Abstract
Purpose
Our study investigated the association between dental caries, periodontal diseases, and tooth loss with diabetes mellitus (DM) among the elderly population, representing the first study of its kind in Iran.
Methods
This was a cross-sectional community-based study as a part of the second wave of the Birjand longitudinal aging study (BLAS, 2021–2022) for people older than 60. We used the Comprehensive Geriatric Oral Health Assessment Tool (CGOHAT) for the oral health evaluation. Participants were initially categorized into diabetic and non-diabetic groups. Those patients with DM were further categorised into uncontrolled and controlled diabetes based on their HbA1c level. The association between periodontitis, gingivitis, and edentulism with type II diabetes mellitus and uncontrolled diabetes was assessed using logistic regression.
Results
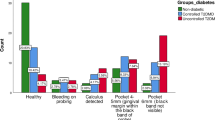
Among the 1,011 participants, 324 (32.04%) had DM. The mean ± SD DMFT was 27.06 ± 7.71 and 27.07 ± 7.72 among those with and without DM, respectively (p = 0.976). The M index comprised 85.46% of the total DMFT among those without DM and 84.51% among those with DM. The prevalence of periodontitis was higher among those without DM (110, 32.84%, p = 0.390). The prevalence of gingivitis was higher among those with DM (73, 45.06%, p = 0.617). Among the diabetic group, 137 (42.28%) had controlled DM. Based on the adjusted matched multivariate logistic model, decayed teeth (1.24, 95%CI: 1.06 – 1.46, p-value = 0.006), periodontitis (2.78, 95%CI: 1.02 – 7.56, p-value = 0.044), and moderate tooth loss (5.73, 95%CI: 1.13 – 28.88, p-value = 0.034) were significantly associated with increased odds of uncontrolled DM.
Conclusions
Based on the findings of this study, tooth loss was highly prevalent among the elderly Iranians regardless of their diabetes status. Also, periodontitis, tooth loss, and decayed teeth were significantly associated with increased odds of poor glycemic control among those with DM. Thus, it can be concluded that improving the oral health of the geriatric population may be a crucial part of improving the glycemic control among those with diabetes which has been frequently neglected.



Similar content being viewed by others
Data Availability
Data is available upon request from the corresponding authors.
References
Cheng X, et al. Population ageing and mortality during 1990–2017: A global decomposition analysis. PLoS Med. 2020;17(6):e1003138.
World Health Organization, WHO. Ageing and Health. 2022 [cited 2024 March 16]; Available from: World Health Oragnization, URL: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
Noroozian M. The elderly population in iran: an ever growing concern in the health system. Iran J Psychiatry Behav Sci. 2012;6(2):1–6.
Safarkhanlou H, RezaeiGhahroodi Z. Changes in the elderly population in Iran and worldwide. srtc-amar. 2017;5(3):8–16.
Dziechciaż M, Filip R. Biological psychological and social determinants of old age: bio-psycho-social aspects of human aging. Ann Agric Environ Med. 2014;21(4):835–8.
Fajemiroye JO, et al. Aging-induced biological changes and cardiovascular diseases. Biomed Res Int. 2018;2018:7156435.
Persson GR. Dental geriatrics and periodontitis. Periodontol 2000. 2017;74(1):102–15.
Liljestrand JM, et al. missing teeth predict incident cardiovascular events, diabetes, and death. J Dent Res. 2015;94(8):1055–62.
NeshandarAsli H, et al. At what age do people in iran use complete denture for the first time? A cross-sectional study within a 10-year period. Gums-dent. 2018;7(4):167–72.
Rabiei M, et al. Dental status of the Iranian elderly: A systematic review and meta-analysis. J Investig Clin Dent. 2019;10(4):e12459.
Soltani MR, et al. Dental caries status and its related factors in Iran: a meta-analysis. J Dent (Shiraz). 2020;21(3):158–76.
