Abstract
The epidemic due to severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection has been spreading globally, raising increasing concerns. This public health emergency has triggered a race to find medications to improve the prognosis of this disease. There is currently great interest in drug repositioning to manage SARS-CoV-2 infection, that is, the evaluation of the potential benefits of a drug that has already been proven safe and effective in humans for other approved indications. As interleukin-6 (IL-6) acts as a key driver of the inflammation associated with coronavirus disease 2019 (COVID-19), IL-6 and IL-6 receptor (IL-6R) inhibition appear to be promising targets for the treatment of COVID-19 patients. It is important to critically analyze the available evidence concerning the use of the available anti-IL-6 (siltuximab) and anti-IL-6R (tocilizumab and sarilumab) agents in COVID-19 patients, in terms of both benefit and risk. In this review, the pathogenesis of the cytokine storm induced by COVID-19, the role of IL-6 in this cytokine storm, the rationale for the use of anti-IL-6 agents, and key information on potential benefits and safety monitoring of these biologicals in COVID-19 patients is discussed.
Similar content being viewed by others
There is currently great interest in drug repurposing of anti-interleukin-6 (IL-6) agents for the treatment of COVID-19 patients, mostly in the advanced disease stage. |
Despite the promising effects of anti-IL-6 agents, available clinical evidence is limited and only partly present for tocilizumab. |
While waiting for more robust clinical data to support the efficacy of anti-IL-6 agents in COVID-19 patients, their potential toxicity should be carefully monitored and managed whenever clinicians decide to treat patients with these agents. |
1 Introduction
The global coronavirus disease 2019 (COVID-19) pandemic has led to 5,459,528 infected patients and 345,994 deaths worldwide between 31 December 2019 and 26 May 2020, according to the European Centre for Disease Control [1]. In the rush to search for a treatment to improve the prognosis of the disease, two contrasting currents of thoughts emerge: on the one hand are those who propose not to use medications whose risk–benefit profile has not been scientifically proven in COVID-19 patients; on the other hand are other researchers and clinicians who propose to repurpose already available treatments, due to a lack of specifically newly developed anti-severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) agents, even in the absence of robust scientific evidence, on the basis of clinical intuition or in vitro findings only [2]. Taking the most appropriate decisions in such circumstances is not easy. Despite the comprehensible pressure to rapidly offer new therapies and the difficulties in carrying out clinical trials to generate robust scientific evidence in such a short time, a stark pre-marketing evaluation of a drug’s benefit–risk profile seems to be essential to keep patients safe from ineffective and/or high-risk drugs [3]. There is currently great interest in drug repurposing of anti-interleukin-6 (IL-6) agents for the treatment of COVID-19 patients with serious lung damage and elevated IL-6 levels. Nevertheless, precise recommendations may be provided only when the results of the ongoing clinical trials of anti-IL-6 agents in COVID-19 patients are published.
In this review, the pathogenesis of COVID-19 as a rationale for anti-IL-6 use will be described. In addition, for all marketed anti-IL-6 agents, available clinical evidence of potential benefits, safety monitoring, and ongoing experimental clinical studies in COVID-19 patients will be presented and discussed.
2 Pathogenesis of COVID-19
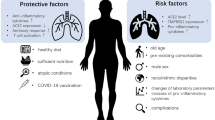
Like SARS-CoV-1, SARS-CoV-2 penetrates cells as a result of the binding of the spike glycoprotein of the viral envelope to the angiotensin-converting enzyme 2 (ACE2) host cell surface receptor [4]. ACE2 is a type I membrane protein expressed on type II pneumocytes, but it can also be found on renal, heart, gastrointestinal, and blood vessel cells [5]. Once SARS-CoV-2 penetrates a cell, viral RNA genome is released into the cytoplasm, where sub-genomic RNA transcription and the replication of viral genetic material takes place [6]. It is important to focus on the pathogenetic process because it can cause severe clinical manifestations such as acute respiratory distress syndrome (ARDS) or macrophage activation syndrome (MAS) in some patients with COVID-19 syndrome, possibly due to immunodysfunction and the uncontrolled release of pro-inflammatory cytokines and chemokines. Furthermore, higher levels of tumor necrosis factor (TNF)-α, interleukin (IL)-1, IL-10, and IL-6 have been detected in patients with severe COVID-19 [7].
