Abstract
Purpose of Review
To examine the effects of combining non-invasive brain stimulation (NIBS) with neuromuscular electrical stimulation (NMES) on upper limb function in patients with a stroke.
Recent Findings
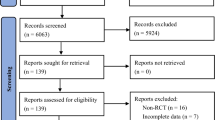
Of 580 articles, five studies met the eligibility criteria, involving 226 patients (mean age = 58.73 years), 45% of whom were female. Three studies considered "good" quality, one exhibited "excellent" quality, and one considered "poor" quality on the PEDro scale. There is heterogeneous evidence regarding the effects of the combined NIBS and NMES intervention on upper limb function in patients with a stroke.
Summary
The combination of NIBS with NMES might be a safe and well-tolerated intervention for patients with a stroke. However, the initial findings indicate that evidence regarding the effects of the combined NIBS and NMES intervention on upper limb function poststroke was limited. Further studies are strongly needed to understand the effects of the combined NIBS and NMES on upper limb outcomes and to identify the optimal treatment parameters.

Similar content being viewed by others
Data Availability
NA.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(7):2064–89. https://doi.org/10.1161/STR.0b013e318296aeca.
Simpson LA, Hayward KS, McPeake M, Field TS, Eng JJ. Challenges of Estimating Accurate Prevalence of Arm Weakness Early After Stroke. Neurorehabil Neural Repair. 2021;35(10):871–9. https://doi.org/10.1177/15459683211028240.
Grefkes C, Fink GR. Recovery from stroke: current concepts and future perspectives. Neurol Res Pract. 2020;2:17. https://doi.org/10.1186/s42466-020-00060-6.
Hatem SM, Saussez G, Della Faille M, et al. Rehabilitation of Motor Function after Stroke: A Multiple Systematic Review Focused on Techniques to Stimulate Upper Extremity Recovery. Front Hum Neurosci. 2016;10:442. Published 2016 Sep 13. https://doi.org/10.3389/fnhum.2016.00442
Nudo RJ, Plautz EJ, Frost SB. Role of adaptive plasticity in recovery of function after damage to motor cortex. Muscle Nerve. 2001;24(8):1000–19. https://doi.org/10.1002/mus.1104.
Simkins M, Kim H, Abrams G, Byl N, Rosen J. Robotic unilateral and bilateral upper-limb movement training for stroke survivors afflicted by chronic hemiparesis. IEEE Int Conf Rehabil Robot. 2013;2013:6650506. https://doi.org/10.1109/icorr.2013.6650506
Krause T, Asseyer S, Taskin B, et al. The Cortical Signature of Central Poststroke Pain: Gray Matter Decreases in Somatosensory, Insular, and Prefrontal Cortices. Cereb Cortex. 2016;26(1):80–8. https://doi.org/10.1093/cercor/bhu177.
Chen G, Huang C, Liu Y, et al. Efficacy and safety of grain moxibustion in hemiplegia: A systematic review and meta-analysis protocol. Medicine (Baltimore). 2019;98(17):e15215. https://doi.org/10.1097/MD.0000000000015215.
Hummel F, Cohen LG. Improvement of motor function with noninvasive cortical stimulation in a patient with chronic stroke. Neurorehabil Neural Repair. 2005;19(1):14–9. https://doi.org/10.1177/1545968304272698.
Chipchase LS, Schabrun SM, Hodges PW. Peripheral electrical stimulation to induce cortical plasticity: a systematic review of stimulus parameters. Clin Neurophysiol. 2011;122(3):456–63. https://doi.org/10.1016/j.clinph.2010.07.025.
de Kroon JR, Ijzerman MJ, Lankhorst GJ, Zilvold G. Electrical stimulation of the upper limb in stroke: stimulation of the extensors of the hand vs. alternate stimulation of flexors and extensors. Am J Phys Med Rehabil. 2004;83(8):592–600. https://doi.org/10.1097/01.phm.0000133435.61610.55.