Shoaee S, et al. Trends in dental caries of deciduous teeth in Iran: a systematic analysis of the national and sub-national data from 1990 to 2017. BMC Oral Health. 2022;22(1):634.
Khoshnevisan M, Ghasemianpour M, Samadzadeh H, Baez R. Oral health status and healthcare system in IR Iran. J Contemp Med Sci. 2018;4(3):107–8.
Shoaee S, Masinaei M, Moghaddam SS, Sofi-Mahmudi A, Hessari H, Shamsoddin E, Heydari MH, Larijani B, Fakhrzadeh H, Farzadfar F. National and subnational trend of dental caries of permanent teeth in Iran, 1990–2017. Int Dent J. 2024;74(1):129–37.
Shoaee S, et al. Dental caries among the elderly in Iran: a meta-analysis. MJIRI. 2024;38(1):57–67.
Takeda M, et al. Combined association of oral and skeletal muscle health with type 2 diabetes mellitus among community-dwelling older adults in Japan: a cross-sectional study. J Rural Med. 2022;17(2):67–72.
Kim YR, Son M, Nam SH. Association between depressive mood and chronic periodontitis among senior residents using the National Health Insurance Service‐Senior Cohort Database. J Periodontol. 2023;94(6):742–50.
Kim SR, Son M, Kim YR. The risk of stroke according to statin medication compliance in older people with chronic periodontitis: an analysis using the Korea National Health Insurance Service-Senior Cohort Database. Epidemiol Health. 2022;44:e2022055.
Kim HS, et al. Association between the severity of periodontitis and osteoarthritis in middle-aged and older patients with type 2 diabetes mellitus: a nationwide population-based study. Arthritis Care Res (Hoboken). 2022;74(3):403–9.
Heydari M-H, et al. Prevalence, trend, and associated risk factors for cleft lip with/without cleft palate: a national study on live births from 2016 to 2021. BMC Oral Health. 2024;24(1):36.
Kapila YL. Oral health’s inextricable connection to systemic health: Special populations bring to bear multimodal relationships and factors connecting periodontal disease to systemic diseases and conditions. Periodontol 2000. 2021;87(1):11–6.
Botelho J, et al. An umbrella review of the evidence linking oral health and systemic noncommunicable diseases. Nat Commun. 2022;13(1):7614.
Leung WK, et al. Health behaviour, metabolic control and periodontal status in medically treated Chinese with type 2 diabetes mellitus. Ann R Australas Coll Dent Surg. 2008;19:102–10.
Nasution DLI, et al. Longitudinal association between periodontal condition and glycaemic status in middle-aged adults: A cross-lagged panel analysis. J Clin Periodontol. 2023;50(8):1042–50.
Jafer M. The periodontal status and associated systemic health problems among an elderly population attending the outpatient clinics of a dental school. J Contemp Dent Pract. 2015;16(12):950–6.
Li J, et al. Periodontitis in elderly patients with type 2 diabetes mellitus: impact on gut microbiota and systemic inflammation. Aging (Albany NY). 2020;12(24):25956–80.
Portes J, et al. Prevalence of undiagnosed diabetes and prediabetes related to periodontitis and its risk factors in elderly individuals. J Dent. 2023;132:104480.
Weijdijk LPM, et al. The risk of tooth loss in patients with diabetes: A systematic review and meta-analysis. Int J Dent Hyg. 2022;20(1):145–66.
Kim OS, et al. The severity of periodontitis and metabolic syndrome in Korean population: The Dong-gu study. J Periodontal Res. 2018;53(3):362–8.
Simpson TC, et al. Treatment of periodontitis for glycaemic control in people with diabetes mellitus. Cochrane Database Syst Rev. 2022;4(4):Cd004714.
Schroeder SM, Adamsen C, Besse R. The relationship between diabetes and oral health status, and dental visits among American Indian, Alaska Native, and Native Hawaiian elders. J Am Dent Assoc. 2021;152(4):293–301.
Abe T, et al. Number of teeth and masticatory function are associated with sarcopenia and diabetes mellitus status among community-dwelling older adults: A Shimane CoHRE study. PLoS ONE. 2021;16(6):e0252625.
