Abstract
Purpose
There are limited studies on factors that impacted retina clinic patient outcomes during the COVID-19 pandemic. We aimed to evaluate visual and anatomic outcomes in patients with diabetic macular edema (DME) requiring anti-VEGF injections at the veterans’ affairs tertiary care eye clinic in Houston, TX.
Methods
Patient volume from April 2020 was compared to that of April 2019 to determine attendance changes. To evaluate outcomes, we reviewed patients with DME who had scheduled appointments during April 2020. We tracked changes in central foveal thickness (CFT) and Snellen visual acuity (VA) measurements. Patient outcomes were classified as poor (defined as worsening VA or CFT at follow-up) or good (no worsening of either at follow-up). Regression analysis identified characteristics associated with poor outcomes.
Results
To prevent the spread of COVID-19, patients were called to reschedule clinic appointments. Attendance frequency decreased from 523 patients in April 2019 to 246 patients in April 2020. 134 patients met inclusion criteria (mean age of 64.7 ± 8.8 years). 19/134 of patients were seen on schedule, 89/134 had delayed appointments (average follow-up interval of 115.2 ± 50.0 days), and 26/134 were lost to follow-up. Patients with delayed appointments had higher odds of poor outcome at follow-up compared to patients seen on schedule (OR = 4.03, 95% CI: 1.14–16.92, p = 0.04). Patient’s baseline visual acuity, macular thickness, comorbidities, and diabetic retinopathy severity, and demographics did not affect visual outcome at follow-up.
Conclusions
On average, patients were rescheduled to a visit 2.4 months later than their usual visit. Over half these patients experienced worsening of vision or edema. This demonstrates that lapses in care result in worsening of DME. However, there is no clear association between baseline characteristics and risk of disease progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately one in three patients with diabetes will develop diabetic retinopathy, and diabetic macular edema (DME) is one of the vision-threatening sequalae [1]. DME affects approximately 21 million people worldwide [2] and is a leading cause of preventable blindness among working-age adults in the United States [3]. Intravitreal injections with anti-vascular endothelial growth factor (VEGF) agents mitigate vision loss in DME, but patient adherence to injection schedules is important to ensure best treatment outcomes [4].
Patient volumes at hospital and outpatient settings in the United States saw significant decreases after COVID-19 was declared a national emergency in mid-March 2020, with the sharpest declines in the immediately following weeks [5, 6]. Similarly, retina clinics within the country also experienced a decrease in both the number of patient visits and number of intravitreal injections performed [7].
Suggestions for adapting intravitreal injection scheduling included increasing the intervals between injections or the use of treatment priority levels [8, 9]. Certain ophthalmology centers limited in person intravitreal injections to just patients with high risk of vision loss, which reduced patient volume and risk of COVID-19 transmission [10].
Studies have been published showing that COVID-19 related delays in treatment were associated with worsened visual acuity and macular thickness among patients undergoing anti-VEGF injections [11, 12]. Our study is unique in that we strictly focus on outcomes among patients with diabetic macular edema, whereas the aforementioned studies include all categories of patients requiring anti-VEGF injections (e.g. neovascular age related macular degeneration, retinal vein occlusions) Furthermore, our study focuses on a patient population at a tertiary care veterans affairs hospital, a population which is on average older, and therefore at higher risk of COVID-19 related complications and also at a higher risk of health disparities compared to the general population [13].
Our study was performed at a retina injection clinic located within a tertiary care veterans’ affairs hospital in Houston, Texas. The aims of our study were to: 1) determine difference in clinic volumes pre and post COVID-19 related restrictions; 2) determine visual and anatomical outcomes among patients with diabetic macular edema; and 3) identify patient characteristics associated with poor visual and anatomical outcomes following a delay in injection appointments.
Methods
This study adheres to the tenets of the Declaration of Helsinki and was approved by the Baylor College of Medicine and the Veterans Affairs Institutional Review Board. Informed consent was waived by the institutional review board as the data were collected retrospectively.
Study population
This retrospective study included patients aged 18 and older who had appointments at Michael E. DeBakey Veterans Affairs Medical Center’s retina injection clinic from April 1, 2020 to April 30, 2020. The number of patient appointments at the retina clinic was also recorded for April 1, 2019 to April 30, 2019 in order to compare patient volumes. April was chosen because the retina injection clinic had fully adopted recommendations for rescheduling visits by the beginning of April 2020.
