Abstract
Purpose
Interest in mobile health applications (apps) for diabetes self-care is growing. Mobile health is a promising new treatment modality for diabetes, though few smartphone apps have been designed based on a proper study and prioritization. The aim of this study was to determine a minimum set of features for diabetes mobile apps.
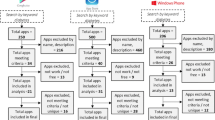
Methods
This study was conducted in three steps: 1.A review of the literature to collect all available features, 2. Assessing the validity of suggested features by Content Validity Index (CVI) and Content Validity Ratio (CVR), 3. Examining the importance of features by Friedman test.
Results
We retrieved all features of available mobile apps for type 2 diabetes, which are suggested and discussed in literature and compiled as a single list comprising of 33 features. Then, a survey of expert’s opinion produced a set of 23 final minimum features which includes all types of tracking, mealtime tagging, food database, diet management, educational materials, healthy coping, reducing risks, problem solving, Email, color coding, alerts, reminder, target range setting, trend chart view, logbook view, numerical indicators view, customizable theme, preset notes, and custom notes. According to the mean rank which indicates the priority of each feature, the most important one was blood glucose tracking (with 16.71 mean rank) and the least important feature was the numerical indicators like such as standard deviation or average (with 6.50 mean rank).
Conclusions
The present study is the first step towards the development of our mobile apps for people with type II diabetes, and highest the essential features that are required for an optimal self-care comprehensively.

Similar content being viewed by others
References
Breland JY, Yeh VM, Yu J. Adherence to evidence-based guidelines among diabetes self-management apps. Transl Behav Med. 2013;3(3):277–86.
World Health Organisation. Global report on diabetes. https://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf?sequence=1. Accessed 19 March 2019.
Torjesen I. More than half of diabetes patients are not getting standard health checks. British Medical Journal Publishing Group. 2012.
Fatehi F, Menon A, Bird D. Diabetes care in the digital era: a synoptic overview. Curr Diab Rep. 2018;18(7):38.
Group UPDS. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837–53.
World Health Organisation. The global diffusion of eHealth: making universal health coverage achievable: report of the third global survey on eHealth. Geneva: WHO; 2016.
Holtz B, Lauckner C. Diabetes management via mobile phones: a systematic review. Telemed J E Health. 2012;18(3):175–84.
Eng DS, Lee JM. The promise and peril of mobile health appss for diabetes and endocrinology. Pediatr Diabetes. 2013;14(4):231–8.
Fu H, McMahon SK, Gross CR, et al. Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: a systematic review. Diabetes Res Clin Pract. 2017;131:70–81.
Eng DS, Lee JM. The promise and peril of mobile health applications for diabetes and endocrinology. Pediatr Diabetes. 2013;14(4):231–8.
Ristau RA, Yang J, White JR. Evaluation and evolution of diabetes mobile appss: key factors for healthcare professionals seeking to guide patients. Diabetes Spectr. 2013;26(4):211–5.
Goyal S, Lewis G, Yu C, Rotondi M, Seto E, Cafazzo JA. Evaluation of a behavioral mobile phone app intervention for the self-management of type 2 diabetes: randomized controlled trial protocol. JMIR Res Protoc. 2016;5(3):e174.
Garabedian LF, Ross-Degnan D, Wharam JF. Mobile phone and smartphone technologies for diabetes care and self-management. Curr Diab Rep. 2015;15(12):109.
Basilico A, Marceglia S, Bonacina S, Pinciroli F. Advising patients on selecting trustful apps for diabetes self-care. Comput Biol Med. 2016;71:86–96.
Strickland PAO, Hudson SV, Piasecki A, Hahn K, Cohen D, Orzano AJ, et al. Features of the Chronic Care Model (CCM) associated with behavioral counseling and diabetes care in community primary care. J Am Board Fam Med. 2010;23(3):295–305.
Sibal L, Home PD. Management of type 2 diabetes: NICE guidelines. Clin Med. 2009;9(4):353–7.
Paulweber B, Valensi P, Lindström J, Lalic N, Greaves C, McKee M, et al. A European evidence-based guideline for the prevention of type 2 diabetes. Horm Metab Res. 2010;42(S 01):S3–S36.
Chomutare T, Fernandez-Luque L, Årsand E, Hartvigsen G. Features of mobile diabetes appss: review of the literature and analysis of current appss compared against evidence-based guidelines. J Med Internet Res. 2011;13(3):e65.
