Abstract
Background
Diabetes is a prevalent chronic disease. Although self-care is the crucial element in managing diabetes, older Korean immigrants with diabetes face challenges in performing effective self-care related to vulnerability as minority immigrants.
Purpose
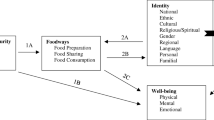
This study measures sociodemographics, self-efficacy, social support, diabetes knowledge, and diabetes self-care activities among older Korean immigrants in the United States. This study also aims to demonstrate the direct and indirect effects of the related factors on diabetes self-care activities using a path analysis.
Methods
This study uses a cross-sectional design. Convenience sampling targeted Korean immigrants aged 55 or older using paper and online surveys. Four instruments were used to measure variables: self-efficacy was measured by the General Self-Efficacy scale, diabetes knowledge by the Simplified Diabetes Knowledge Test, social support by the Lubben Social Network Scale-6, and diabetes self-care by the Summary of Diabetes Self-Care Activities questionnaire. Using path analysis, the effects of related factors on self-care activities were analyzed.
Results
190 older Korean immigrants participated, 53.2% female, and 46.8% male. The mean age was 67.2 (SD = 9.9; range, 58–93). A path model shows that sociodemographics (sex, age, education, and years in the United States), diabetes knowledge, self-efficacy, and family support predict diabetes self-care.
Conclusions
The path model demonstrates the effects of sociodemographics, self-efficacy, diabetes knowledge, and social support on diabetes self-care among older Korean immigrants. The findings can help to understand diabetes self-care among the minority ethnic older group and can be used to develop culturally tailored education, counseling, and healthcare services.

Similar content being viewed by others
References
Centers for Disease Control and Prevention. National diabetes statistics report. 2022. https://www.cdc.gov/diabetes/data/statistics-report/index.html.
Sinclair AJ, Abdelhafiz AH. Challenges and strategies for diabetes management in community-living older adults. Diabetes Spectr. 2020;33(3):217–27. https://doi.org/10.2337/ds20-0013.
Centers for Disease Control and Prevention. Diabetes complications are costly in older adults. 2022. https://www.cdc.gov/diabetes/resources-publications/research-summaries/diabetes-complications-costly.html#:~:text=Early%20diagnosis%20and%20treatment%20of,older%20with%20type%202%20diabetes.
Saunders T. Type 2 Diabetes self-management barriers in older adults. J Gerontol Nurs. 2019;45(3):43–54.
Freeman J. Management of hypoglycemia in older adults with type 2 Diabetes. Postgrad Med. 2019;131(4):241–50. https://doi.org/10.1080/00325481.2019.1578590.
Kristianingrum ND, Wiarsih W, Nursasi AY. Perceived family support among older persons in diabetes mellitus self-management. BMC Geriatr. 2018;18(Suppl 1):1–6. https://doi.org/10.1186/s12877-018-0981-2.
Weinger K, Beverly EA, Smaldone A. Diabetes self-care and the older adult. West J Nurs Res. 2015;36(9):1272–98. https://doi.org/10.1177/0193945914521696.
American Diabetes Association. Older adults: standards of medical care in diabetes. Diabetes Care. 2018;41(1):119–s125. https://doi.org/10.2337/dc21-S012.
Trevizani FA, Doreto DT, Lima GS, Marques S. Self-care activities, sociodemographic variables, treatment and depressive symptoms among older adults with diabetes mellitus. Revista Brasileira De Enfermagem. 2019;72:22–9. https://doi.org/10.1590/0034-7167-2017-0579.
Borba AKOT, Arruda IKG, Marques APO, Leal MCC, Diniz AS. Knowledge and attitude about diabetes self-care of older adults in primary health care. Ciencia E Saude Coletiva. 2019;24(1):125–36. https://doi.org/10.1590/1413-81232018241.35052016.
Seah SJ, Harding SC, Pay JY, Wang J, Aw S, Lam J, Lim RBT. Sociodemographic characteristics associated with self-care and quality of life among community-dwelling older adults with type 2 diabetes. Prim Care Diabetes. 2022;16(1):179–87. https://doi.org/10.1016/j.pcd.2021.12.011.
Seyyedrasooli A, Parvan K, Valizadeh L, Rahmani A, Zare M. Self-efficacy in foot-care and effect of training: a single-blinded randomized controlled clinical trial. J Community Based Nurs Midwifery. 2015;3(2).
Migration Information Source. Korean immigrants in the United States. 2014. https://www.migrationpolicy.org/article/korean-immigrants-united-states-2013.
