in intensity and reported by one subject each. Increases in pulse rate were observed at 6 h after the first administration in the 200 mg group and at 6 h after the last administration in the 100 and 200 mg groups as compared with the placebo group. None of the pulse rate increases were judged clinically significant by the investigator. There were no clinically significant changes in blood pressure, body temperature, 12-lead ECG, or physical examination results.
In Study 2, there were six AEs reported by four (33 %) of the 12 subjects, and five of these were considered by the investigator to be related to study drug. Of the six AEs, two and four events occurred in two and three subjects receiving a 25 and 50 mg dose, respectively. All were mild in intensity and reported by one subject each. Mean supine pulse rate at 6 h postdose appeared to show a dose-dependent increase. Mean systolic blood pressure tended to increase at 3–6 h postdose; however, it was considered to be due to circadian rhythm. There were no apparent changes in mean diastolic blood pressures and no clinically significant findings in ECG data. No deaths, serious AEs, or AEs requiring symptomatic therapy occurred in either study. All AEs resolved spontaneously.
4 Discussion
In these studies in healthy Japanese male subjects, mirabegron C max were reached on average within 2.8–4.0 h following single-dose oral administration and at 5.0 h following multiple-dose administration. Steady-state conditions were reached by 7 days of once-daily administration with mirabegron, and accumulation of mirabegron was about twofold. These findings are in accordance with previously published single- and multiple-dose studies in healthy non-Japanese individuals, which mainly comprised Caucasians (60–100 %) [7, 8]. The mean t ½β of mirabegron (25.1–36.4 h) was consistent with the range observed in non-Japanese males following single- (27.9–40.6 h) and multiple-dose administration (29.2–36.8 h) in those previous studies that used a similar sampling duration (up to 72 or 96 h postdose) as the present studies [7, 8].
A greater than dose-proportional increase in exposure was observed following single-dose administration across the 25–100 mg dose range, resulting in a predicted 2.8- and 2.5-fold increase in mirabegron C max and AUC∞, respectively, with each doubling of the dose within this dose range. Similar deviations from dose proportionality (approximately 3.0-fold for C max and 2.7-fold for AUC∞) were observed in a single-dose pharmacokinetics study in healthy non-Japanese male subjects using the same dose range [7]. Above 100 mg, the dose non-proportionality was much less marked as the normalized AUC–dose relationship began to reach a maximum. A postulated mechanism for the non-proportionality of mirabegron pharmacokinetics after oral administration is the decrease in the action of gut efflux transporters (predominantly P-glycoprotein) with increasing doses that reduce the bioavailability of mirabegron [21]. The efflux ability of these transporters may be saturated at higher doses (above 100 mg), resulting in a return to dose proportionality.
A small increase (28 % at 100 mg and 18 % at 200 mg) in AUCτ at steady state compared with first-dose AUC∞ was observed, suggesting that mirabegron may exhibit non-linear pharmacokinetics over time (i.e., an increase in bioavailability and/or a decrease in clearance with time) at these doses. Similar deviations from linear pharmacokinetics (ranging from a 6 % increase at 100 mg to 38 % increase at 300 mg) were observed in a multiple-dose pharmacokinetics study in healthy non-Japanese individuals [8]. As mirabegron exhibited linear pharmacokinetics with time at a clinically relevant dose of 50 mg [8], the clinical meaningfulness of the finding is likely to be limited.