The mechanisms leading to the uncontrolled release of inflammatory cytokines are still unclear, but there are at least two hypotheses. The first considers the rate of viral replication, which can cause pyroptosis (the inflammatory apoptosis of epithelial and endothelial cells), and thus trigger the release of pro-inflammatory cytokines and chemokines [8]. This apoptosis also involves macrophages and lymphocytes, and may cause peripheral lymphopenia in patients with COVID-19 syndrome [9]. Evidence indicates an alteration in innate immunity in which a pivotal role is played by INF-1, which controls viral replication and promotes adaptive immune responses. INF-1 responses to SARS-CoV and Middle East respiratory syndrome coronavirus (MERS-CoV) are suppressed because both coronaviruses have multiple strategies to interfere with the induction of the signal leading to INF-1 production [10], and this weakening of the action of INF-1 is strictly associated with the severity of the disease [11].
The second hypothesis concerns adaptive immunity and the role of neutralizing antibodies against the S protein of the virus. Animal studies of SARS-CoV have shown that the immunoglobulin Gs (IgGs) binding the viral S protein trigger a still-little-understood inflammatory process that can cause severe pulmonary lesions. Anti-S protein IgGs may facilitate the accumulation of pro-inflammatory monocytes and macrophages in the lungs by producing monocyte chemoattractant protein-1 (MCP-1) and IL-8, and this pro-inflammatory response seems to be mediated by the binding of the virus/anti-S IgG complex to Fc receptors (FcR) on the surface of monocytes/macrophages [12]. Moreover, the appearance of antiviral IgGs coincides with the onset of acute respiratory disease in 80% of patients with SARS-CoV infection [13].
The role of adaptive immunity in these circumstances cannot be entirely explained without also considering the involvement of CD8+ and CD4+ T lymphocytes, because cytotoxic CD8+ T cells (CTLs) secrete molecules such as perphorine, granzymes, and INF-γ in an attempt to eradicate the virus from host cells [14], and CD4+ helper T lymphocytes (Th) assist cytotoxic T cells and B cells by producing inflammatory cytokines [15].
However, persistent SARS-CoV stimulation can deplete T lymphocytes in such a way as to reduce their function and prevent cytokine production [16]. This may be induced by the inhibitory cytokine IL-10, which has been detected in the peripheral blood of patients with COVID-19 and, in addition to preventing the proliferation of T lymphocytes, may also promote their depletion [17].
IL-6 and TNF-α also seem to be specifically involved in CD4+ and CD8+ T-cell depletion (which leads to the lymphopenia that is frequently observed in COVID-19 patients treated in intensive care units) because their concentrations seem to be inversely proportional to the number of T lymphocytes [18]. IL-6 production can be induced by SARS-CoV-2 and stimulated by other cells of the immune system [19]. It has been shown that, during SARS-CoV-2 infection, CD4+ T lymphocytes are rapidly activated to differentiate into pathogenic Th1 cells, thus generating granulocyte-macrophage colony-stimulating factor (GM-CSF) and other pro-inflammatory cytokines that stimulate the activation of monocytes highly expressing IL-6 [20]. The complex activation of IL-6 requires the involvement of IL-6, the IL-6 receptor (IL-6R) and the gp130 co-receptor [21], but many cells that are not part of the immune system (including stromal and epithelial cells) can trigger strong inflammatory responses by means of trans-signaling when these three components attach to their membranes [22].
IL-1, a pleiotropic cytokine involved in inflammatory processes, hematopoiesis, and fibrosis [23], also plays an important role in MAS and COVID-19. The release of IL-1β depends on the activity of the NLRP3 inflammasome, a receptor of the NOD family that responds to various noxious stimuli including viral RNA [24]. Inflammasomes are large multi-molecular complexes present on innate immunity cells, and are best known for controlling the activation of caspase-1 and thus regulating the maturation of IL-1β and IL-18 [25]. It is becoming increasingly clear that NLRP3 recognizes some RNA viruses by detecting the cell damage or distress induced by their viroporins, which are pore-forming transmembrane proteins [26]. Viroporins alter cell membrane permeability to ions by forming membrane channels [27], and a recent study has shown that the E protein of SARS-CoV creates channels that are permeable to Ca2+ ions, and activates the NLRP3 inflammasome [28]. It is therefore possible that the mode of action of SARS-CoV-2 may be similar if the concentration of IL-1 is increased in patients with severe COVID-19 manifestations.
In conclusion, this alteration of the immune response leading to an uncontrolled cytokine storm, similar to the cytokine release syndrome (CRS) observed with CAR-T immunotherapy, was associated with ARDS (even fatal) in COVID-19 patients. According to these observations, CRS is the main target on which the majority of researchers are focusing, with the aim of identifying an effective treatment for critical COVID-19 patients with severe manifestations.