Study design
Study data were obtained from the Computerized Patient Record System (CPRS), which is the electronic medical record used throughout the veterans’ affairs medical systems. ICD-10 diagnosis codes were used to identify patients who had diabetic macular edema. We reviewed physician notes to confirm the diagnosis and identify patients undergoing injections.
Optical coherence tomography (OCT) images were used to determine macular edema. Visit information was obtained for baseline (defined as the most recent visit prior to COVID -19 restrictions i.e. visit between January 1, 2020 to March 31,2020) and follow-up (defined as the patient’s return to clinic between April 1, 2020 to December 1, 2020) periods to determine the changes in visual acuity and foveal thickness.
Inclusion and exclusion criteria
Patients were included for the final analysis if they 1) had a diagnosis of DME; 2) had an anti-VEGF injection within the 3 months prior to and including their baseline visit; 3) had at least one visit each during the baseline and follow-up intervals. We excluded patients if they had any eye surgery or steroid injections within the 3 months prior to or at the baseline and follow-up visits.
Data collection
The following parameters were recorded for each patient included in this study: age, sex, Snellen VA with correction and pinhole, DR grade, anti-VEGF injection dates, past eye history, procedures in past 3 months, baseline visit date, if the patient underwent rescheduling, follow-up visit date, days between visits, baseline OCT image date, follow-up OCT image date, and central 1 mm foveal thickness (CFT).
Snellen VA was measured as the last line read correctly with refractive correction on a Snellen chart. OCT (Spectralis, Heidelberg Engineering) was used to determine CFT, the values of which were measured automatically by the Heidelberg Eye Explorer (HEYEX) software. Snellen VA and CFT were recorded for both baseline and follow-up periods.
In our clinic, OCT imaging is typically not performed at every visit. In the study population, the image taken closest to the visit date was selected for analysis as long as the image was within 3 months of the visit date.
Measurement of outcomes
For retina clinic attendance frequency, “appointments kept” was defined as the number of patients who presented to the clinic for their scheduled appointment in April. “Cancellations” indicates the number of patients who originally had appointment(s) scheduled during April, but these appointment(s) were cancelled by either the retina clinic or the patient prior to the appointment date(s). “No shows” indicates the number of patients who did not present to the clinic and did not cancel their appointment(s) prior.
Outcome analysis focused on changes in VA and retinal thickness in the interval between visits. For Snellen VA measurements, a gain of 1 line or more from baseline to follow-up was considered “improved” and loss of 1 line or more was considered “worsened.” VA outcomes were categorized as “stable” if the VA measurements changed by less than 1 line of vision. Edema outcomes were also categorized as by comparing the CFT values between the baseline and follow-up. A decrease in CFT value of 10% or more from baseline to follow-up was categorized as “improved,” and an increase of 10% or more was categorized as “worsened.” Stable edema was defined as a change of less than 10%.
Poor outcome for a patient was defined as having any worsening (either in VA or edema or both) at follow-up. Good outcome was defined as having no worsening at follow-up. If a patient was being treated for both eyes, the eye with the worse VA was included for analysis.
Statistical analysis
Patient demographics and clinic characteristics were summarized by either a) median with 25th and 75th percentiles, b) mean with standard deviation or c) frequencies with percentages. Wilcoxon rank sum test or Pearson Chi-square test were used to determine if there was significant difference between patients who had on-schedule appointments and patients who had delayed appointments.
To identify baseline characteristics significantly associated with follow-up VA and follow-up CFT, we used simple linear regression. Multiple linear regression was used to determine whether the baseline characteristics identified were significantly associated with outcomes after adjusting for the number of weeks between appointments and other significant factors.
Univariable logistic regression was used to identify baseline characteristics associated with worse outcomes. Multivariable logistic regression was used to identify baseline characteristics significantly associated with worse outcomes after adjusting for time between appointments and other significant factors. A significance level of 0.05 was used for all analyses.
Results
Change in retina clinic attendance rates
The World Health Organization declared COVID-19 a global pandemic in mid-March [14], and our eye clinic quickly adopted changes to reschedule patients to prevent the spread of COVID-19. At provider discretion, patients were called to postpone appointments. This contributed to a drastic decline in appointment attendance rates at our clinic. In the retina clinic, overall appointment attendance for all visits was lower in April 2020 compared to April 2019 (Fig. 1).
