Abstract
Ruxolitinib cream 1.5% (OPZELURA™) is a topical formulation of ruxolitinib, a potent, selective inhibitor of Janus kinase (JAK)1 and JAK2. The targeting of these kinases is associated with therapeutic benefits in patients with atopic dermatitis (AD). In two identically designed, multinational, phase III studies in patients aged ≥ 12 years with mild to moderate AD, ruxolitinib cream 1.5% improved measures of disease severity, pruritus and sleep disturbance relative to vehicle cream when applied twice daily for 8 weeks. Disease severity was controlled for the next 44 weeks when applied as needed to active lesions. Ruxolitinib cream 1.5% was well tolerated in this patient population; its safety profile was similar to that of vehicle cream over the short term, with the types of treatment-emergent adverse events typical of those seen in the vehicle-controlled period over the longer term. Moreover, application site treatment-emergent adverse events indicative of skin tolerability issues (e.g. stinging/burning sensation) were infrequent and no safety findings suggestive of systemic JAK inhibition were identified. Although further longer-term data would be of use, ruxolitinib cream 1.5% provides an alternative to established topical agents (e.g. corticosteroids and calcineurin inhibitors) for the treatment of mild to moderate AD in adults and adolescents.
Plain Language Summary
Atopic dermatitis (AD; also known as atopic eczema) is a chronic, relapsing, inflammatory skin disease that most commonly occurs in children but may also affect adults. Ruxolitinib cream 1.5% (OPZELURA™) is a topical therapy that inhibits Janus kinase (JAK)1 and JAK2, which are enzymes that can modify the inflammatory pathways involved in AD. It is approved in the USA for short-term and non-continuous longer-term treatment of mild to moderate AD in non-immunocompromised patients aged ≥ 12 years whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. Patients experienced clearer skin and a reduction in itch and disturbed sleep when treated with ruxolitinib cream 1.5% twice daily compared with a non-medicated cream for 8 weeks. Moreover, clearer skin was maintained for a further 44 weeks when using the treatment as needed. The safety profile of ruxolitinib cream 1.5% was similar to that of the non-medicated cream, and stinging/burning sensations following application were infrequent. Thus, ruxolitinib cream 1.5% offers an alternative to established topical agents (e.g. corticosteroids and calcineurin inhibitors) for the treatment of adults and adolescents with mild to moderate AD.
Similar content being viewed by others
Digital Features for this Adis Drug Evaluation can be found at https://doi.org/10.6084/m9.figshare.20280291. |
First topical JAK inhibitor approved in the USA |
Provides early and sustained improvements in disease severity, pruritus and sleep disturbance measures when applied twice daily over the short term |
Controls disease severity measures when applied as needed to active lesions over the longer term |
Safety profile similar to that of vehicle cream; no safety findings suggestive of systemic JAK inhibition |
1 Introduction
Atopic dermatitis (AD; also known as atopic eczema) is a chronic, relapsing, inflammatory skin disorder that occurs most commonly in children, but may also affect adults [1]. Along with eczematous skin lesions, it is characterized by pruritus, which negatively affects health-related quality of life via sleep disturbance, anxiety and depression [2]. The pathogenesis of AD comprises the abnormal activation of type 2 helper T (Th2), type 22 helper T (Th22) and, to a lesser degree, type 17 helper T cells [3]. Additionally, the Janus kinase (JAK)–signal transducer and activator of transcription (STAT) signalling pathway is involved in the signalling of various cytokines implicated in AD, including Th2 cytokines IL-4, IL-13 and IL-31 (a potent pruritogenic cytokine) and the Th22 cytokine IL-22 [3]. The JAK family includes JAK1, JAK2, JAK3 and tyrosine kinase 2 (TYK2), with each member selectively binding to different receptor chains [4]. Targeting these kinases has been associated with therapeutic benefits in patients with AD [5].
The therapeutic management of AD encompasses both non-pharmacological (e.g. moisturizers) and pharmacological (e.g. anti-inflammatory agents) interventions, with topical agents (e.g. corticosteroids, calcineurin inhibitors and phosphodiesterase 4 inhibitors) the cornerstone of treatment in most patients [1, 6, 7]. There are, however, limitations of use with any agent. For instance, topical corticosteroids can be absorbed to such a degree that they result in systemic adverse events (AEs), with such AEs more likely with higher potency agents and prolonged continuous use, especially in patients receiving corticosteroids via another route of administration (e.g. oral and inhaled) [6]. Their use is also limited in sensitive skin areas [7], and has been associated with patients’ concerns over AEs, potentially resulting in poor adherence [8]. Compared with topical corticosteroids, topical calcineurin inhibitors are associated with a higher frequency of local reactions (e.g. burning, stinging) upon application [6]. While these tend to lessen over several applications, they may result in patient non-adherence if the patient is not made aware of them [6]. Thus, there remains a need for other topical therapeutic options.
Ruxolitinib cream 1.5% (OPZELURA™) is the first topical JAK inhibitor approved in the USA. This article discusses pharmacological, therapeutic efficacy and tolerability data relevant to its use in adults and adolescents with mild to moderate AD.