Han H-R, Kim J, Kim MT, Kim KB. Measuring health literacy among immigrants with a phonetic primary language: a case of Korean American women. J Immigr Minor Health. 2011;13(2):253–9. https://doi.org/10.1007/s10903-010-9366-0.
Song Y, Song H-J, Han H-R, Park S-Y, Nam S, Kim MT. Unmet needs for social support and effects on Diabetes self-care activities in Korean americans with type 2 diabetes. Diabetes Educ. 2012;38(1):77–85. https://doi.org/10.1177/0145721711432456.
Choi S, Rush E. Effect of a short-duration, culturally tailored, community-based diabetes self-management intervention for Korean immigrants. Diabetes Educ. 2012;38(3):377–85. https://doi.org/10.1177/0145721712443292.
Kwon YE, Kim YS. Factors related to self-management the elderly people with diabetes mellitus in a community-dwelling. J Korean Soc Living Environ Sys. 2011;18(1):92–100.
Primozic S, Tavcar R, Avbelj M, Dernovsek MZ, Oblak MR. Specific cognitive abilities are associated with Diabetes self-management behavior among patients with type 2 diabetes. J Diabetes Res. 2012;95(1):48–54. https://doi.org/10.1016/j.diabres.2011.09.004.
Choi GA, Jang SM, Nam HW. Current status of self-management and barriers in senior diabetic patient. J Korean Diabetes. 2008;32(3):280–9. https://doi.org/10.4093/kdj.2008.32.3.280.
Orem DE, Nursing. Concepts of practice. 4th ed. St. Louis, MO: Mosby-Year Book Inc.; 1991.
Munro B. Statistical methods for health care research. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.
Jöreskog KG, Sőrbom D. LISREL 10 for Windows (10.3.3.26). Lincolnwood, IL: Scientific Software International, Inc.; 2018.
Schwarzer R, Jerusalem M. Generalized self-efficacy scale. Measures in health psychology: a user’s portfolio. Causal and control beliefs. Berkshire, UK: NFER-NELSON; 1995. pp. 35–7.
Fitzgerald JT, Funnell MM, Hess GE, Barr PA, Anderson RM, Hiss RG, Davis WK. The reliability and validity of a brief Diabetes knowledge test. Diabetes Care. 1998;21(5):706–10. https://doi.org/10.2337/diacare.21.5.706.
Lubben J, Gironda M. Centrality of social ties to the health and wellbeing of older adults. In: Berkman LF, Harootyan L, editors. Social work and health care in an aging society. New York: Springer; 2003. pp. 319–50.
Lubben J. Assessing social networks among senior populations. Fam Community Health. 1988;11(3):42–52. https://doi.org/10.1097/00003727-198811000-00008.
Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109(2):186–204. https://doi.org/10.1093/oxfordjournals.aje.a112674.
Lubben J, Blozik E, Gillmann G, Iliffe S, von Renteln-Kruse W, Beck J, Stuck A. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist. 2006;46(4):503–13. https://doi.org/10.1093/geront/46.4.503.
Hong M, Casado BL, Harrington D. Validation of Korean versions of the Lubben Social Network Scales in Korean americans. Clin Gerontol. 2011;34(4):319–34. https://doi.org/10.1080/07317115.2011.572534.
Kamradt M, Bozorgmehr K, Krisam J, Freund T, Kiel M, Qreini M, Flum E, Berger S, Besier W, Szecsenyi J, Ose D. Assessing self-management in patients with Diabetes Mellitus type 2 in Germany: validation of a German version of the Summary of Diabetes Self-Care activities measure (SDSCA-G). Health Qual Life Outcomes. 2014;12(1). https://doi.org/10.1186/s12955-014-0185-1.
Toobert DJ, Glasgow RE. Assessing Diabetes self-management: the summary of Diabetes self-care activities questionnaire. In: Bradley C, editor. Handbook of psychology and Diabetes. Reading, UK: Harwood Academic; 1994. pp. 351–75.
Choi EJ, Nam M, Kim SH, Park CG, Toobert DJ, Yoo JS, Chu SH. Psychometric properties of a Korean version of the summary of Diabetes self-care activities measure. Int J Nurs Stud. 2011;48(3):333–7. https://doi.org/10.1016/j.ijnurstu.2010.08.007.
David D, Dalton J, Magny-Normilus C, Brain MM, Linster T, Lee SJ. The quality of family relationships, Diabetes self-care, and health outcomes in older adults. Diabetes Spectr. 2019;32(2):132–8. https://doi.org/10.2337/ds18-0039.
D’Souza MS, Karkada SN, Parahoo K, Venkatesaperumal R, Achora S, Cayaban ARR. Self-efficacy and self-care behaviours among adults with type 2 Diabetes. Appl Nurs Res. 2017;36:25–32. https://doi.org/10.1016/j.apnr.2017.05.004.