In April 2020, there was a 53.0% decrease in appointments kept and an 84.8% increase in cancellations or no shows compared to April 2019. 694 patients had an appointment scheduled at the retina clinic in April 2019: 75.4% (523/694) of patients kept their April appointment, and 24.6% (171/694) patients canceled or were no shows. 562 patients had an appointment scheduled in April 2020: 43.8% (246/562) of patients kept their appointment, and 56.2% (316/562) patients canceled or were no shows.
Cohort selection
562 unique patients had appointments scheduled at the retina clinic between April 1 and April 30, 2020 (Fig. 2). Of these, 32.9% (185/562) had diagnoses of DME. 27.6% of these (51/185) were excluded because they did not receive an injection within 3 months of their pre-COVID baseline visits or had undergone ocular surgeries or steroid injections within the past 3 months. Of the remaining 134 patients, 66.4% (89/134) were rescheduled and seen for follow-up at a delayed appointment date and 14.2% (19/134) were seen at their originally scheduled appointment date. 19.4% (26/134) have been lost to follow-up until the end of our study period and were not included in the final analysis. 108 patients with DME had complete clinical information and OCT imaging available from both baseline and follow-up periods and were included in the final analysis.
Study participants
Table 1 shows the baseline characteristics of the patients in the delayed appointment group (n = 89) and the on-schedule appointment group (n = 19). For the baseline measurements of most patients (78.0%), the anti-VEGF injection date, VA measurement date, and OCT imaging date were the same. However, some patients (22.0%) had their OCT images and VA measurements performed on different dates (average difference of 37.5 ± 22.6 days). At follow-up, most patients had their OCT imaging and VA measurement performed on the same date (93.6%). The remaining 6.4% had these performed on different dates (average difference of 40.4 ± 17.8 days). The delayed appointment group had an average follow-up interval (115.2 days) about 2.7 times longer than that of the on-schedule appointment group (42.3 days).
Table 1 summarizes the differences between patients who were rescheduled (and had a delayed appointment) and those who were seen on-schedule. Of the 26/134 patients who met inclusion criteria but were lost to follow-up, 23.1% (6/26) had mild NPDR, 42.3% (11/26) had moderate NPDR, 15.4% (4/26) had severe NPDR, and 19.2% (5/26) had PDR. 1 of the patients with PDR had received panretinal photocoagulation.
Comparison of visual and edema outcomes between the on schedule and delayed appointment groups
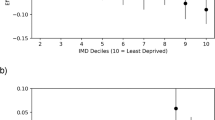
Descriptive statistics were used to compare the differences between the on-schedule group and delayed appointment group in terms of visual and edema outcomes. Figure 3a shows that the group of patients seen on schedule had a significantly higher proportion of patients with improved or stable edema compared to the group of patients whose appointments were delayed (94.7% (18/19) vs. 73.0% (65/89), p = 0.042). Figure 3b shows comparison of Snellen VA changes between the group of patients who were seen on-schedule and the group of patients whose appointments were delayed. No significant difference was found between the two groups when comparing proportions of patients with improved or stable VA (78.9%; 15/19 vs. 58.4%; 52/89, p = 0.094).
(A) Comparison of macular edema changes between the on-schedule and delayed appointment groups. A change in edema of 10% or more is considered significant and categorized as either “Improved” or “Worsened.” Changes of < 10% is categorized as “Stable.” (B) Comparison of Snellen VA changes between the on-schedule and delayed appointment groups. A gain of 1 line or more on Snellen VA chart is categorized as “Improved” and a loss of 1 line or more is considered “Worsened.” No change in lines is considered “Stable.” (C) Comparison of outcome between the on-schedule and delayed appointment groups. Poor outcome for a patient was defined as having worsened VA or worsened edema, or both at follow-up. Good outcome was defined as having neither worsened VA nor worsened edema at follow-up
Compared to the group seen on schedule, the group with delayed appointments had more than twice the proportion of patients with either worsening vision or increased edema at follow-up (54%; 48/89 vs 21%; 4/19, p = 0.009) (Fig. 3c).