2 Pharmacodynamic Properties of Ruxolitinib Cream 1.5%
Ruxolitinib is a potent and selective JAK1 and JAK2 inhibitor [9, 10]. In vitro, it displayed nanomolar potency against JAK1 and JAK2 [mean half-maximal inhibitory concentration (IC50) 3.3 and 2.8 nmol/L], less activity against JAK3 and TYK2 (mean IC50 428 and 19 nmol/L) and no activity against (unrelated) Chk2 and c-MET (mean IC50 > 1000 and > 10,000 nmol/L [11].
Topical ruxolitinib reduced inflammation in preclinical models. In a murine delayed-type hypersensitivity model, it suppressed STAT3 phosphorylation, disorganized keratinocyte hyperplasia, lymphocyte infiltration and oedema, and inhibited IL-23- or thymic stromal lymphopoietin (TSLP)-induced ear swelling [10]. Ruxolitinib cream 1.5% twice daily downregulated Th2-driven inflammation, resulting in reduced skin thickening and itch, in multiple murine models of dermatitis [12], and, along with resolving skin dermatitis, was associated with a restoration of sleep to baseline levels without sedation in a murine model of acute TSLP-induced dermatitis. An ex vivo human skin dermatitis model corroborated the findings of the multiple murine dermatitis models [12].
In a topical toxicology study in Göttingen minipigs (a preferred species in such studies owing to the similarity of swine to human skin), ruxolitinib cream 0.5%, 1.0% or 1.5% once daily [application rate of 4 mg/cm2 to 10% body surface area (BSA)] for 28 days was not associated with alterations in clinical or dermal signs, body weight, food consumption, clinical pathology or histopathology [10].
In biomarker analyses of data from an 8-week, randomized, double-blind, dose-ranging, multinational, phase II study in adults with mild to moderate AD, ruxolitinib was associated with reductions in disease-related inflammatory markers [13, 14]. Of 1012 inflammatory marker proteins evaluated in 19, 16, 13 and 17 patients receiving triamcinolone cream 0.1% twice daily (administered for 4 weeks followed by vehicle for 4 weeks), ruxolitinib cream 1.5% twice daily for 8 weeks, ruxolitinib cream 1.5% once daily for 8 weeks or vehicle for 8 weeks, respectively, 183, 26, 50 and 17 were modulated, with 175, 15, 50 and 17 downregulated [13]. Serum levels of Th2 biomarkers (IgE, and thymus and activation-regulated chemokine) declined with the application of ruxolitinib cream 1.5% twice daily, although the baseline levels of these biomarkers did not predict the response to ruxolitinib treatment, as assessed by the percentage reduction in the Eczema Area and Severity Index (EASI) score [14]. Moreover, a biomarker analysis of data from two multinational phase III studies in patients aged ≥ 12 years with mild to moderate AD (TRuE-AD1 and TRuE-AD2; Sect. 4) suggests that changes in systemic protein levels following the twice-daily application of ruxolitinib cream 1.5% reflect local drug effects and improved clinical condition and were not correlated with steady-state plasma ruxolitinib concentrations [15].
3 Pharmacokinetic Properties of Ruxolitinib Cream 1.5%
Plasma concentrations of ruxolitinib following the twice-daily application of ruxolitinib cream 1.5% are minimal and not expected to reach the threshold associated with the AEs commonly seen with oral JAK inhibitor therapy [16]. In a pooled analysis of data [16] from TRuE-AD1 and TRuE-AD2 (Sect. 4) [17], mean bioavailability was 7.7% and 6.2% following the application of ruxolitinib cream 0.75% and 1.5% twice daily [16]. At steady state, mean trough plasma ruxolitinib concentrations were 23.8 and 35.7 nmol/L with the respective dosages; in comparison, the IC50 for thrombopoietin-stimulated phosphorylated STAT3 inhibition (a JAK/STAT signaling marker) is 281 nmol/L [16]. In adults with affected AD areas of up to 20% BSA participating in the multinational phase II study [18, 19], the increase in trough plasma ruxolitinib concentrations was less than dose-proportional at steady state following the application of ruxolitinib cream 0.15% once daily, 0.5% once daily, 1.5% once daily and 1.5% twice daily [16]. With no clinically relevant changes in haematological parameters seen in the three studies (Sect. 5), correlation analyses between plasma ruxolitinib concentrations at steady state and haematological changes could not be generated [16]. Moreover, in an open-label, multinational, phase I, maximum use study in patients aged 12–65 years with AD who had an IGA score of ≥ 2 and BSA involvement of ≥ 25% (median 31.2%; range 25–90%), mean steady state plasma ruxolitinib concentrations (104 nmol/L) were well below the IC50 for JAK-mediated myelosuppression following the twice daily application of ruxolitinib cream 1.5% for 28 days, with concentrations decreasing further when ruxolitinib was applied as needed for 28 days [20].
There is no evidence of ruxolitinib accumulation following the daily application of ruxolitinib cream 1.5% for 28 days in patients with AD [9]. Ruxolitinib is highly bound (≈ 97%) to plasma proteins and is predominately metabolized by CYP3A4 and to a lesser extent by CYP2C9 in vitro. Ruxolitinib and its metabolites are primarily excreted via the urine (74%) and faeces (22%); < 1% is excreted as unchanged drug. Following the application of ruxolitinib cream 1.5%, the estimated mean terminal half-life of ruxolitinib was ≈ 116 h [9].