Yoo JJ, et al. The effect of diabetes on tooth loss caused by periodontal disease: A nationwide population-based cohort study in South Korea. J Periodontol. 2019;90(6):576–83.
Moodi M, et al. Birjand longitudinal aging study (BLAS): the objectives, study protocol and design (wave I: baseline data gathering). J Diabetes Metab Disord. 2020;19(1):551–9.
Shoaee S, Heydari MH, Hessari H, Mehrdad N, Khalilazar L, Hatami B, Sharifi F. Development and initial validation of the comprehensive geriatric Oral health assessment tool. Clin Exp Dent Res. 2023;9(5):879–86.
Shoaee S, et al. Experiences from the management of COVID-19 pandemic in a nursing home in Iran (March–April, 2020). J Diabetes Metab Disord. 2022;21(1):1195–9.
Salomon JA, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. The Lancet. 2012;380(9859):2129–43.
Locker D, Slade G. Measuring oral health and quality of life. Chapel Hill: University of North Carolina; 1997.
Kimmie-Dhansay F, Pontes CC, Chikte UM, Chinhenzva A, Erasmus RT, Kengne AP, Matsha TE. Impacts of tooth loss on OHRQoL in an adult population in Cape Town, South Africa. Int J Environ Res Public Health. 2021;18(9):4989.
Stuart EA, King G, Imai K, Ho D. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011.
Moscowchi A, Moradian-Lotfi S, Koohi H, Sarrafan Sadeghi T. Levels of smoking and outcome measures of root coverage procedures: a systematic review and meta-analysis. Oral Maxillofac Surg. 2023;(2):1–3.
Wagner J, et al. Systematic review on diabetes mellitus and dental implants: an update. Int J Impl Dent. 2022;8(1):1.
Zhu Z, et al. Age differences in the effects of multi-component periodontal treatments on oral and metabolic health among people with diabetes mellitus: A meta-epidemiological study. J Dent. 2023;135:104594.
Nikbin A, et al. Oral health-related quality of life in diabetic patients: comparison of the Persian version of Geriatric Oral Health Assessment Index and Oral Health Impact Profile: A descriptive-analytic study. J Diabetes Metab Disord. 2014;13(1):32.
MohseniHomagarani Y, et al. The effect of diabetes mellitus on oral health-related quality of life: A systematic review and meta-analysis study. Front Public Health. 2023;11:1112008.
Azami-Aghdash S, et al. Oral health and related quality of life in older people: a systematic review and meta-analysis. Iran J Public Health. 2021;50(4):689.
Kakooei S, et al. The knowledge and attitude of diabetic patients regarding oral and dental disorders in Kerman diabetes clinics. J Dent. 2020;21(3):195.
Poursadeqiyan M, Arefi MF, Pouya AB, Jafari M. Quality of life in health Iranian elderly population approach in health promotion: a systematic review. J Educ Health Promot. 2021;10(1).
Tolou AF, Jadidfard MP, Ghasemi H, Boroumand F, Namdari M, Khoshnevisan MH. Influential factors on oral health status of the elderly iranians: a path analysis. J Contemp Med Sci 2022;8(3).
Ayoobi F, et al. Dyslipidemia, diabetes and periodontal disease, a cross-sectional study in Rafsanjan, a region in southeast Iran. BMC Oral Health. 2023;23(1):549.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical consideration
This study was approved by the ethical committee of Shahid Beheshti University of Medical Sciences and Tehran University of Medical Sciences (IR.SBMU.DRC.REC.1420.060). Informed consent was obtained from all the participants in BLAS prior to any examination.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Heydari, MH., Sharifi, F., Sobhaninejad, S. et al. The association between dental caries, periodontal diseases, and tooth loss with diabetes mellitus among the elderly population. J Diabetes Metab Disord (2024). https://doi.org/10.1007/s40200-024-01434-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40200-024-01434-2