3 Anti-IL-6 Agents
To date, it has been demonstrated that blocking IL-6 is therapeutically effective in various diseases, such as rheumatoid arthritis and Castleman’s disease, as well as in the management of CRS following CAR T-cell infusion [29, 30]. More recently, as mentioned above, IL-6 was proven to be a key driver of the inflammation associated with COVID-19 infection [5]. As such, it has been hypothesized that monoclonal antibodies blocking IL-6 could help improve clinical outcomes in COVID-19 patients with severe pneumonia. As explained earlier, the scientific rationale to use IL-6 inhibitors is that the underlying pathophysiology of organ damage (especially lungs) is caused by an amplified immune response and cytokine release, or ‘cytokine storm’ [31], that seems to be a major driver of mortality in COVID-19.
Several IL-6 inhibitors have become available on the market for clinical use as monoclonal antibodies targeting IL-6 (siltuximab) or IL-6R (tocilizumab and sarilumab) (Fig. 1). The first approved drug is tocilizumab [32], marketed as an intravenous formulation to be dosed based on body weight and, only for rheumatological indications, a fixed-dose subcutaneous formulation. Tocilizumab has been proven to be effective either as monotherapy or in combination with disease-modifying antirheumatic drugs (DMARDs) for adult patients with moderate to severe rheumatoid arthritis [33, 34] (Online Resource 1, see electronic supplementary material [ESM]). The IL-6R blockade with tocilizumab was also used as first-line treatment for the management of CRS following CAR T-cell infusion, demonstrating high response rates [35, 36]. It has been shown that fever and tachycardia associated with CRS resolved within hours after administration of tocilizumab [37, 38]; resolution of hypotension and organ dysfunction was delayed [39]. Moreover, Alvi et al. reported that a longer lag time between CRS onset and tocilizumab administration was associated with an increase in CRS-related cardiovascular events [40]. In some cases, CRS refractory to tocilizumab therapy was also reported [41, 42]. Given the rapid clinical response to tocilizumab, it has become a mainstay therapy in CRS [43]. Data on tocilizumab for CRS treatment are still considered limited, due to a lack of randomized trials. However, the published studies describing the beneficial effects of tocilizumab on objective early endpoints (e.g., vital signs) [35, 36] provide substantial evidence for its use in life-threatening CRS.
SARS-CoV-2-induced cytokine storm and mechanism of action of anti-IL-6 and anti-IL-6R drugs. IL-6/IL-6R signaling pathway: the binding of IL-6 to its soluble (sIL-6R) and membrane-bound receptors (mIL-6R) determines their dimerization, resulting in the juxtaposing of receptor-associated JAKs. The JAKs subsequently undergo auto-phosphorylation and/or transphosphorylation on target tyrosine residues. The activation of JAKs results in the propagation of the cytokine-mediated signal and finally determines the activation of transcription factors, such as the STATs. The activated STATs dimerize and translocate to the cell nucleus to induce or suppress target genes [62]. Anti-IL-6 and anti-IL-6R agents inhibit sIL-6R and mIL-6R-mediated signaling. IL-6 interleukin 6, IL-6R interleukin 6 receptor, JAK Janus kinase, SARS-CoV-2 severe acute respiratory syndrome coronavirus-2, STAT Signal Transducer and Activator of Transcription
Other marketed anti-IL-6 agents are siltuximab, licensed for the treatment of Castleman’s disease by the European Medicine Agency (EMA) in 2014 [44], and the more recently marketed sarilumab (2017), approved for the treatment of rheumatoid arthritis (Online Resource 1, see ESM). While tocilizumab and sarilumab act on the IL-6 receptor, siltuximab binds directly to IL-6. The affinity of sarilumab for the human IL-6R is greater than that of tocilizumab, and it has a prolonged half-life; on the other hand, the overall efficacy and safety of the two anti-IL-6 agents seem to be comparable [45, 46]. Siltuximab has been less thoroughly studied in CRS treatment [47], although it has been used off-label in CRS management, especially in patients who are tocilizumab and steroid refractory [48].
IL-6 inhibition is a promising mechanistic pathway that has been explored for drug development for the treatment of a number of diseases such as type 1 diabetes mellitus, schizophrenia, solid tumors (siltuximab and tocilizumab), uveitis, and sarcoidosis (sarilumab). Several clinical trials investigating anti-IL-6 agents in those diseases are currently ongoing (as reported in ClinicalTrials.gov and EU Clinical Trials).