A retrospective comparison of mirabegron exposure in Japanese and non-Japanese (primarily Caucasian) healthy men was conducted. Only single-dose data at 25, 50, 100, and 200 mg from Study 1 Part I and Study 2 were used for the comparison, as these were generated under similar food conditions (i.e., after an overnight fast) as those obtained in the non-Japanese subjects. The comparison revealed that mean C max values for mirabegron in Japanese male subjects at the lower dose levels (25, 50, and 100 mg) were higher than those observed in previous studies at the same dose level in non-Japanese male individuals (Table 4). Differences ranged from approximately 32 % at 25 mg to 58 % at 100 mg. For mean C max at 200 mg and mean AUC∞ at all evaluated dose levels, values were generally comparable or only slightly higher in Japanese subjects. The apparent differences in mean mirabegron C max and, to a lesser extent, AUC∞ between Japanese and non-Japanese individuals most likely reflect the variability in C max and AUC∞ observed within and across studies of mirabegron pharmacokinetics, and the small sample size in the present and previous studies. In addition, the differences are attributable in part to differences in body weight (mean weight ranging from 58.8 to 64.5 kg in Japanese subjects vs. 80.0 to 83.5 kg in non-Japanese subjects) (Table 4). The differences in mirabegron C max were smaller when values were normalized for body weight (Table 4). Such weight-based trends have been observed in previous studies with mirabegron. Correction for body weight nearly completely eliminated differences in mirabegron exposure between healthy men and women after intravenous administration [7], and markedly reduced sex differences in exposure after single- and multiple-dose oral administration [7, 8].
Mirabegron was well-tolerated in healthy Japanese subjects. No serious AEs or discontinuations as a result of AEs were reported at any dose of mirabegron administered in either study. These tolerability findings are consistent with single- and multiple-dose studies conducted in non-Japanese, predominantly Caucasian, healthy subjects at single doses of mirabegron up to 300 mg or multiple daily doses of up to 300 mg [7, 8]. The most common AEs were increased pulse rate in Study 1, and the pulse rate tended to increase dose dependently. These trends are reported by Krauwinkel et al. [8].
5 Conclusions
Mirabegron exhibited a greater than dose-proportional increase in exposure after single and multiple oral doses of mirabegron OCAS in healthy Japanese male subjects. Steady-state conditions were reached by 7 days of once-daily administration, and accumulation of mirabegron was about twofold. The single- and multiple-dose pharmacokinetic characteristics and deviations from dose proportionality in healthy Japanese male subjects were similar to those observed in non-Japanese (primarily Caucasian) subjects in previous studies.
References
Takasu T, Ukai M, Sato S, et al. Effect of (R)-2-(2-aminothiazol-4-yl)-4’-{2-[(2-hydroxy-2-phenylethyl)amino]ethyl} acetanilide (YM178), a novel selective β3-adrenoceptor agonist, on bladder function. J Pharmacol Exp Ther. 2007;321:642–7.
Yamaguchi O. β3-adrenoceptors in human detrusor muscle. Urology. 2002;59:25–9.
Yamaguchi O, Chapple CR. β3-adrenoceptors in urinary bladder. Neurourol Urodyn. 2007;26:752–6.
Astellas Pharma. Betanis tablets Japanese prescribing information. July 2011.http://www.info.pmda.go.jp/shinyaku/P201100119/80012600_22300AMX00592_A100_1.pdf. Accessed 29 Oct 2013
Astellas Pharma US Inc. Myrbetriq United States prescribing information. June 2012. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.Set_Current_Drug&ApplNo=202611&DrugName=MYRBETRIQ&ActiveIngred=MIRABEGRON&SponsorApplicant=APGDI&ProductMktStatus=1&goto=Search.Label_ApprovalHistory. Accessed 29 Oct 2013
Athanasopoulos A, Giannitsas K. An overview of the clinical use of antimuscarinics in the treatment of overactive bladder. Adv Urol. 2011;2011:820816
Eltink C, Lee J, Schaddelee M, et al. Single dose pharmacokinetics and absolute bioavailability of mirabegron, β3-adrenoceptor agonist for treatment of overactive bladder. Int J Clin Pharm Ther. 2012;50:838–49.
Krauwinkel W, Van Dijk J, Schaddelee M, et al. Pharmacokinetic properties of mirabegron, a β3-adrenoceptor agonist: results from two phase I, randomized, multiple-dose studies in healthy young and elderly men and women. Clin Ther. 2012;34:2144–60.
Takusagawa S, van Lier JJ, Suzuki K, et al. Absorption, metabolism and excretion of [14C]mirabegron (YM178), a potent and selective β3-adrenoceptor agonist, after oral administration to healthy male volunteers. Drug Metab Dispos. 2012;40:815–24.