Characteristics associated with poor outcomes
Analysis with multiple linear regression found that baseline VA was significantly associated with follow-up VA (p < 0.001) after adjusting for weeks between visits (Table 2). A 1 unit increase in baseline logMAR was associated with a 0.81 unit increase in follow-up VA (95% CI: 0.73, 0.90). Supplemental 1 shows that the association between baseline CFT and follow-up CFT depended on the number of weeks between appointments. Patients with longer intervals between baseline and follow-up appointments experienced greater increases in follow-up CFT per unit increase in baseline CFT compared to patients with shorter follow-up intervals. Two factors, the interaction between baseline CFT and length of follow-up (p = 0.033) and epiretinal membrane (p < 0.001), were significantly associated with increased CFT after adjustment (Table 3).
Table 4 shows the results of the univariable and multivariable regression models measuring the effect of each variable on the categorization of patient outcome. Compared to the group that was seen on schedule, the group that had appointment delays had significantly higher odds of poor outcome at follow-up (OR = 4.03, 95% CI 1.14–16.92, p = 0.039) after adjusting for the number of weeks between visits. No other factors were significant after adjustment.
Discussion
In our study, we found that the group of patients with delayed appointments experienced an average delay of 2.4 months later than their originally scheduled visit. This delay can be directly attributed to rescheduling of patient appointments to prevent the spread of COVID-19. Other potential factors also include patient hesitancy, or inability due to COVID related illness, to attend clinic visits in-person during the beginning of the pandemic. 54% of patients with delayed visits experienced a worsening of edema or visual acuity at follow-up. About one-fifth of the patients seen in our clinic had not yet returned for follow-up at the end of the study period. This is concerning as untreated macular edema may lead to persistent visual disability over time1. Long-term follow-up studies are needed to determine to what degree re-institution of delayed anti-VEGF treatment can restore vision and lead to resolution of macular edema. Additionally, PDR was diagnosed in about a fifth of patients who were still lost to follow-up at the end of the study, highlighting the importance of PRP vs monthly anti-VEGF treatments in these patients in situations where there is risk of loss to follow-up [15].
Regression analyses found several characteristics associated with worsening visual acuity or worsening CFT at follow-up when these two outcomes were assessed individually. Worse baseline VA was associated with worse follow-up VA. In the case of CFT, presence of epiretinal membrane and longer interval between visits were associated with higher CFT at follow-up. Furthermore, CFT increased at a faster rate as follow-up intervals increased. In other words, this indicates that longer periods of time without treatment of DME could contribute to a more rapid accumulation of macular edema. However, when logistic regression was performed to identify factors associated with overall poor visual outcome, none of the prior mentioned variables were significant.
Patients with a delayed appointment had 4 times the odds of poor outcome (defined as either worse vision or worse CFT compared to baseline) when compared to those who were seen on schedule. This is interesting considering that those seen on schedule had higher disease severity as reflected by the higher proportion with PDR (63% of those seen on schedule vs 35% of those with delayed appointments).
Patients at our retina clinic were rescheduled based on physician judgment at the beginning of the COVID-19 pandemic. Algorithms for patient rescheduling during the pandemic have since then been published [10]. Reviewing the differences between patients who were rescheduled and those who were not, we found that patients who were rescheduled were less likely to have PDR (35% vs 63%) and hypertensive retinopathy (3% vs 16%). In the patient populations of other studies on COVID-19 related delays in anti-VEGF injections, patients who were rescheduled were more likely to have poor baseline VA [11], be female [11], or have mild/moderate NPDR [10] compared to patients seen on schedule. One survey found that patients who self-reported their overall health as poor, self-reported their race as white, or were of older age were more likely to be lost to follow-up for anti-VEGF injections during the pandemic [16]. However, despite this information from our study, other studies, and guidelines published, it is difficult to accurately predict which patients are at the highest risk of vision loss. Physicians need more objective data to accurately triage which patients need in-office evaluation and treatment and which patients can defer their visits. The experience during the pandemic with the need to limit crowding in clinics has made it increasingly important to develop home monitoring devices that can provide physicians with this information when triaging patients for follow-up.