4 Available Clinical Evidence and Ongoing Clinical Studies on Anti-IL-6 Agents for COVID-19 Treatment
To date, evidence on beneficial effects of tocilizumab are derived from observational studies and case reports only, as summarized below. No published data regarding sarilumab and siltuximab in COVID-19 patients is yet available.
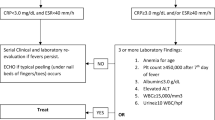
A retrospective study conducted in China recruited 21 patients diagnosed with severe or critical COVID-19 and treated with tocilizumab 400 mg once through intravenous infusion, in addition to the standard care, including lopinavir and methylprednisolone. The diagnosis was considered severe if any of the following conditions was met: (i) respiratory rate ≥ 30 breaths/min; (ii) oxygen saturation ≤ 93%; (iii) PaO2/FiO2 ≤ 300 mmHg. The diagnosis was considered critical if any of the following conditions was met: (i) respiratory failure requiring mechanical ventilation; (ii) shock; (iii) other organ failure necessitating admission to intensive care unit (ICU). The authors reported that the body temperature of all patients returned to normal values within the first day after receiving tocilizumab, remaining stable thereafter. Within the fifth day of treatment, 75% of patients had a reduced need for oxygen supplementation and one patient needed no oxygen therapy. Computed tomography (CT) scan showed that 90.5% of the patients had absorption of pulmonary lesions. Moreover, white blood cell count and laboratory tests demonstrated that blood lymphocytes, CRP and IL-6 levels returned to normal values [49]. However, due to the absence of a comparator group, the interpretation of tocilizumab-specific effects is limited and only ongoing experimental studies will provide more insight on the true effect of this drug.
Another Chinese retrospective observational study evaluated the effects of tocilizumab (with doses ranging from 80 to 600 mg per administration) in a cohort of 15 patients with COVID-19 [50]. Of these, two (13.3%) patients were moderately ill, six (40.0%) patients were seriously ill, and seven (46.7%) patients were critically ill. In all patients, CRP serum levels were high before the start of the treatment with tocilizumab and they rapidly decreased after tocilizumab treatment. In ten patients, despite an initial increase, IL-6 serum levels decreased after the treatment, while a constant increase was observed for four patients for whom tocilizumab was ineffective. The authors suggested using tocilizumab in patients affected by COVID-19 and at risk of developing cytokine storms and recommended repeated doses (2–3 doses with a frequency of daily, every other day, or every 3 days) for critically ill patients with elevated IL-6 serum levels.
Further evidence of the effectiveness of tocilizumab on COVID-19 patients emerges from a case report of a 42-year-old male affected by metastatic sarcomatoid clear cell renal cell carcinoma who was hospitalized for fever [51]. On the sixth day, the real-time polymerase chain reaction (RT-PCR) assay proved him positive for SARS-CoV-2. The patient was initially treated with lopinavir/ritonavir, which was ineffective, leading him to develop sudden dyspnea and an increased need for oxygen supplementation. The patient was subsequently treated with two intravenous doses of tocilizumab 8 mg/kg. A clinical improvement was rapidly observed and the oxygen consumption also decreased. The treatment was fully withdrawn on day 12. The clinical improvement was also confirmed by CT scan that showed a partial regression of the pulmonary infiltration and by laboratory examinations demonstrating a decrease in serum CRP levels in 4 days. The patient fully recovered from COVID-19 symptoms on day 12.
More recent data on the effectiveness of tocilizumab in COVID-19 patients come from an Italian observational study that enrolled 100 patients with confirmed COVID-19 pneumonia and ARDS requiring ventilatory support, from March 9 until March 20, 2020. Patients were treated with tocilizumab at a dosage of 8 mg/kg by two consecutive intravenous infusions every 12 h. Based on clinical response, a third infusion was optional. Improvement in ADRS was assessed at 24–72 h and 10 days after administration of tocilizumab, using the ‘Brescia-COVID respiratory severity scale’ (BCRSS 0–8, with higher scores indicating higher severity). Of the 100 treated patients, 43 received tocilizumab in the ICU, while 57 received it in the general ward. Overall, at 10 days, the respiratory condition was improved or stabilized in 77 patients (77%), of whom 61 (79.2%) showed a significant reduction in lung lesions and 15 (19.5%) were discharged from the hospital [52]. However, a limitation of this study is the lack of a control group.