Drug interaction studies of ruxolitinib cream 1.5% have not been conducted [9]. According to in vitro studies, the topical application of ruxolitinib is not expected to result in CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6, 3A4, P-gp, BCRP, OATP1B1, OATP1B3, OCT1, OCT2, OAT1 or OAT3 inhibition, or CYP1A2, 2B6 or 3A4 induction. Ruxolitinib is not a substrate of P-gp but is a CYP3A4 substrate. Thus, the concomitant administration of ruxolitinib cream 1.5% and strong CYP3A4 inhibitors should be avoided (owing to the possibility of increased systemic concentrations of ruxolitinib) [9].
Findings from a Göttingen minipig model determined that topical application resulted in higher drug concentrations in the skin that oral administration [21]. The average total epidermal and dermal concentrations of ruxolitinib were 1989- and 507-fold higher following topical (cream 1.5% applied to 10% BSA) versus oral (40 mg/kg) administration of ruxolitinib. Moreover, the unbound ruxolitinib concentration (≈ 12 nmol/L) in the dermis 74 h following topical application is predicted to result in sustained and near-complete inhibition of JAK–STAT signalling [21].
4 Therapeutic Efficacy of Ruxolitinib Cream 1.5%
The potential of ruxolitinib cream in adults with mild to moderate AD was demonstrated in the multinational phase II study (Sect. 2) [18, 19]. In this study, the approved ruxolitinib dosage of 1.5% twice daily (Sect. 6) achieved a mean percentage change from baseline in the EASI score at week 4 that was significantly (p < 0.0001) greater than vehicle (primary endpoint) but that did not significantly differ from triamcinolone cream 0.1% twice daily (key secondary endpoint) [18, 19]. This section focuses on two identically designed, randomized, double-blind, vehicle-controlled, multinational, phase III confirmatory studies (TRuE-AD1 and TRuE-AD2), which evaluated the therapeutic efficacy of ruxolitinib cream 1.5% in patients aged ≥ 12 years with mild to moderate AD [17]. Individual [17, 22, 23] and pooled [24,25,26,27,28,29,30,31,32,33,34,35,36] data from these two studies are discussed.
Patients who had AD for ≥ 2 years and an Investigator’s Global Assessment (IGA) score of 2 (mild) or 3 (moderate) and BSA involvement of 3–20% (excluding the scalp) were enrolled in TRuE-AD1 and TRuE-AD2 [17]. Those with investigator-determined unstable AD (i.e. spontaneously improving and/or rapidly deteriorating) or other types of eczema, or who were immunocompromised or had used AD therapies during the washout period prior to baseline (biologics: 12 weeks or 5 half-lives; systemic corticosteroids or other immunomodulating agents: 4 weeks; topical drugs: 1 week) or during the study were among those excluded [17].
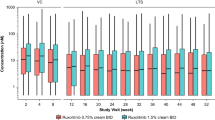
In both studies, patients received ruxolitinib cream 0.75% or 1.5%, or vehicle cream, administered topically twice daily for 8 weeks (vehicle-controlled period); no rescue treatments were permitted [17]. At week 8, eligible patients receiving ruxolitinib cream 0.75% or 1.5% continued on the same regimen for a further 44 weeks, while those receiving vehicle were re-randomized to receive ruxolitinib cream 0.75% or 1.5% twice daily (double-blind longer-term safety (LTS) period) [17, 22, 24]. During the vehicle-controlled period, patients were instructed to continue treating the lesions regardless of lesion improvement [17, 24]. During the LTS period, patients were instructed to only treat active skin lesions and to stop therapy 3 days after lesion clearance, with treatment to be restarted at the first sign of recurrence [24]. Discussion in this section focuses on the approved ruxolitinib dosage of 1.5% twice daily (Sect. 6).
At baseline, the distribution of demographics across the treatment groups was similar in each study [17]. In TRuE-AD1 (n = 631) and TRuE-AD2 (n = 618), respectively, the median patient age was 32.0 and 33.0 years, with 19.5% and 19.7% of patients aged 12–17 years, and the mean Itch Numerical Rating Scale (NRS) score was 5.1 and 5.1; 75.9% and 74.1% of patients had baseline IGA scores of 3 [17].
4.1 Short-Term Efficacy
Topical therapy with twice-daily ruxolitinib cream 1.5% for 8 weeks improved disease severity, pruritus and sleep disturbance measures in patients aged ≥ 12 years with mild to moderate AD [17, 25, 26]. At week 8, ruxolitinib cream 1.5% was significantly more effective than vehicle as regards the proportion of patients achieving an IGA treatment success (IGA-TS) response (primary endpoint) in TRuE-AD1, TRuE-AD2 and a pooled analysis of these studies (Table 1 for definitions and results). Additionally, the efficacy of ruxolitinib cream 1.5% was demonstrated for a 75% improvement from baseline in the Eczema Area and Severity Index (EASI) score (EASI75) response (a key secondary endpoint) (Table 1 for definitions and results). A treatment effect was seen from week 2 for both the IGA-TS response (TRuE-AD1: 27.3% of ruxolitinib cream 1.5% recipients vs 3.2% of vehicle recipients; TRuE-AD2: 25.0% vs 4.2%; pooled analysis: 26.2% vs 3.7%) and the EASI75 response (TRuE-AD1: 36.0% vs 5.6%; TRuE-AD2: 31.6% vs 4.2%; pooled analysis: 33.9% vs 4.9%) [17, 25].