Smartphone applications are available for diabetic retinopathy screening and monitoring without the need for patients to go to a retina clinic [17, 18]. These applications can check visual acuity and take fundus photos using just a smartphone, although more rigorous evaluation in prospective studies is needed. Limited data have been published regarding the use of teleophthalmology resources and their impact on clinical care decisions and outcomes during the COVID-19 pandemic [18, 19]. The array of resources available for home monitoring of retinal disease is expanding. The ForeseeHome AMD monitoring device is FDA approved and allows patients with intermediate AMD to monitor vision changes [20]. Home-based OCT imaging devices are in clinical trials for the monitoring of retinal thickness in patients with age-related macular degeneration [21, 22], and this technology is currently being developed for the monitoring of diabetic retinopathy as well [23]. The emergence of these technologies will increase the feasibility of remote monitoring of chronic retinal diseases while reducing patient obligations to travel to healthcare facilities.
A limitation of our study is that we only assessed patients at two timepoints in their clinical care: at a baseline “pre-pandemic” point and at a follow-up point during the pandemic. We did not perform long term follow-up of the visual outcomes of patients with delays in treatments to see if their vision would recover to baseline level after re-initiating treatments. Further studies on long term outcomes of patients with DME and delay of care could provide more information on how to make clinical triaging decisions during situations like the COVID-19 pandemic.
Conclusion
The COVID-19 pandemic was associated with an inevitable delay in follow-up care and treatment for many patients with DME. Most patients seen at our clinic had their appointments delayed by several months, and this was associated with a worsening of macular or edema at follow-up compared to patients who were seen on schedule. Potential factors associated with worse outcomes are poor eye health at baseline and longer intervals between anti-VEGF injections, but it is difficult to accurately predict which patients are at highest risk for disease progression without regular checkup. These findings demonstrate the value of implementing home monitoring devices to evaluate diabetic retinopathy progression with objective data when capacity for in person visits becomes limited.
References
Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376(9735):124–36. https://doi.org/10.1016/S0140-6736(09)62124-3.
Yau JWY, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–64. https://doi.org/10.2337/dc11-1909.
Ciulla TA, Amador AG, Zinman B. Diabetic retinopathy and diabetic macular edema: pathophysiology, screening, and novel therapies. Diabetes Care. 2003;26(9):2653–64. https://doi.org/10.2337/diacare.26.9.2653.
Stewart MW. Anti-vegf therapy for diabetic macular edema. Curr Diab Rep. 2014;14(8):510. https://doi.org/10.1007/s11892-014-0510-4.
Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. What impact has covid-19 had on outpatient visits? Published online 2020. https://doi.org/10.26099/DS9E-JM36.
Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the covid-19 pandemic on hospital admissions in the united states. Health Aff. 2020;39(11):2010–7. https://doi.org/10.1377/hlthaff.2020.00980.
Xu D, Starr MR, Boucher N, et al. Real-world vitreoretinal practice patterns during the 2020 COVID-19 pandemic: a nationwide, aggregated health record analysis. Curr Opin Ophthalmol. 2020;31(5):427–34. https://doi.org/10.1097/ICU.0000000000000692.
Prünte C, Fajnkuchen F, Mahmood S, et al. Ranibizumab 0.5 mg treat-and-extend regimen for diabetic macular oedema: the RETAIN study. Br J Ophthalmol. 2016;100(6):787–95. https://doi.org/10.1136/bjophthalmol-2015-307249.
Stone LG, Devenport A, Stratton IM, Talks JS. Macula service evaluation and assessing priorities for anti-VEGF treatment in the light of COVID-19. Graefes Arch Clin Exp Ophthalmol. Published online July 25, 2020:1–7. https://doi.org/10.1007/s00417-020-04849-8.
Corazza P, D’Alterio FM, Younis S. Proposed algorithm during COVID-19 pandemic for patient management in medical retina clinic. Int J Retina Vitreous. 2020;6(1):20. https://doi.org/10.1186/s40942-020-00226-z.
Naravane AV, Mundae R, Zhou Y, et al. Short term visual and structural outcomes of anti-vascular endothelial growth factor (Anti-vegf) treatment delay during the first COVID-19 wave: A pilot study. PLoS One. 2021;16(2): e0247161. https://doi.org/10.1371/journal.pone.0247161.
Sindal MD, Chhabra K, Khanna V. Profile of patients receiving intravitreal anti-vascular endothelial growth factor injections during COVID-19-related lockdown. Indian J Ophthalmol. 2021;69(3):730–3. https://doi.org/10.4103/ijo.IJO_2807_20.