As regards experimental investigations, 49 clinical trials of anti-IL-6 drugs in COVID-19 patients are currently ongoing, as registered on ClinicalTrials.gov and the EU Clinical Trials Register (updated to 21 May 2020). Of these, 36 (73.5%) are aimed at investigating tocilizumab, 15 (30.6%) sarilumab, and 3 (6.1%) siltuximab. The majority of these studies are phase II clinical trials (N = 23; 46.9%), followed by phase III clinical trials (N = 10; 20.4%). The remaining studies are phase II/III clinical trials (N = 6; 12.3%), phase IV clinical trials (N = 3; 6.1%), observational studies (N = 6; 12.3%) and phase I clinical trials (N = 1; 2.0%). Only nine (18.4%) of them are sponsored by pharmaceutical companies. Most of these studies are conducted in European (N = 33; 67.3%) or American (N = 14; 28.6%) countries. The estimated enrollment ranges from 20 patients in the smallest study to 12,000 patients in the largest study, which is evaluating several different pharmacological interventions (Online Resource 2, see ESM).
Although clinical evidence is still sparse, in March 2020, the Chinese National Medical Products Administration (NMPA) approved tocilizumab for the treatment of patients affected by COVID-19 with serious lung injury and elevated IL-6 levels [53]. Several national drug agencies have approved anti-IL-6 agents for compassionate use. Accordingly, the Society for Immunotherapy of Cancer (SITC) issued a statement requesting to maximize the availability of anti-IL-6/IL-6R drugs for compassionate use to treat critically ill hospitalized patients with COVID-19 [54].
5 Monitoring of Safety of Anti-IL-6 Agents
The use of anti-IL-6 drugs is associated with an increased risk of severe infections (e.g., tuberculosis); accordingly, monitoring for early detection of infections [55,56,57,58] is recommended. Other common adverse reactions of anti-IL-6 agents include increased transaminase blood levels (tocilizumab and sarilumab) and cytopenias [56,57,58,59]. The mechanism underlying anti-IL-6-induced neutropenia is unclear and it could be related to a margination effect rather than myelosuppression [60]. Serious drug-induced liver injury, including acute liver failure, hepatitis, and jaundice, have been observed with tocilizumab [56,57,58].
A recent review of literature aiming to assess the efficacy of tocilizumab for the treatment of CRS carried out a retrospective analysis of pooled data from prospective clinical trials of CAR T-cell therapies for hematological malignancies. No adverse reactions to tocilizumab in the patients treated for CRS were reported. However, as confirmed by authors, there were no specific assessments for the safety of tocilizumab (e.g., infusion reactions, exacerbation of CAR T cell-induced neurotoxicity, prolonged neutropenia) in clinical trials analyzed. Data reviewed were considered insufficient to assess the overall activity of tocilizumab for treatment of CRS, and further post-marketing studies to confirm the safety of tocilizumab in patients with CRS are required. Nevertheless, the risks associated with tocilizumab seem to be outweighed by the potential benefits observed in patients with severe or life-threatening CRS and potentially for COVID-19 patients [61].
Hypersensitivity reactions, erythema, pruritus, and edema are adverse reactions occasionally observed after administration of anti-IL-6 drugs. In case of hypersensitivity reactions, administration of anti-IL-6 agents should be immediately stopped [56,57,58].
6 Conclusions
The pathological mechanisms leading to severe clinical manifestations in COVID-19 patients have not been fully determined. It has been demonstrated that serum levels of IL-6 are significantly elevated in these patients, thus leading to an excessive immune response and autoimmune injury. Except for tocilizumab in China, no anti-IL-6 drugs have been specifically approved for COVID-19 treatment so far. To shorten timeframes and reduce costs, repurposing of drugs that have already proven to be safe and effective in humans in other indications could be a valid option in such difficult circumstances, while awaiting more experimental clinical evidence on potentially eligible drugs for COVID-19 treatment to be generated. There is a strong rationale for the use of anti-IL-6 agents in COVID-19 patients, mostly in the advanced disease stage. However, despite their promising effects, available clinical evidence is limited and only partly present for tocilizumab. Nevertheless, several phase II and III clinical studies of anti-IL-6 are ongoing and will eventually shed light on the beneficial effects of these drugs in COVID-19. While awaiting the preliminary results of these studies, the potential toxicity of anti-IL-6 should be carefully monitored and managed, whenever clinicians decide to treat patients with anti-IL-6 agents.
References
European Centre for Disease Prevention and Control. Situation update worldwide, as of 24 May 2020 [Internet]. 2020. https://www.ecdc.europa.eu/en/covid-19-pandemic.