In terms of patient-reported key secondary endpoints, significantly more ruxolitinib cream 1.5% than vehicle recipients achieved a clinically relevant (i.e. ≥ 4-point improvement from baseline) Itch NRS response at week 8 in TRuE-AD1, TRuE-AD2 and the pooled analysis (Table 1). A significant (p ≤ 0.048 vs vehicle) difference was seen as early as day 2 (≈ 36 h following the first application) in TRuE-AD1 (11.6% of ruxolitinib cream 1.5% recipients vs 2.9% of vehicle recipients), TRuE-AD2 (10.8% vs 1.3%) and a pooled analysis of these studies (11.2% vs 2.1%) [17, 26]. At week 2, 33.5% of ruxolitinib cream 1.5% recipients and 5.1% of vehicle recipients in TRuE-AD1, 32.2% and 5.0% of patients in TRuE-AD2 and 32.9% and 5.1% of patients in the pooled analysis had achieved a clinically relevant Itch NRS response [17, 26]. In the pooled analysis, the median time to a clinically relevant Itch NRS response was 13.0 days for patients receiving ruxolitinib cream 1.5%; the median time for patients receiving vehicle was not reached [26]. A clinically relevant (i.e. ≥ 6-point improvement from baseline) Patient-Reported Outcomes Measurement Information System short form sleep disturbance questionnaire (PROMIS 8b) response was achieved in significantly more ruxolitinib cream 1.5% than vehicle recipients at week 8 in TRuE-AD1 and the pooled analysis, but not TRuE-AD2 (Table 1). At week 2, 14.7% of ruxolitinib cream 1.5% recipients and 5.2% of vehicle recipients in TRuE-AD1, 18.0% and 10.0% of patients in TRuE-AD2 and 16.3% and 7.5% of patients in the pooled analysis had achieved a clinically relevant PROMIS 8b response [17, 25].
With regard to other secondary endpoints, ruxolitinib cream 1.5% was associated with significant (nominal p < 0.0001) between-group differences relative to vehicle in the proportion of patients achieving a 90% improvement from baseline in the EASI score at week 8 [TRuE-AD1: 44.3% vs 9.5%, odds ratio (OR) 7.8 (95% CI 4.0–16.4); TRuE-AD2 43.4% vs 35.1%, OR 19.0 (95% CI 7.4–62.4)], with a treatment effect seen from week 2 (TRuE-AD1: 19.8% vs 2.4%; TRuE-AD2: 15.8% vs 0.8%) [17]. Moreover, the mean change from baseline in the EASI score was significantly (nominal p < 0.0001) greater with ruxolitinib cream 1.5% than placebo at week 8 (TRuE-AD1: − 77.2 vs − 40.5; TRuE-AD2: − 74.7 vs − 28.9), with significant (nominal p < 0.0001) differences seen at each timepoint from week 2 [17]. In the pooled analysis, the mean change from baseline at week 8 in the Itch NRS score was significantly (nominal p < 0.0001) greater in the ruxolitinib cream 1.5% group than the vehicle group (− 3.3 vs − 1.6); a significant (nominal p < 0.02 vs vehicle) between-group difference in this endpoint was seen within ≈ 12 h of the first application of ruxolitinib cream 1.5% (mean change from baseline of − 0.5 vs − 0.1 with vehicle) [26].
An itch-free state (defined as patients with a baseline Itch NRS score > 1 who achieved an Itch NRS score of 0 or 1) was achieved by significantly (p < 0.05) more ruxolitinib cream 1.5% than vehicle recipients at week 8 (49.5% vs 18.3%; pooled data) [37]. A significant (p < 0.05) between-group difference in this measure was seen within ≈ 36 h of the first application of ruxolitinib cream 1.5% and sustained at all timepoints thereafter [37]. Ruxolitinib cream 1.5% was also associated with improvements in work impairment and daily activity impairment (as assessed by the Work Productivity and Activity Impairment Questionnaire–Specific Health Problem version 2.0) compared with vehicle at week 8, according to a post hoc analysis of pooled data [38].
According to subgroup analyses of the pooled data, the benefits of ruxolitinib cream 1.5% on the IGA-TS response were consistent regardless of age [27], sex [27], race [27], atopic comorbidities [28], AD severity at baseline [29, 30], head and/or neck involvement [31] and previous topical or systemic therapy [32]. Moreover, at week 8, among 584 patients who did not achieve an IGA-TS response, a clinically meaningful response [defined as the achievement of 1 of the following: ≥ 50% improvement from baseline in the EASI score, a ≥ 2-point reduction from baseline in the Itch NRS score, ≥ 4-point reduction from baseline in the Dermatology Life Quality Index (DLQI; adults), or a ≥ 6-point reduction from baseline in the Children’s DLQI score (adolescents)] was achieved by significantly more ruxolitinib cream 1.5% than vehicle recipients (85.3% vs 63.2%; p < 0.0001) [33].