Lee YJ, Shin SJ, Wang RHEA. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 Diabetes Mellitus. Patient Educ Couns. 2016;99(2):287–94.
Yao J, Wang H, Yin X, Yin J, Guo X, Sun Q. The association between self-efficacy and self-management behaviors among Chinese patients with type 2 Diabetes. PLoS ONE. 2019;14(11):e0224869. https://doi.org/10.1371/journal.pone.0224869.
Fan L, Sidani S, Cooper-Brathwaite A, Metcalfe K. Feasibility, acceptability and effects of a foot self care educational intervention on minor foot problems in adult patients with Diabetes at low risk foot ulceration: a pilot study. Can J Diabetes. 2013;37:195–201. https://doi.org/10.1016/j.jcjd.2013.03.020.
Hu J, Gruber KJ, Liu H, Zhao H, Garcia AA. Diabetes knowledge among older adults with Diabetes in Beijing, China. J Clin Nurs. 2013;22(1–2):51–60. https://doi.org/10.1111/j.1365-2702.2012.04273.x.
Strom JL, Egede LE. (2012). The impact of social support on outcomes in adult patients with type 2 diabetes: A systematic review. Curr Diab Rep. 2012;12(6):769–781. https://doi.org/10.1007/s11892-012-0317-0.
Paddison C. Family support and conflict among adults with type 2 Diabetes. J Diabetes Nurs. 2010;7:29–33.
Rintala T-M, Jaatinen P, Paavilainen E, Åstedt-Kurki P. Interrelation between adult persons with Diabetes and their family: a systematic review of the literature. J Fam Nurs. 2013;19(1). https://doi.org/10.1177/1074840712471899.
Heiss VJ, Petosa RL. Social cognitive theory correlates of moderate-intensity exercise among adults with type 2 Diabetes. Psychol Health Med. 2016;21(1):92–101. https://doi.org/10.1080/13548506.2015.1017510.
Rachmah Q, Setyaningtyas SW, Rifqi MA, Indriani D, Nindya TS, Megatsari H, Mahmudiono T, Kriengsinyos W. Self-efficacy to engage in physical activity and overcome barriers, sedentary behavior, and their relation to body mass index among elderly indonesians with Diabetes. J Prev Med Public Health. 2019;52(4):242–9. https://doi.org/10.3961/jpmph.19.003.
Vanden Bosch ML, Robbins LB, Anderson K. Correlates of physical activity in middle-aged women with and without Diabetes. West J Nurs Res. 2015;37(12):1581–603. https://doi.org/10.1177/0193945914541333.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. https://doi.org/10.1037/0033-295X.84.2.191.
Gökdeniz D, Akgün Şahin Z. Evaluation of knowledge levels about Diabetes foot care and self-care activities in diabetic individuals. Int J Low Extrem Wounds. 2022;21(1):65–74. https://doi.org/10.1177/1534734620926266.
Coelho ACM, Boas LCGV, Gomides DdS, Foss-Freitas MC, Pace AE. Self-care activities and their relationship to metabolic and clinical control of people with Diabetes Mellitus. Texto E Contexto Enfermagem. 2015;24(3):697–705. https://doi.org/10.1590/0104-07072015000660014.
Acknowledgements
The content is the sole responsibility of the authors and does not necessarily represent the official position of any other entity. There are no conflicts of interest to report by the authors.
Funding
There is no funding or grant for this research.
Author information
Authors and Affiliations
Contributions
Conceptualization or/and Methodology: Kim, JE/ Jiang, YH/ Dee, V. Data curation or/and Analysis: Kim, JE/ Jiang, YH. Funding acquisition: None. Investigation: Kim, JE. Project administration or/and Supervision: Kim, JE/ Dee, V. Resources or/and Software: Kim, JE. Validation: Kim, JE/ Jiang, YH. Visualization: Kim, JE. Writing: original draft or/and review & editing: Kim, JE/ Jiang, YH/ Dee, V.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants complied with ethical requirements. The research was approved by the authors’ University’s Institutional Review Board (IRB). All participants were informed of the purpose, risks, benefits, and rights to confidentiality and withdrawal from the study. All participants in this study provided their consent after being fully informed.
Conflict of interests
The authors have no financial or nonfinancial interests that are directly or indirectly related to the work submitted for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, J.E., Jiang, Y. & Dee, V. Implications on self-care behaviors among older Korean immigrants diagnosed with diabetes residing in the United States: a path analytical approach. J Diabetes Metab Disord (2023). https://doi.org/10.1007/s40200-023-01363-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40200-023-01363-6