Angus DC. Optimizing the trade-off between learning and doing in a pandemic. JAMA. 2020. https://doi.org/10.1001/jama.2020.4984.
Rome BN, Avorn J. Drug evaluation during the Covid-19 pandemic. N Engl J Med. 2020. https://doi.org/10.1056/NEJMp2009457.
Wei WE, Li Z, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic transmission of SARS-CoV-2—Singapore, January 23–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:411–5.
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1038.
Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–6.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.
McGonagle D, Sharif K, O’Regan A, Bridgewood C. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev. 2020;19(6):102537.
Zou Z, Yan Y, Shu Y, Gao R, Sun Y, Li X, et al. Angiotensin-converting enzyme 2 protects from lethal avian influenza A H5N1 infections. Nat Commun. 2014;5:3594.
Diao B, Wang C, Tan Y, Chen X, Liu Y, Ning L, et al. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19). medRxiv. 2020. https://doi.org/10.1101/2020.02.18.20024364.
Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29.
Yang M. Cell pyroptosis, a potential pathogenic mechanism of 2019-nCoV infection. SSRN Electron J. 2020. https://doi.org/10.2139/ssrn.3527420.
Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–3.
Peiris JSM, Chu CM, Cheng VCC, Chan KS, Hung IFN, Poon LLM, et al. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet. 2003;361(9371):1767–72.
Mescher MF, Curtsinger JM, Agarwal P, Casey KA, Gerner M, Hammerbeck CD, et al. Signals required for programming effector and memory development by CD8+ T cells. Immunol Rev. 2006;211:81–92.
Zhu J, Yamane H, Paul WE. Differentiation of effector CD4 T cell populations. Annu Rev Immunol. 2010;28:445–89.
He L, Ding Y, Zhang Q, Che X, He Y, Shen H, et al. Expression of elevated levels of pro-inflammatory cytokines in SARS-CoV-infected ACE2+ cells in SARS patients: Relation to the acute lung injury and pathogenesis of SARS. J Pathol. 2006;210(3):288–97.
Brooks DG, Trifilo MJ, Edelmann KH, Teyton L, McGavern DB, Oldstone MBA. Interleukin-10 determines viral clearance or persistence in vivo. Nat Med. 2006;12(11):1301–9.
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
Liao Y, Wang X, Huang M, Tam JP, Liu DX. Regulation of the p38 mitogen-activated protein kinase and dual-specificity phosphatase 1 feedback loop modulates the induction of interleukin 6 and 8 in cells infected with coronavirus infectious bronchitis virus. Virology. 2011;420(2):106–16.
Zhou Y, Fu B, Zheng X, Wang D, Zhao C, Qi Y, et al. Aberrant pathogenic GM-CSF+ T cells and inflammatory CD14+CD16+ monocytes in severe pulmonary syndrome patients of a new coronavirus. bioRxiv. 2020. https://doi.org/10.1101/2020.02.12.945576.
Mihara M, Hashizume M, Yoshida H, Suzuki M, Shiina M. IL-6/IL-6 receptor system and its role in physiological and pathological conditions. Clin Sci. 2012;122(4):143–59.
Jones SA, Richards PJ, Scheller J, Rose-John S. IL-6 transsignaling: the in vivo consequences. J Interf Cytokine Res. 2005;25(5):241–53.
Conti P, Gallenga CE, Tetè G, Caraffa A, Ronconi G, Younes A, et al. How to reduce the likelihood of coronavirus-19 (CoV-19 or SARS-CoV-2) infection and lung inflammation mediated by IL-1. J Biol Regul Homeost Agents. 2020;34(2):10.23812.
Chen IY, Moriyama M, Chang MF, Ichinohe T. Severe acute respiratory syndrome coronavirus viroporin 3a activates the NLRP3 inflammasome. Front Microbiol. 2019;10:50.
Farag NS, Breitinger U, Breitinger HG, El Azizi MA. Viroporins and inflammasomes: a key to understand virus-induced inflammation. Int J Biochem Cell Biol. 2020;122:105738.
Ichinohe T, Pang IK, Iwasaki A. Influenza virus activates inflammasomes via its intracellular M2 ion channel. Nat Immunol. 2010;11(5):404–10.
Tan YJ, Lim SG, Hong W. Characterization of viral proteins encoded by the SARS-coronavirus genome. Antiviral Res. 2005;65(2):69–78.
Ogata A, Kato Y, Higa S, Yoshizaki K. IL-6 inhibitor for the treatment of rheumatoid arthritis: a comprehensive review. Mod Rheumatol. 2019;29(2):258–67.