4.2 Longer-Term Efficacy
Ruxolitinib cream 1.5% demonstrated effective disease control during the LTS period of TRuE-AD1 and TRuE-AD2, according to a pooled analysis of these studies [24]. At week 52, an IGA score of 0 (clear) or 1 (almost clear) was achieved by 77.8% of 428 patients receiving ruxolitinib cream 1.5% (twice daily during the 8-week vehicle-controlled period and as needed during the 44-week LTS period) and by 74.1% of 96 patients who switched from vehicle to ruxolitinib cream 1.5% at week 8. At this timepoint, mean total affected BSA was 1.4% and 1.7% in the respective patient populations. With the as-needed application of ruxolitinib cream 1.5%, patients who continued treatment and those who switched from vehicle to ruxolitinib cream 1.5% spent a median of 44% and 38% of the 44-week LTS period time off treatment due to lesion clearance. Among 63 patients who achieved clear skin (i.e. an IGA score of 0) with ruxolitinib cream 1.5% at week 8, the median time to first retreatment was 12.0 days [24].
According to subgroup analyses, the benefits of ruxolitinib cream 1.5% on the IGA score of 0 or 1 response and mean affected BSA were consistent between adolescents and the overall patient population (individual study data) [23] and regardless of previous topical or systemic therapy (pooled data) [34] during the LTS period. The beneficial effects of ruxolitinib cream 1.5% over the longer term were also evident in patients with more severe baseline disease (defined as an IGA score of 3, an EASI score of ≥ 16 and a BSA ≥ 10%) [pooled data] [35].
5 Safety and Tolerability of Ruxolitinib Cream 1.5%
Topical therapy with ruxolitinib cream 1.5% was well tolerated in patients aged ≥ 12 years with mild to moderate AD participating in TRuE-AD1 and TRuE-AD2 [17, 24]. No safety findings indicative of systemic JAK inhibition were observed [17, 24].
The safety profile of twice-daily ruxolitinib cream 1.5% was similar across the treatment groups over the 8-week vehicle-controlled period; there were no differences in tolerability based on lesion location [17]. In a pooled analysis of data from this period, treatment-emergent AEs (TEAEs) were reported in 26.5% of 499 ruxolitinib cream 1.5% recipients and 33.2% of 250 vehicle cream recipients, with nasopharyngitis (2.6% vs 0.8%), upper respiratory tract infection (URTI) [2.4% vs 2.0%] and headache (2.2% vs 2.0%) the most frequently reported TEAEs (occurring in > 1% of the total pooled patient population). Application site TEAEs indicative of skin tolerability issues (e.g. stinging/burning sensation) were infrequent with ruxolitinib cream 1.5%: application site burning was reported in 0.8% and 4.8% of patients receiving ruxolitinib cream 1.5% or vehicle, and application site pruritus in 0.2% and 2.8% of patients. Treatment-related AEs (TRAEs) occurred in 4.8% and 11.2% of patients in the ruxolitinib cream 1.5% and vehicle groups, with application site burning (0.8% vs 4.4%) the most frequently reported TRAE (occurring in > 0.5% of the total pooled patient population). Application-site pruritus TRAEs were reported in 0% of ruxolitinib cream 1.5% recipients (vs 2.4% of vehicle recipients). Serious TEAEs occurred in 0.6% and 0.8% of patients receiving ruxolitinib cream 1.5% or vehicle, and treatment discontinuations because of TEAEs in 0.8% and 3.2% of patients [17].
During the 44-week LTS period of TRuE-AD1 and TRuE-AD2, the types of TEAEs seen following as needed application with ruxolitinib cream 1.5% were typical of those seen in the vehicle-controlled period [24]. In a pooled analysis of data from these studies, TEAEs were reported in 62.6% of 446 patients who received ruxolitinib cream 1.5% throughout the vehicle-controlled and LTS periods (total treatment duration 52 weeks) and 57.6% of 99 patients who switched from vehicle to ruxolitinib cream 1.5% at the end of the vehicle-controlled period (total treatment duration 44 weeks). The most frequently reported TEAEs (occurring in > 4% of patients) in the respective patient populations were URTI (11.4% and 7.1% of patients), nasopharyngitis (9.9% and 14.1%), headache (4.5% and 4.0%), bronchitis (3.4% and 5.1%) and influenza (2.5% and 7.1%). TRAEs were reported in 7.4% of patients who received ruxolitinib cream 1.5% throughout the vehicle-controlled and LTS periods and 6.1% of those who switched from vehicle to ruxolitinib cream 1.5% at the end of the vehicle-controlled period, with neutropenia (in 0.9% and 3.0% of patients) the most frequently reported TRAE. In the respective patient populations, serious TEAEs occurred in 1.8% and 1.0% of patients, and treatment discontinuations because of TEAEs in 0.2% and 0% [24]. Notably, incidence rates per 100 patient–years for any TEAE (73.0 vs 191.6) and any application site reaction (2.0 vs 42.2) were lower for patients applying ruxolitinib cream 1.5% (n = 545) at any point during the total (52-week) study period than those applying vehicle (n = 200) during the vehicle-controlled period (pooled analysis) [36].
