Abstract
Purpose of Review
Von Hippel-Lindau disease is a multiple neoplasia syndrome that encompasses uncommon tumor types including hemangioblatoma, pheochromocytoma, renal cancer, and pancreatic neuroendocrine tumors. The disease is highly variable, and a review of the literature reinforces the need for referral for genetic risk assessment and counseling when a patient has any component tumor.
Recent Findings
Research from registry-based von Hippel-Lindau disease (VHL) populations provides new evidence of the benefits of patient compliance with close surveillance, the significantly younger age of renal cancer compared to the US population, evidence that pregnancy may not trigger new hemangioblastomas, and that the rate of new tumor growth is age and genotype dependent with the highest rates occurring between 30 and 34 years. Testing for somatic mosaicism has not moved from research to the clinical realm despite the known clinical implications for patients. Qualitative research supports observations that patients attribute stories of resilience to their medical experiences, while they also endorse that greater support is needed to help them cope with VHL-related distress.
Summary
The breadth of considerations in risk assessment, genetic testing, and psychosocial issues for VHL patient across the lifespan is described.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Maher ER, Yates JRW, Harries R, Benjamin C, Harris R, Moore AT, et al. Clinical features and natural history of von Hippel-Lindau disease. QJM. 1990;77(1):1151–63.
Lonser RR, Glenn GM, Walther M, Chew EY, Libutti SK, Linehan WM, et al. von Hippel-Lindau disease. Lancet. 2003;361(9374):2059–67.
Latif F, Tory K, Gnarra J, Yao M, Duh FM, Orcutt ML, et al. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science. 1993;260(5112):1317–20.
Herman JG, Latif F, Weng Y, Lerman MI, Zbar B, Liu S, et al. Silencing of the VHL tumor-suppressor gene by DNA methylation in renal carcinoma. Proc Natl Acad Sci U S A. 1994;91(21):9700–4.
Iliopoulos O, Levy AP, Jiang C, Kaelin Jr WG, Goldberg MA. Negative regulation of hypoxia-inducible genes by the von Hippel-Lindau protein. Proc Natl Acad Sci U S A. 1996;93(20):10595–9.
Schunemann V, Huntoon K, Lonser RR. Personalized medicine for nervous system manifestations of von Hippel-Lindau disease. Frontiers in surgery. 2016;3:39.
van der Mijn JC, Panka DJ, Geissler AK, Verheul HM, Mier JW. Novel drugs that target the metabolic reprogramming in renal cell cancer. Cancer Metab. 2016;4:14.
• Gossage L, Eisen T, Maher ER. VHL, the story of a tumour suppressor gene. Nat Rev Cancer. 2015;15(1):55–64. The authors provide an elegant historical perspective with emphasis on the importance of the VHL gene in the biological understanding of cancer.
Poulsen ML, Budtz-Jorgensen E, Bisgaard ML. Surveillance in von Hippel-Lindau disease (vHL). Clin Genet. 2010;77(1):49–59.
Binderup ML, Budtz-Jorgensen E, Bisgaard ML. Risk of new tumors in von Hippel-Lindau patients depends on age and genotype. Genetics in medicine : official journal of the American College of Medical Genetics. 2016;18(1):89–97.
Stolle C, Glenn G, Zbar B, Humphrey JS, Choyke P, Walther M, et al. Improved detection of germline mutations in the von Hippel-Lindau disease tumor suppressor gene. Hum Mutat. 1998;12(6):417–23.
GeneTests. GeneTests. [12/14/16]. 2016. Available from: genetests.org.
Freed D, Stevens EL, Pevsner J. Somatic mosaicism in the human genome. Genes (Basel). 2014;5(4):1064–94.
Murgia A, Martella M, Vinanzi C, Polli R, Perilongo G, Opocher G. Somatic mosaicism in von Hippel-Lindau disease. Hum Mutat. 2000;15(1):114.
Santarpia L, Sarlis NJ, Santarpia M, Sherman SI, Trimarchi F, Benvenga S. Mosaicism in von Hippel-Lindau disease: an event important to recognize. J Cell Mol Med. 2007;11(6):1408–15.