Kondo K, Low A, Everson T, et al. Health disparities in veterans: a map of the evidence. Med Care. 2017;55(Suppl 9 Suppl 2):S9–15. https://doi.org/10.1097/MLR.0000000000000756.
Cucinotta D, Vanelli M. Who declares covid-19 a pandemic. Acta Biomed. 2020;91(1):157–60. https://doi.org/10.23750/abm.v91i1.9397.
Wubben TJ, Johnson MW, Anti-VEGF Treatment Interruption Study Group. Anti-vascular endothelial growth factor therapy for diabetic retinopathy: consequences of inadvertent treatment interruptions. Am J Ophthalmol. 2019;204:13–8. https://doi.org/10.1016/j.ajo.2019.03.005.
Lindeke-Myers A, Zhao PYC, Meyer BI, et al. Patient perceptions of sars-cov-2 exposure risk and association with continuity of ophthalmic care. JAMA Ophthalmol. 2021;139(5):508–15. https://doi.org/10.1001/jamaophthalmol.2021.0114.
Aruljyothi L, Janakiraman A, Malligarjun B, Babu BM. Smartphone applications in ophthalmology: a quantitative analysis. Indian J Ophthalmol. 2021;69(3):548–53. https://doi.org/10.4103/ijo.IJO_1480_20.
Galiero R, Pafundi PC, Nevola R, et al. The importance of telemedicine during covid-19 pandemic: a focus on diabetic retinopathy. J Diabetes Res. 2020;2020: e9036847. https://doi.org/10.1155/2020/9036847.
Raparia E, Husain D. Covid-19 launches retinal telemedicine into the next frontier. Semin Ophthalmol. 2021;36(4):258–63. https://doi.org/10.1080/08820538.2021.1893352.
Chew EY, Clemons TE, Bressler SB, AREDS2-HOME Study Research Group, et al. Randomized trial of a home monitoring system for early detection of choroidal neovascularization home monitoring of the Eye (HOME) study. Ophthalmology. 2014;121(2):535–44.
Vision N. Notal vision launches first U. S. Home oct longitudinal study with patient self-operated device. GlobeNewswire News Room. Published January 12, 2021. https://www.globenewswire.com/en/news-release/2021/01/12/2157032/0/en/Notal-Vision-Launches-First-U-S-Home-OCT-Longitudinal-Study-with-Patient-Self-operated-Device.html. Accessed 24 Dec 2021.
Notal Vision Ltd. Home Retinal Imaging Using Notal-Oct v3. 0. clinicaltrials.gov; 2021. https://clinicaltrials.gov/ct2/show/NCT04241198. Accessed 24 Dec 2021.
Compact imaging collaborates with global pharma to accelerate development of home monitor for age-related macular degeneration and diabetic retinopathy. Compact Imaging. Published October 25, 2018. https://compactimaging.com/compact-imaging-collaborates-with-global-pharma-to-accelerate-development-of-home-monitor-for-age-related-macular-degeneration-and-diabetic-retinopathy/. Accessed 24 Dec 2021.
Acknowledgements
This work was supported in part by an Unrestricted Grant from Research to Prevent Blindness, Inc. to the UW Madison Department of Ophthalmology and Visual Sciences. RC is supported by National Eye Institute, K23 Career Development Award.
Author information
Authors and Affiliations
Contributions
Philip Zhou: Conceptualization, methodology, investigation, data curation, writing- original draft, writing- review & editing. Jie Gao: Conceptualization, methodology, investigation, writing- review & editing. Kristen Staggers: Formal analysis, data curation, software, writing- review & editing. Xiaofan Huang: Formal analysis, data curation, software, writing- review & editing. Kristin Biggerstaff: Methodology, resources, writing- review & editing. Silvia Orengo-Nania: Methodology, resources, supervision, writing- review & editing. Roomasa Channa: Conceptualization, methodology, visualization, supervision, project administration, writing- original draft, writing- review & editing.
Corresponding author
Ethics declarations
Conflicting interests
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, P., Gao, J., Huang, X. et al. Impact of the COVID-19 pandemic on visual outcomes of diabetic macular edema patients at a tertiary care veterans affairs center. J Diabetes Metab Disord 21, 759–768 (2022). https://doi.org/10.1007/s40200-022-01049-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-01049-5