Schinnerling K, Aguillón JC, Catalán D, Soto L. The role of interleukin-6 signalling and its therapeutic blockage in skewing the T cell balance in rheumatoid arthritis. Clin Exp Immunol. 2017;189(1):12–20.
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–4.
Schoels MM, Van Der Heijde D, Breedveld FC, Burmester GR, Dougados M, Emery P, et al. Blocking the effects of interleukin-6 in rheumatoid arthritis and other inflammatory rheumatic diseases: systematic literature review and meta-analysis informing a consensus statement. Ann Rheum Dis. 2013;72(4):583–9.
Alfonso-Cristancho R, Armstrong N, Arjunji R, Riemsma R, Worthy G, Ganguly R, et al. Comparative effectiveness of biologics for the management of rheumatoid arthritis: systematic review and network meta-analysis. Clin Rheumatol. 2017;36(1):25–34.
Haraoui B, Casado G, Czirják L, Taylor A, Bernasconi C, Reiss W, et al. Patterns of tocilizumab use, effectiveness and safety in patients with rheumatoid arthritis: core data results from a set of multinational observational studies. Clin Exp Rheumatol. 2017;35(6):899–906.
Davila ML, Riviere I, Wang X, Bartido S, Park J, Curran K, et al. Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci Transl Med. 2014;6(224):224ra25.
Maude SL, Barrett D, Teachey DT, Grupp SA. Managing cytokine release syndrome associated with novel T cell-engaging therapies. Cancer J (United States). 2014;20(2):119–22.
Fitzgerald JC, Weiss SL, Maude SL, Barrett DM, Lacey SF, Melenhorst JJ, et al. Cytokine release syndrome after chimeric antigen receptor T cell therapy for acute lymphoblastic leukemia. Crit Care Med. 2017;45(2):e124–31.
Brudno JN, Kochenderfer JN. Toxicities of chimeric antigen receptor T cells: recognition and management. Blood. 2016;127(26):3321–30.
Maude SL, Frey N, Shaw PA, Aplenc R, Barrett DM, Bunin NJ, et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med. 2014;371(16):1507–17.
Alvi RM, Frigault MJ, Fradley MG, Jain MD, Mahmood SS, Awadalla M, et al. Cardiovascular events among adults treated with chimeric antigen receptor T-cells (CAR-T). J Am Coll Cardiol. 2019;74(25):3099–108.
Kochenderfer JN, Dudley ME, Kassim SH, Somerville RPT, Carpenter RO, Maryalice SS, et al. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J Clin Oncol. 2015;33(6):540–9.
Frey NV, Levine LB, Lacey SF, Grupp SA, Maude SL, Schuster SJ, Shaw P, Hwang W-T, Wasik MA, Obstfeld A, Leung M, Shen A, Ericson SG, Melenhorst JJ, June CH, Porter D. Refractory cytokine release syndrome in recipients of chimeric antigen receptor (CAR) T cells. Blood. 2014;45(2):e124–31.
Grupp SA, Kalos M, Barrett D, Aplenc R, Porter DL, Rheingold SR, et al. Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. N Engl J Med. 2013;368(16):1509–18.
Van Rhee F, Wong RS, Munshi N, Rossi JF, Ke XY, Fosså A, et al. Siltuximab for multicentric Castleman’s disease: a randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2014;15(9):966–74.
June RR, Olsen NJ. Room for more IL-6 blockade? Sarilumab for the treatment of rheumatoid arthritis. Expert Opin Biol Ther. 2016;16(10):1303–9.
Raimondo MG, Biggioggero M, Crotti C, Becciolini A, Favalli EG. Profile of sarilumab and its potential in the treatment of rheumatoid arthritis. Drug Des Dev Ther. 2017;11:1593–603.
Turtle CJ, Hay KA, Hanafi LA, Li D, Cherian S, Chen X, et al. Durable molecular remissions in chronic lymphocytic leukemia treated with CD19-Specific chimeric antigen Receptor-modified T cells after failure of ibrutinib. J Clin Oncol. 2017;35(26):3010–20.
Dholaria BR, Bachmeier CA, Locke F. Mechanisms and management of chimeric antigen receptor T-cell therapy-related toxicities. BioDrugs. 2019;33(1):45–60.
Xu X, Han M, Li T, Sun W, Wang D, Fu B, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci USA. 2020;117(20):10970–5.