Kristensen MGH, Busk H, Wienecke T. Neuromuscular electrical stimulation improves activities of daily living post stroke: a systematic review and meta-analysis. Arch Rehabil Res Clin Transl. 2021;4(1):100167. https://doi.org/10.1016/j.arrct.2021.100167
Ward NS. Mechanisms underlying recovery of motor function after stroke. Postgrad Med J. 2005;81(958):510–4. https://doi.org/10.1136/pgmj.2004.030809.
Simonetti D, Zollo L, Milighetti S, et al. Literature review on the effects of tDCS Coupled with robotic therapy in post stroke upper limb rehabilitation. Front Hum Neurosci. 2017;11:268. https://doi.org/10.3389/fnhum.2017.00268.
•• Alashram AR, Padua E, Romagnoli C, Raju M, Annino G. Effects of Repetitive transcranial magnetic stimulation on upper extremity spasticity Post-Stroke: A Systematic review. Physikalische Medizin Rehabilitationsmedizin Kurortmedizin. 2021. https://doi.org/10.1055/a-1691-9641. This study reported that combining rTMS with other rehabilitation interventions may show a superior effect in reducing the upper extremity spasticity compared with rTMS intervention alone.
Alashram AR, Padua E, Aburub A, Raju M, Annino G. Transcranial direct current stimulation for upper extremity spasticity rehabilitation in stroke survivors: A systematic review of randomized controlled trials. PM R. 2023;15(2):222–34. https://doi.org/10.1002/pmrj.12804.
Tedla JS, Sangadala DR, Reddy RS, Gular K, Kakaraparthi VN, Asiri F. Transcranial direct current stimulation (tDCS) effects on upper limb motor function in stroke: an overview review of the systematic reviews. Brain Inj. 2023;37(2):122–33. https://doi.org/10.1080/02699052.2022.2163289.
Chen G, Lin T, Wu M, et al. Effects of repetitive transcranial magnetic stimulation on upper-limb and finger function in stroke patients: A systematic review and meta-analysis of randomized controlled trials. Front Neurol. 2022;13:940467. https://doi.org/10.3389/fneur.2022.940467.
Lee JH, Jeun YJ, Park HY, Jung YJ. Effect of transcranial direct current stimulation combined with rehabilitation on arm and hand function in stroke patients: a systematic review and meta-analysis. Healthcare (Basel). 2021;9(12):1705. https://doi.org/10.3390/healthcare9121705
Figlewski K, Blicher JU, Mortensen J, Severinsen KE, Nielsen JF, Andersen H. Transcranial Direct Current Stimulation Potentiates Improvements in Functional Ability in Patients With Chronic Stroke Receiving Constraint-Induced Movement Therapy. Stroke. 2017;48(1):229–32. https://doi.org/10.1161/STROKEAHA.116.014988.
Dehem S, Gilliaux M, Lejeune T, et al. Effectiveness of a single session of dual-transcranial direct current stimulation in combination with upper limb robotic-assisted rehabilitation in chronic stroke patients: a randomized, double-blind, cross-over study. Int J Rehabil Res. 2018;41(2):138–45. https://doi.org/10.1097/MRR.0000000000000274.
Gersner R, Kravetz E, Feil J, Pell G, Zangen A. Long-term effects of repetitive transcranial magnetic stimulation on markers for neuroplasticity: differential outcomes in anesthetized and awake animals. J Neurosci. 2011;31(20):7521–6. https://doi.org/10.1523/JNEUROSCI.6751-10.2011.
• Del Felice A, Daloli V, Masiero S, Manganotti P. Cathodal versus dual transcranial direct current stimulation for decreasing upper limb spasticity in chronic stroke individuals: a clinical and neurophysiological study [published correction appears in J Stroke Cerebrovasc Dis 2016;25(12):2932–41. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.08.008. This study demonstrated that cathodal tDCS is slightly more effective than dual tDCS in reducing distal upper limb spasticity in chronic poststroke subjects.