Sgambati MT, Stolle C, Choyke PL, Walther MM, Zbar B, Linehan WM, et al. Mosaicism in von Hippel-Lindau disease: lessons from kindreds with germline mutations identified in offspring with mosaic parents. Am J Hum Genet. 2000;66(1):84–91.
• Coppin L, Grutzmacher C, Crepin M, Destailleur E, Giraud S, Cardot-Bauters C, et al. VHL mosaicism can be detected by clinical next-generation sequencing and is not restricted to patients with a mild phenotype. European journal of human genetics : EJHG. 2014;22(9):1149–52.The authors are first to demonstrate technical feasibility of detecting VHL mosaicism with next-generation sequencing which holds promise for defining atypical cases in the future.
VHL Alliance. [VHL Alliance Homepage]. 2016. Available from: vhl.org.
Catapano D, Muscarella LA, Guarnieri V, Zelante L, D’Angelo VA, D’Agruma L. Hemangioblastomas of central nervous system: molecular genetic analysis and clinical management. Neurosurgery. 2005;56(6):1215–21. discussion 21
Hes FJ, McKee S, Taphoorn MJ, Rehal P, van Der Luijt RB, McMahon R, et al. Cryptic von Hippel-Lindau disease: germline mutations in patients with haemangioblastoma only. J Med Genet. 2000;37(12):939–43.
Woodward ER, Wall K, Forsyth J, Macdonald F, Maher ER. VHL mutation analysis in patients with isolated central nervous system haemangioblastoma. Brain J Neurol. 2007;130(Pt 3):836–42.
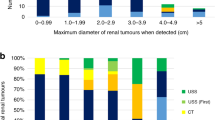
Neumann HP, Bender BU, Berger DP, Laubenberger J, Schultze-Seemann W, Wetterauer U, et al. Prevalence, morphology and biology of renal cell carcinoma in von Hippel-Lindau disease compared to sporadic renal cell carcinoma. J Urol. 1998;160(4):1248–54.
Bausch B, Wellner U, Peyre M, Boedeker CC, Hes FJ, Anglani M, et al. Characterization of endolymphatic sac tumors and von Hippel-Lindau disease in the International Endolymphatic Sac Tumor Registry. Head & neck. 2016;38(Suppl 1):E673–9.
Brauch H, Hoeppner W, Jahnig H, Wohl T, Engelhardt D, Spelsberg F, et al. Sporadic pheochromocytomas are rarely associated with germline mutations in the vhl tumor suppressor gene or the ret protooncogene. J Clin Endocrinol Metab. 1997;82(12):4101–4.
Erlic Z, Ploeckinger U, Cascon A, Hoffmann MM, von Duecker L, Winter A, et al. Systematic comparison of sporadic and syndromic pancreatic islet cell tumors. Endocr Relat Cancer. 2010;17(4):875–83.
Castellano M, Mori L, Giacche M, Agliozzo E, Tosini R, Panarotto A, et al. Genetic mutation screening in an Italian cohort of nonsyndromic pheochromocytoma/paraganglioma patients. Ann N Y Acad Sci. 2006;1073:156–65.
SEER Cancer Stat Fact Sheets [Internet]. [cited 12/14/16]. Available from: seer.cancer.gov.
• Shuch B, Vourganti S, Ricketts CJ, Middleton L, Peterson J, Merino MJ, et al. Defining early-onset kidney cancer: implications for germline and somatic mutation testing and clinical management. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32(5):431–7.The authors provide evidence that the average age of renal cancer diagnosis is significantly younger and provides grounds for using age in identifying which patients should be referred for genetic risk assessment and evaluation.
Brito JP, Asi N, Bancos I, Gionfriddo MR, Zeballos-Palacios CL, Leppin AL, et al. Testing for germline mutations in sporadic pheochromocytoma/paraganglioma: a systematic review. Clin Endocrinol. 2015;82(3):338–45.