Luo P, Liu Y, Qiu L, Liu X, Liu D, Li J. Tocilizumab treatment in COVID-19: a single center experience. J Med Virol. 2020. https://doi.org/10.1002/jmv.25801.
Michot J-M, Albiges L, Chaput N, Saada V, Pommeret F, Griscelli F, et al. Tocilizumab, an anti-IL6 receptor antibody, to treat Covid-19-related respiratory failure: a case report. Ann Oncol. 2020. https://doi.org/10.1016/j.annonc.2020.03.300.
Toniati P, Piva S, Cattalini M, Garrafa E, Regola F, Castelli F, et al. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: a single center study of 100 patients in Brescia, Italy. Autoimmun Rev. 2020;19(7):102568. https://doi.org/10.1016/j.autrev.2020.102568.
Office of the Chinese Medicine Bureau. State Health Office Medical Letter [2020] No. 184: Notice regarding the issuance of a new coronavirus pneumonia diagnosis and treatment plan (for trial implementation of the seventh edition) [Internet]. http://www.gov.cn/zhengce/zhengceku/2020-03/04/content_5486705.htm. Accessed 26 May 2020.
Ascierto PA, Fox B, Urba W, Carrizosa Anderson A, Atkins MB, Borden EC, Brahmer J, Butterfield LH, Cesano A, Chen D, de Gruijl T, Dillman RO, Drake CG, Emens LA, Gajewski TF, Gulley JL, Hodi FS, Hwu P, Kaufman D, Kaufman H, Lotze MM. Insights from immuno-oncology: the society for immunotherapy of cancer statement on access to IL-6-targeting therapies for COVID-19. J Immunother Cancer. 2020;8(1):e000878.
Kourbeti IS, Ziakas PD, Mylonakis E. Biologic therapies in rheumatoid arthritis and the risk of opportunistic infections: a meta-analysis. Clin Infect Dis. 2014;58(12):1649–57.
European Medicines Agency. Tocilizumab: summary of product characteristics [Internet]. https://www.ema.europa.eu/en/documents/product-information/roactemra-epar-product-information_en.pdf. Accessed 26 May 2020.
European Medicines Agency. Sarilumab: summary of product characteristics [Internet]. https://www.ema.europa.eu/en/documents/product-information/kevzara-epar-product-information_en.pdf. Accessed 26 May 2020.
European Medicines Agency. Siltuximab: summary of product characteristics [Internet]. https://www.ema.europa.eu/en/documents/product-information/sylvant-epar-product-information_en.pdf. Accessed 26 May 2020.
Grange S, Schmitt C, Banken L, Kuhn B, Zhang X. Thorough QT/QTc study of tocilizumab after single-dose administration at therapeutic and supratherapeutic doses in healthy subjects. Int J Clin Pharmacol Ther. 2011;49(11):648–55.
Shovman O, Shoenfeld Y, Langevitz P. Tocilizumab-induced neutropenia in rheumatoid arthritis patients with previous history of neutropenia: case series and review of literature. Immunol Res. 2014;61(1–2):164–8.
Le RQ, Li L, Yuan W, Shord SS, Nie L, Habtemariam BA, et al. FDA approval summary: tocilizumab for treatment of chimeric antigen receptor T cell-induced severe or life-threatening cytokine release syndrome. Oncologist. 2018;23(8):943–7.
Jatiani SS, Baker SJ, Silverman LR, Premkumar Reddy E. JAK/STAT pathways in cytokine signaling and myeloproliferative disorders: approaches for targeted therapies. Genes Cancer. 2010;1(10):979–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to prepare this article.
Conflict of interest
G Trifirò has served on advisory boards for Sandoz, Hospira, Sanofi, Biogen, Ipsen, and Shire; is a consultant for Otsuka; is the principal investigator of observational studies funded by several pharmaceutical companies (e.g., Amgen, AstraZeneca, Daiichi Sankyo, and IBSA) to University of Messina; and is scientific coordinator of the Master’s program ‘Pharmacovigilance, pharmacoepidemiology and pharmacoeconomics: real-world data evaluations’ at University of Messina, which is partly funded by several pharmaceutical companies. Salvatore Crisafulli, Valentina Isgrò, Laura La Corte, and Fabiola Atzeni have no conflicts of interest that are directly relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Crisafulli, S., Isgrò, V., La Corte, L. et al. Potential Role of Anti-interleukin (IL)-6 Drugs in the Treatment of COVID-19: Rationale, Clinical Evidence and Risks. BioDrugs 34, 415–422 (2020). https://doi.org/10.1007/s40259-020-00430-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-020-00430-1