• Hainaut K, Duchateau J. Neuromuscular electrical stimulation and voluntary exercise. Sports Med. 1992;14(2):100–13. https://doi.org/10.2165/00007256-199214020-00003(Thisstudyshowedthat. NMES effectively retards muscle wasting during denervation or immobilization and optimizes recovery of muscle strength during rehabilitation.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100.
Macedo LG, Elkins MR, Maher CG, Moseley AM, Herbert RD, Sherrington C. There was evidence of convergent and construct validity of Physiotherapy Evidence Database quality scale for physiotherapy trials. J Clin Epidemiol. 2010;63(8):920–5. https://doi.org/10.1016/j.jclinepi.2009.10.005.
Foley NC, Teasell RW, Bhogal SK, Speechley MR. Stroke Rehabilitation Evidence-Based Review: methodology. Top Stroke Rehabil. 2003;10(1):1–7.
Du J, Wang S, Cheng Y, et al. Effects of neuromuscular electrical stimulation combined with repetitive transcranial magnetic stimulation on upper limb motor function rehabilitation in stroke patients with hemiplegia. Comput Math Methods Med. 2022;2022:9455428. https://doi.org/10.1155/2022/9455428
Etoh S, Kawamura K, Tomonaga K, et al. Effects of concomitant neuromuscular electrical stimulation during repetitive transcranial magnetic stimulation before repetitive facilitation exercise on the hemiparetic hand. NeuroRehabilitation. 2019;45(3):323–9. https://doi.org/10.3233/NRE-192800.
Wei YY, Koh CL, Hsu MJ, Lo SK, Chen CH, Lin JH. Effects of Transcranial Direct Current Stimulation Combined With Neuromuscular Electrical Stimulation on Upper Extremity Motor Function in Patients With Stroke. Am J Phys Med Rehabil. 2022;101(2):145–51. https://doi.org/10.1097/PHM.0000000000001759.
Tosun A, Türe S, Askin A, et al. Effects of low-frequency repetitive transcranial magnetic stimulation and neuromuscular electrical stimulation on upper extremity motor recovery in the early period after stroke: a preliminary study. Top Stroke Rehabil. 2017;24(5):361–7. https://doi.org/10.1080/10749357.2017.1305644.
Koyama S, Tanabe S, Warashina H, et al. NMES with rTMS for moderate to severe dysfunction after stroke. NeuroRehabilitation. 2014;35(3):363–8. https://doi.org/10.3233/NRE-141127.
Di Pino G, Pellegrino G, Assenza G, et al. Modulation of brain plasticity in stroke: a novel model for neurorehabilitation. Nat Rev Neurol. 2014;10(10):597–608. https://doi.org/10.1038/nrneurol.2014.162.
Boros K, Poreisz C, Münchau A, Paulus W, Nitsche MA. Premotor transcranial direct current stimulation (tDCS) affects primary motor excitability in humans. Eur J Neurosci. 2008;27(5):1292–300. https://doi.org/10.1111/j.1460-9568.2008.06090.x.
Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527(Pt 3):633–9. https://doi.org/10.1111/j.1469-7793.2000.t01-1-00633.x.
Gartside IB. Mechanisms of sustained increases of firing rate of neurons in the rat cerebral cortex after polarization: reverberating circuits or modification of synaptic conductance? Nature. 1968;220(5165):382–3. https://doi.org/10.1038/220382a0.
Rossi S, Hallett M, Rossini PM, Pascual-Leone A. Safety of TMS Consensus Group. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120(12):2008–39. https://doi.org/10.1016/j.clinph.2009.08.016.