Gao J, Wang J, Zhu Y, Yu J. Validation of an information–motivation–behavioral skills model of self-care among Chinese adults with type 2 diabetes. BMC Public Health. 2013;13(1):100.
Williams JP, Schroeder D. Popular glucose tracking apps and use of mHealth by Latinos with diabetes. JMIR Mhealth Uhealth. 2015;3(3):e84.
Rao A, Hou P, Golnik T, Flaherty J, Vu S. Evolution of data management tools for managing self-monitoring of blood glucose results: a survey of iPhone appss. J Diabetes Sci Technol. 2010;4(4):949–57.
Klonoff DC. The current status of mHealth for diabetes: will it be the next big thing? J Diabetes Sci Technol. 2013;7(3):749–58.
Demidowich AP, Lu K, Tamler R, Bloomgarden Z. An evaluation of diabetes self-management appss for android smartphones. J Telemed Telecare. 2012;18(4):235–8.
Chen L, Chuang L-M, Chang C-H, Wang C-S, Wang I-C, Chung Y, et al. Evaluating self-management behaviors of diabetic patients in a telehealthcare program: longitudinal study over 18 months. J Med Internet Res. 2013;15(12):e266.
Arnhold M, Quade M, Kirch W. Mobile appss for diabetics: a systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. J Med Internet Res. 2014;16(4).
Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–75.
Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;3596:382–6.
Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011;1(1):53–71.
Peeples M, Tomky D, Mulcahy K, Peyrot M, Siminerio L, Project AO, et al. Evolution of the American Association of Diabetes Educators' diabetes education outcomes project. The Diabetes Educator. 2007;33(5):794–817.
Wilkinson A, Whitehead L, Ritchie L. Factors influencing the ability to self-manage diabetes for adults living with type 1 or 2 diabetes. Int J Nurs Stud. 2014;51(1):111–22.
Sigurðardóttir ÁK. Self-care in diabetes: model of factors affecting self-care. J Clin Nurs. 2005;14(3):301–14.
Issom D-Z, Woldaregay AZ, Chomutare T, Bradway M, Årsand E, Hartvigsen G. Mobile apps for people with diabetes published between 2010 and 2015. Diabetes Management (DMJ). 2015;5(6):539–50.
Shi C. Mobile phone messaging for facilitating self-management of long-term illnesses: summaries of nursing care-related systematic reviews from the Cochrane library. International Journal of Evidence-Based Healthcare. 2013;11(4):344–5.
Fijacko N, Brzan PP, Stiglic G. Mobile applications for type 2 diabetes risk estimation: a systematic review. J Med Syst. 2015;39(10):124.
Okazaki S, Castañeda JA, Sanz S, Henseler J. Factors affecting mobile diabetes monitoring adoption among physicians: questionnaire study and path model. J Med Internet Res. 2012;14(6):e183.
Eyler AA. Are diabetes self-management apps based on evidence? Transl Behav Med. 2013;3(3):233.
Beratarrechea A, Lee AG, Willner JM, Jahangir E, Ciapponi A, Rubinstein A. The impact of mobile health interventions on chronic disease outcomes in developing countries: a systematic review. Telemedicine and e-Health. 2014;20(1):75-82.
Acknowledgments
This study is a part of a Ph.D. dissertation financially supported by Tehran University of Medical Sciences (Grant: # 37529-97-01-31). We appreciate the contributions of all members of the Board of Health Informatics, Adult Endocrinologist, Health Education and Promotion which commented on our questionnaire form.
Author information
Authors and Affiliations
Contributions
Conception and design: Raheleh Salari, Sharareh R. Niakan Kalhori, Marjan Ghazisaeedi. Provision of study material or patients: Raheleh Salari, Sharareh R. Niakan Kalhori, Marjan Ghazisaeedi. Collection and assembly of data: Raheleh Salari, Sharareh R. Niakan Kalhori. Data analysis and interpretation: Raheleh Salari, Sharareh R. Niakan Kalhori. Manuscript writing: All authors. Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Limitation
The number of specialists filling out the questionnaire was less than expected. Due to the widespread geographical dispersion, there was no possibility to deliver this form in paper in person for all of them. Therefore the questionnaire form emeiled in electronic form. Inaccessibility to the full text of some articles were another limitation in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Salari, R., Niakan Kalhori, S.R., Fatehi, F. et al. Determining minimum set of features for diabetes mobile apps. J Diabetes Metab Disord 18, 333–340 (2019). https://doi.org/10.1007/s40200-019-00417-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-019-00417-y