Among patients who applied ruxolitinib cream 1.5% at any time during TRuE-AD1 and TRuE-AD2 (n = 598), malignancies occurred in two patients and notable serious infections, major adverse cardiac events and thrombotic events were each reported in one patient [24]. None of these events were considered related to ruxolitinib 1.5% cream [24]. No patients died during the vehicle-controlled and LTS periods [17, 24, 39, 40].
According to a phase I maximum use study in patients aged 12–65 years with AD (Sect. 3), ruxolitinib cream 1.5% was generally well tolerated following twice-daily application on all AD lesions (excluding the scalp) for 28 days and then twice-daily application on active AD lesions only for an additional 28 days [20]. In this study, TEAEs and TRAEs were reported in 31.7% and 9.8% of 41 patients [20].
6 Dosage and Administration of Ruxolitinib Cream 1.5%
Ruxolitinib cream 1.5% (15 mg of ruxolitinib per gram of cream) is approved in the USA for the topical short-term and non-continuous chronic treatment of mild to moderate AD in non-immunocompromised patients aged ≥ 12 years whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable [9]. Twice daily application of a thin layer to affected areas of up to 20% BSA is recommended; no more than 60 g/week should be applied. Treatment should be stopped when the signs and symptoms of AD (e.g. itch, rash and redness) have resolved; patients showing no improvements within 8 weeks should be re-examined by their healthcare provider [9].
The US prescribing information carries a boxed warning regarding serious infections, thrombosis, major adverse cardiac events, malignancies and mortality associated with the use of JAK inhibitors in inflammatory conditions [9]. The concomitant administration of ruxolitinib cream 1.5% and therapeutic biologics, other JAK inhibitors or potent immunosuppressants (e.g. azathioprine and cyclosporine) is not recommended, and the use of ruxolitinib cream 1.5% should be avoided in patients with active, serious infections, including localized infections [9]. Local prescribing information should be consulted for detailed information regarding these and other warnings and precautions, potential drug interactions and use in special patient populations.
7 Current Status of Ruxolitinib Cream 1.5% in Mild to Moderate Atopic Dermatitis
Anatomical restrictions, local and/or systemic AEs, and patients' concerns over AEs potentially resulting in poor treatment adherence can limit the use of established topical agents for the treatment of mild to moderate AD (Sect. 1). Recently, the JAK inhibitor ruxolitinib was approved in the USA as a 1.5% cream for the topical short-term and non-continuous chronic treatment of mild to moderate AD in non-immunocompromised patients aged ≥ 12 years whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable (Sect. 6). Owing to the timing of approval, it has not been mentioned in current US guidelines for the treatment of AD [1, 6].
Ruxolitinib cream 1.5% is the first topical JAK inhibitor approved in the USA (Sect. 1). Ruxolitinib potently and selectively inhibits JAK1 and JAK2 (Sect. 2), and its plasma concentrations following topical application are well below the IC50 for JAK-mediated myelosuppression (Sect. 3). US FDA approval was based on data from the TRuE-AD clinical study programme. In patients aged ≥ 12 years with mild to moderate AD participating in TRuE-AD1 and TRuE-AD2, ruxolitinib cream 1.5% provided early and sustained improvements in disease severity, pruritus and sleep disturbance measures relative to vehicle cream when applied twice daily over the short term (8 weeks) (Sect. 4.1), with its as needed application to active lesions controlling disease severity over the longer term (an additional 44 weeks) (Sect. 4.2).
Topical therapy with ruxolitinib cream 1.5% was well tolerated in TRuE-AD1 and TRuE-AD2; there were no safety findings indicative of systemic JAK inhibition (Sect. 5). Its safety profile was similar to that of vehicle cream following twice-daily application over 8 weeks, with no differences seen in tolerability based on lesion location, and the types of TEAEs seen following as needed application were typical of those seen in the vehicle-controlled period. The most frequently reported TEAEs with both twice daily and as needed therapy were URTI, nasopharyngitis and headache. Moreover, application site TEAEs indicative of skin tolerability issues (e.g, stinging/burning sensation) were infrequent (Sect. 5).
Although further longer-term efficacy and tolerability data would be beneficial, current evidence suggests that ruxolitinib cream 1.5% is a useful addition to the topical therapeutic options available for mild to moderate AD, addressing some of the limitations observed with current therapies.
Data Selection Ruxolitinib: 149 records identified
Duplicates removed | 42 |
Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomized trial) | 30 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase I/II trials) | 37 |
Cited efficacy/tolerability articles | 18 |
Cited articles not efficacy/tolerability | 22 |
Search Strategy: EMBASE, MEDLINE and PubMed from 1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were Ruxolitinib, Opzelura, INCB-18424, topical, cream, atopic dermatitis, eczema, pruritus. Records were limited to those in English language. Searches last updated 5 December 2022 | |
Change history
24 March 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40257-023-00769-5
References
Eichenfield LF, Ahluwalia J, Waldman A, et al. Current guidelines for the evaluation and management of atopic dermatitis: a comparison of the Joint Task Force Practice Parameter and American Academy of Dermatology guidelines. J Allergy Clin Immunol. 2017;139(4S):S49–57.