Sanchis-Gomar F, Lopez-Lopez S, Romero-Morales C, Maffulli N, Lippi G, Pareja-Galeano H. Neuromuscular electrical stimulation: a new therapeutic option for chronic diseases based on contraction-induced myokine secretion. Front Physiol. 2019;10:1463. https://doi.org/10.3389/fphys.2019.01463
Knutson JS, Fu MJ, Sheffler LR, Chae J. Neuromuscular Electrical Stimulation for Motor Restoration in Hemiplegia. Phys Med Rehabil Clin N Am. 2015;26(4):729–45. https://doi.org/10.1016/j.pmr.2015.06.002.
Harris JE, Eng JJ. Strength training improves upper-limb function in individuals with stroke: a meta-analysis. Stroke. 2010;41(1):136–40. https://doi.org/10.1161/STROKEAHA.109.567438.
Chae J. Neuromuscular electrical stimulation for motor relearning in hemiparesis. Phys Med Rehabil Clin N Am. 2003;14(1 Suppl):S93–109. https://doi.org/10.1016/s1047-9651(02)00051-7.
Greve KR, Joseph CF, Berry BE, Schadl K, Rose J. Neuromuscular electrical stimulation to augment lower limb exercise and mobility in individuals with spastic cerebral palsy: a scoping review. Front Physiol. 2022;13:951899. https://doi.org/10.3389/fphys.2022.951899
Guo Y, Phillips EB, Atherton PJ, Piasecki M. Molecular and neural adaptations to neuromuscular electrical stimulation; Implications for ageing muscle. Mech Ageing Dev. 2021;193:111402. https://doi.org/10.1016/j.mad.2020.111402.
Koseki T, Kudo D, Yoshida K, et al. Combined neuromuscular electrical stimulation and transcutaneous spinal direct current stimulation increases motor cortical plasticity in healthy humans. Front Neurosci. 2023;16:1034451. https://doi.org/10.3389/fnins.2022.1034451.
Mollayeva T, Mollayeva S, Colantonio A. Traumatic brain injury: sex, gender and intersecting vulnerabilities. Nat Rev Neurol. 2018;14(12):711–22. https://doi.org/10.1038/s41582-018-0091-y.
Ng YS, Tan KH, Chen C, Senolos GC, Koh GC. How Do Recurrent and First-Ever Strokes Differ in Rehabilitation Outcomes? Am J Phys Med Rehabil. 2016;95(10):709–17. https://doi.org/10.1097/PHM.0000000000000502.
Perna R, Temple J. Rehabilitation Outcomes: Ischemic versus Hemorrhagic Strokes. Behav Neurol. 2015;2015:891651. https://doi.org/10.1155/2015/891651.
Oosterveer DM, Wermer MJH, Volker G, Vlieland TPMV. Are there differences in long-term functioning and recovery between hemorrhagic and ischemic stroke patients receiving rehabilitation? J Stroke Cerebrovasc Dis. 2022;31(3):106294. https://doi.org/10.1016/j.jstrokecerebrovasdis.2021.106294.
Salvadori E, Papi G, Insalata G, et al. Comparison between ischemic and hemorrhagic strokes in functional outcome at discharge from an intensive rehabilitation hospital. Diagnostics (Basel). 2020;11(1):38. https://doi.org/10.3390/diagnostics11010038
Naghdi S, Ansari NN, Mansouri K, Hasson S. A neurophysiological and clinical study of Brunnstrom recovery stages in the upper limb following stroke. Brain Inj. 2010;24(11):1372–8. https://doi.org/10.3109/02699052.2010.506860.
Longley V, Peters S, Swarbrick C, Bowen A. What factors affect clinical decision-making about access to stroke rehabilitation? A systematic review Clin Rehabil. 2019;33(2):304–16. https://doi.org/10.1177/0269215518808000.
Hatem SM, Saussez G, Della Faille M, et al. Rehabilitation of Motor Function after Stroke: A Multiple Systematic Review Focused on Techniques to Stimulate Upper Extremity Recovery. Front Hum Neurosci. 2016;10:442. https://doi.org/10.3389/fnhum.2016.00442.