• Binderup ML, Budtz-Jorgensen E, Bisgaard ML. New von Hippel-Lindau manifestations develop at the same or decreased rates in pregnancy. Neurology. 2015;85(17):1500–3. The evidence presented in this retrospective study that pregnancy does not necessarilty aggravate tumors can provide clinicians with some reassurance when counseling women with VHL who are planning pregnancy.
Lenders JW. Pheochromocytoma and pregnancy: a deceptive connection. Eur J Endocrinol. 2012;166(2):143–50.
Chittiboina P, Lonser RR. Von Hippel-Lindau disease. Handb Clin Neurol. 2015;132:139–56.
Metelo AM, Noonan HR, Li X, Jin Y, Baker R, Kamentsky L, et al. Pharmacological HIF2alpha inhibition improves VHL disease-associated phenotypes in zebrafish model. J Clin Invest. 2015;125(5):1987–97.
Noonan HR, Metelo AM, Kamei CN, Peterson RT, Drummond IA, Iliopoulos O. Loss of vhl in the zebrafish pronephros recapitulates early stages of human clear cell renal cell carcinoma. Dis Model Mech. 2016;9(8):873–84.
Kasparian NA, Rutstein A, Sansom-Daly UM, Mireskandari S, Tyler J, Duffy J, et al. Through the looking glass: an exploratory study of the lived experiences and unmet needs of families affected by Von Hippel-Lindau disease. European journal of human genetics : EJHG. 2015;23(1):34–40.
Lammens CR, Bleiker EM, Verhoef S, Hes FJ, Ausems MG, Majoor-Krakauer D, et al. Psychosocial impact of Von Hippel-Lindau disease: levels and sources of distress. Clin Genet. 2010;77(5):483–91.
Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. The American psychologist. 2000;55(5):469–80.
Schmidt L. Peering down the rabbit hole: living with von Hippel-Lindau syndrome from the young adult perspective [Masters thesis]. Brandeis Institutional Repository: Brandeis University; 2015.
Rechitsky S, Verlinsky O, Chistokhina A, Sharapova T, Ozen S, Masciangelo C, et al. Preimplantation genetic diagnosis for cancer predisposition. Reprod BioMed Online. 2002;5(2):148–55.
Lammens C, Bleiker E, Aaronson N, Vriends A, Ausems M, Jansweijer M, et al. Attitude towards pre-implantation genetic diagnosis for hereditary cancer. Familial Cancer. 2009;8(4):457–64.
Meister U, Finck C, Stobel-Richter Y, Schmutzer G, Brahler E. Knowledge and attitudes towards preimplantation genetic diagnosis in Germany. Hum Reprod. 2005;20(1):231–8.
Quinn GP, Pal T, Murphy D, Vadaparampil ST, Kumar A. High-risk consumers’ perceptions of preimplantation genetic diagnosis for hereditary cancers: a systematic review and meta-analysis. Genetics in medicine: official journal of the American College of Medical Genetics. 2012;14(2):191–200.
Walther MM, Lubensky IA, Venzon D, Zbar B, Linehan WM. Prevalence of microscopic lesions in grossly normal renal parenchyma from patients with von Hippel-Lindau disease, sporadic renal cell carcinoma and no renal disease: clinical implications. J Urol. 1995;154(6):2010–4. discussion 4-5
Lammens CR, Aaronson NK, Hes FJ, Links TP, Zonnenberg BA, Lenders JW, et al. Compliance with periodic surveillance for Von-Hippel-Lindau disease. Genetics in medicine: official journal of the American College of Medical Genetics. 2011;13(6):519–27.
Rasmussen A, Alonso E, Ochoa A, De Biase I, Familiar I, Yescas P, et al. Uptake of genetic testing and long-term tumor surveillance in von Hippel-Lindau disease. BMC medical genetics. 2010;11:4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that there is no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Genetic Counseling and Clinical Testing
Rights and permissions
About this article
Cite this article
Chan-Smutko, G. Genetic Counseling in Von Hippel-Lindau Disease: Navigating the Landscape of a Well-Established Syndrome. Curr Genet Med Rep 5, 66–74 (2017). https://doi.org/10.1007/s40142-017-0119-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40142-017-0119-4