Takusagawa S, Yajima K, Miyashita A, et al. Identification of human cytochrome P450 isoforms and esterases involved in the metabolism of mirabegron, a potent and selective β3-adrenoceptor agonist. Xenobiotica. 2012;42:957–67.
van Gelderen E, Li Q, Meijer J, et al. An exploratory comparison of the single dose pharmacokinetics of the β3-adrenoceptor agonist mirabegron in healthy CYP2D6 poor and extensive metabolizers. Clin Pharmacol Ther. 2009;85(Suppl 1):S88.
Sawamoto T, Lee J, Alak A, et al. Phase I, open-label, drug interaction study to evaluate the effect of multiple doses of ketoconazole on single dose mirabegron (YM178) oral controlled absorption system (OCAS) in healthy adult subjects. Clin Pharmacol Ther 2011; 89(Suppl. 1):S21.
World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Adopted by the 18th WMA General assembly and amended by 48th WMA General Assembly, Somerset West, South Africa, October 1996. http://www.wma.net/en/30publications/10policies/b3/. Accessed 29 Oct 2013.
International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. Guideline for good clinical practice E6(R1). http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6_R1/Step4/E6_R1__Guideline.pdf. Accessed 31 July 2013
Chapple CR. The development of the oral controlled absorption system (Ocas®): a new improved formulation of tamsulosin. Eur Urol Suppl. 2005;4:1–4.
Van Teijlingen R, Meijer J, Takusagawa S, et al. Development and validation of LC-MS/MS methods for the determination of mirabegron and its metabolites in human plasma and their application to a clinical pharmacokinetic study. J Chromatogr B Analyt Technol Biomed Life Sci. 2012;887–888:102–11.
Gabrielsson J, Weiner D. Pharmacokinetic and pharmacodynamic data analysis: concepts and applications. 4th ed. Stockholm: Swedish Pharmaceutical Press; 2007.
Gough K, Hutchison M, Keene O, et al. Assessment of dose proportionality: report from the statisticians in the pharmaceutical industry/pharmacokinetics UK joint working party. Drug Inf J. 1995;29:1039–48.
Smith BP, Vandenhende FR, DeSante KA, et al. Confidence interval criteria for assessment of dose proportionality. Pharm Res. 2000;17:1278–83.
Rowland M, Tozer TN. Clinical pharmacokinetics: concepts and application. 3rd ed. Baltimore: Lippincott Williams & Wilkins; 1995.
Takusagawa S, Ushigome F, Nemoto H, et al. Intestinal absorption mechanism of mirabegron, a potent and selective β3-adrenoceptor agonist: involvement of human efflux and/or influx transport systems. Mol Pharm. 2013;10:1783–94.
Acknowledgments
The studies were sponsored by Astellas Pharma Inc. The authors thank Virginie Kerbusch, PhD (PharmAspire Consulting) for scientific writing support, for which she received financial compensation from Astellas. Drs. Tokuno, Matsushima, Katashima, Sawamoto, Takusagawa, and Van Gelderen, and Ms. Iitsuka and Amada played a substantial role in the design and overall management of the study, and the collection, analysis, and interpretation of data. Drs. Tanaka and Miyahara were involved in data collection. All authors listed were involved in the critical review and revision of the manuscript, and all provided final approval of the content.
Conflict of interest
Drs. Tokuno, Matsushima, Katashima, Sawamoto, Takusagawa, and Van Gelderen, and Ms. Iitsuka and Amada are paid employees of Astellas Pharma. Drs. Tanaka and Miyahara were the primary study investigators, for which they received financial compensation from Astellas. The authors have indicated that they have no other conflicts of interest with regard to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Iitsuka, H., Tokuno, T., Amada, Y. et al. Pharmacokinetics of Mirabegron, a β3-Adrenoceptor Agonist for Treatment of Overactive Bladder, in Healthy Japanese Male Subjects: Results from Single- and Multiple-Dose Studies. Clin Drug Investig 34, 27–35 (2014). https://doi.org/10.1007/s40261-013-0146-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-013-0146-1