Smith P, Yao W, Shepard S, et al. Developing a JAK inhibitor for targeted local delivery: ruxolitinib cream. Pharmaceutics. 2021;13(7):1044.
Nakashima C, Yanagihara S, Otsuka A. Innovation in the treatment of atopic dermatitis: emerging topical and oral Janus kinase inhibitors. Allergol Int. 2021;71(1):40–6.
O’Shea JJ, Schwartz DM, Villarino AV, et al. The JAK-STAT pathway: impact on human disease and therapeutic intervention. Annu Rev Med. 2015;66:311–28.
Howell MD, Kuo FI, Smith PA. Targeting the Janus kinase family in autoimmune skin diseases. Front Immunol. 2019;10:2342.
Eichenfield LF, Tom WL, Berger TG, et al. Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J Am Acad Dermatol. 2014;71(1):116–32.
Wollenberg A, Barbarot S, Bieber T, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol. 2018;32(5):657–82.
Muller SM, Tomaschett D, Euler S, et al. Topical corticosteroid concerns in dermatological outpatients: a cross-sectional and interventional study. Dermatology. 2016;232(4):444–52.
Incyte Corporation. OPZELURA™ (ruxolitinib) cream, for topical use: US prescribing information. 2022. https://dailymed.nlm.nih.gov/. Accessed 28 Nov 2022.
Fridman JS, Scherle PA, Collins R, et al. Preclinical evaluation of local JAK1 and JAK2 inhibition in cutaneous inflammation. J Invest Dermatol. 2011;131(9):1838–44.
Quintas-Cardama A, Vaddi K, Liu P, et al. Preclinical characterization of the selective JAK1/2 inhibitor INCB018424: therapeutic implications for the treatment of myeloproliferative neoplasms. Blood. 2010;115(15):3109–17.
Scuron MD, Fay BL, Connell AJ, et al. Ruxolitinib cream has dual efficacy on pruritus and inflammation in experimental dermatitis. Front Immunol. 2020;11: 620098.
Owens S, Liu H, Sun K, et al. Ruxolitinib cream significantly modulates inflammatory profiles of atopic dermatitis patients [abstract no. 998]. J Invest Dermatol. 2019;139(5 Suppl):S173.
Owens S, Howell MD. Ruxolitinib cream suppresses Th2 inflammation in adult patients with atopic dermatitis [abstract no. 384]. J Allergy Clin Immunol. 2019;143(2 Suppl):AB128.
Liu H, Gong X, Smith SH. Clinical serum biomarker profiling in TRuE-AD1 and TRuE-AD2 studies after 8 weeks of treatment with ruxolitinib cream [abstract no. LB991]. In: Society for Investigative Dermatology Annual Meeting. 2022.
Gong X, Chen X, Kuligowski ME, et al. Pharmacokinetics of ruxolitinib in patients with atopic dermatitis treated with ruxolitinib cream: data from phase II and III studies. Am J Clin Dermatol. 2021;22(4):555–66.
Papp K, Szepietowski JC, Kircik L, et al. Efficacy and safety of ruxolitinib cream for the treatment of atopic dermatitis: results from 2 phase 3, randomized, double-blind studies. J Am Acad Dermatol. 2021;85(4):863–72.
Kim BS, Howell MD, Sun K, et al. Treatment of atopic dermatitis with ruxolitinib cream (JAK1/JAK2 inhibitor) or triamcinolone cream. J Allergy Clin Immunol. 2020;145(2):572–82.
Kim BS, Sun K, Papp K, et al. Effects of ruxolitinib cream on pruritus and quality of life in atopic dermatitis: results from a phase 2, randomized, dose-ranging, vehicle- and active-controlled study. J Am Acad Dermatol. 2020;82(6):1305–13.
Bissonnette R, Call RS, Raoof T, et al. A maximum-use trial of ruxolitinib cream in adolescents and adults with atopic dermatitis. Am J Clin Dermatol. 2022;23(3):355–64.
Persaud I, Diamond S, Pan R, et al. Plasma pharmacokinetics and distribution of ruxolitinib into skin following oral and topical administration in minipigs. Int J Pharm. 2020;590: 119889.
Papp K, Szepietowski JC, Kircik L, et al. Long-term safety and disease control with ruxolitinib cream in atopic dermatitis: results from two phase 3 studies [abstract no. 511 plus poster]. Br J Dermatol. 2021;185(3):e134–5.
Eichenfield LF, Simpson E, Papp K, et al. Long-term safety and disease control of ruxolitinib cream among adolescents with atopic dermatitis: results from two phase 3 studies [abstract no. 49]. Pediatric Dermatol. 2021;38(5):1433.
Papp K, Szepietowski JC, Kircik L, et al. Long-term safety and disease control with ruxolitinib cream in atopic dermatitis: results from two phase 3 studies. J Am Acad Dermatol. 2022. https://doi.org/10.1016/j.jaad.2022.09.060.
Papp K, Szepietowski JC, Kircik L, et al. Efficacy and safety of ruxolitinib cream for the treatment of atopic dermatitis: pooled analysis of two phase III, randomized, double-blind studies [abstract no. 337 plus poster]. Br J Dermatol. 2021;184(3):e62–3.
Blauvelt A, Kircik L, Papp KA, et al. Rapid pruritus reduction with ruxolitinib cream treatment in patients with atopic dermatitis. J Eur Acad Dermatol Venereol. 2022. https://doi.org/10.1111/jdv.18571.
Papp K, Szepietowski JC, Kircik L, et al. Efficacy of ruxolitinib cream for the treatment of atopic dermatitis by baseline patient demographics: pooled subgroup analysis from two randomized phase 3 studies [abstract no. 27496]. J Am Acad Dermatol. 2021;85(3 Suppl):AB149.
Simpson E, Lee M, Brar KK, et al. Efficacy of ruxolitinib cream in adults and adolescents with atopic comorbidities [abstract no. 329]. J Invest Dermatol. 2021;141(5 Suppl):S58.
Papp K, Szepietowski JC, Kircik L, et al. Efficacy of ruxolitinib cream for the treatment of atopic dermatitis by baseline clinical characteristics: pooled subgroup analysis from two randomized phase 3 studies [abstract no. 27716]. J Am Acad Dermatol. 2021;85(3 Suppl):AB160.
Simpson EL, Kircik L, Blauvelt A, et al. Effects of ruxolitinib cream in patients with atopic dermatitis with baseline body surface area ≥10% and Eczema Area and Severity Index score ≥16: pooled results from two phase 3 studies [abstract no. 27620]. J Am Acad Dermatol. 2021;85(3 Suppl):AB157.
Simpson E, Bissonnette R, Kuligowski ME, et al. Effects of ruxolitinib cream in patients with atopic dermatitis with head and/or neck involvement [abstract no. 311]. J Invest Dermatol. 2021;141(5 Suppl):S55.
Blauvelt A, Eichenfield LF, Kuligowski ME, et al. Efficacy of ruxolitinib cream among patients with atopic dermatitis based on previous medication history: pooled results from two phase 3 studies [abstract no. 27482]. J Am Acad Dermatol. 2021;85(3 Suppl):AB148.
Simpson EL, Kircik L, Blauvelt A, et al. Efficacy of ruxolitinib cream in patients with atopic dermatitis who demonstrated partial responses: pooled analysis from two randomized phase 3 studies [abstract no. 24916]. J Am Acad Dermatol. 2021;85(3 Suppl):AB50.
Blauvelt A, Eichenfield LF, Kuligowski ME, et al. Long-term safety and disease control with ruxolitinib cream in patients with atopic dermatitis based on previous medication history: pooled results from two phase III studies [abstract no. 515]. Br J Dermatol. 2021;185(3):e136–7.
Simpson EL, Kircik L, Blauvelt A, et al. Long-term safety and disease control with ruxolitinib cream in patients with more severe atopic dermatitis: pooled results from two phase III studies [abstract no. 513]. Br J Dermatol. 2021;185(3):e135–6.
Papp K, Szepietowski JC, Kircik L, et al. Long-term safety and disease control with ruxolitinib cream in atopic dermatitis: pooled results from two phase 3 studies [abstract no. 94 plus poster]. Exp Dermatol. 2021;30(Suppl 2):43.
Blauvelt A, Szepietowski JC, Papp K, et al. Itch-free state in patients with atopic dermatitis treated with ruxolitinib cream: pooled analysis from two randomized phase 3 studies. J Am Acad Dermatol. 2022. https://doi.org/10.1016/j.jaad.2022.09.010.
Bloudek L, Eichenfield LF, Silverberg JI, et al. Impact of ruxolitinib cream on work productivity and activity impairment and associated indirect costs in patients with atopic dermatitis: pooled results from two phase III studies. Am J Clin Dermatol. 2022. https://doi.org/10.1007/s40257-022-00734-8.
US National Institutes of Health. ClinicalTrials.gov identifier NCT03745638. 2021. https://clinicaltrials.gov/. Accessed 28 Nov 2022.
US National Institutes of Health. ClinicalTrials.gov identifier NCT03745651. 2021. https://clinicaltrials.gov/. Accessed 28 Nov 2022.
Acknowledgements
During the peer review process, the manufacturer of ruxolitinib cream 1.5% was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and Conflict of interest
Sheridan M. Hoy is a salaried employee of Adis International Ltd/Springer Nature, and declares no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent to publish, Availability of data and material, Code availability
Not applicable.
Additional information
The original online version of this article was revised due to retrospective open access request.
The manuscript was reviewed by: E. M. Altman, Department of Dermatology, University of New Mexico, Albuquerque, NM, USA; J. C. Szepietowski, Department of Dermatology, Venereology and Allergology, Wrocław Medical University, Wrocław, Poland.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hoy, S.M. Ruxolitinib Cream 1.5%: A Review in Mild to Moderate Atopic Dermatitis. Am J Clin Dermatol 24, 143–151 (2023). https://doi.org/10.1007/s40257-022-00748-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-022-00748-2