Cifu DX, Stewart DG. Factors affecting functional outcome after stroke: a critical review of rehabilitation interventions. Arch Phys Med Rehabil. 1999;80(5 Suppl 1):S35–9. https://doi.org/10.1016/s0003-9993(99)90101-6.
Simić-Panić D, Bošković K, Milićević M, et al. The Impact of Comorbidity on Rehabilitation Outcome after Ischemic Stroke. Acta Clin Croat. 2018;57(1):5–15. https://doi.org/10.20471/acc.2018.57.01.01.
Tan M, Li H, Wang X. Analysis of the current status of rehabilitation motivation and its influencing factors in older adults with stroke: a cross-sectional study. Front Aging Neurosci. 2023;15:1186681. https://doi.org/10.3389/fnagi.2023.1186681
Jung HY. Rehabilitation in subacute and chronic stage after stroke. In: Springer EBooks; 2017:351–360. https://doi.org/10.1007/978-981-10-1424-6_33
van Lieshout ECC, van der Worp HB, Visser-Meily JMA, Dijkhuizen RM. Timing of Repetitive Transcranial Magnetic Stimulation Onset for Upper Limb Function After Stroke: A Systematic Review and Meta-Analysis. Front Neurol. 2019;10:1269. https://doi.org/10.3389/fneur.2019.01269.
Lee JH, Jeun YJ, Park HY, Jung YJ. Effect of Transcranial Direct Current Stimulation Combined with Rehabilitation on Arm and Hand Function in Stroke Patients: A Systematic Review and Meta-Analysis. Healthcare (Basel). 2021;9(12):1705. https://doi.org/10.3390/healthcare9121705.
Obayashi S, Saito H. Neuromuscular Stimulation as an Intervention Tool for Recovery from Upper Limb Paresis after Stroke and the Neural Basis. Appl Sci. 2022;12(2):810. https://doi.org/10.3390/app12020810.
Raghavan P. Upper Limb Motor Impairment After Stroke. Phys Med Rehabil Clin N Am. 2015;26(4):599–610. https://doi.org/10.1016/j.pmr.2015.06.008.
Wu L, Subramanian N, Abdulrahman MD, Liu C, Pawar KS. Short-term versus long-term benefits: Balanced sustainability framework and research propositions. Sustain Prod Consum. 2017;11:18–30. https://doi.org/10.1016/j.spc.2016.09.003.
Hara Y. Brain plasticity and rehabilitation in stroke patients. J Nippon Med Sch. 2015;82(1):4–13. https://doi.org/10.1272/jnms.82.4.
Lieshout ECCV, van de Port IG, Dijkhuizen RM, Visser-Meily JMA. Does upper limb strength play a prominent role in health-related quality of life in stroke patients discharged from inpatient rehabilitation? Top Stroke Rehabil. 2020;27(7):525–33. https://doi.org/10.1080/10749357.2020.1738662.
Martin S, Cordeiro L, Richardson P, Davis S, Tartaglia N. The Association of Motor Skills and Adaptive Functioning in XXY/Klinefelter and XXYY Syndromes. Phys Occup Ther Pediatr. 2019;39(4):446–59. https://doi.org/10.1080/01942638.2018.1541040.
Jenkinson C, Fitzpatrick R, Crocker H, Peters M. The Stroke Impact Scale: validation in a UK setting and development of a SIS short form and SIS index. Stroke. 2013;44(9):2532–5. https://doi.org/10.1161/STROKEAHA.113.001847.
Sears ED, Chung KC. Validity and responsiveness of the Jebsen-Taylor Hand Function Test. J Hand Surg Am. 2010;35(1):30–7. https://doi.org/10.1016/j.jhsa.2009.09.008.
Feys P, Lamers I, Francis G, et al. The Nine-Hole Peg Test as a manual dexterity performance measure for multiple sclerosis. Mult Scler. 2017;23(5):711–20. https://doi.org/10.1177/1352458517690824.
Johnson D, Harris JE, Stratford P, Richardson J. Interrater Reliability of Three Versions of the Chedoke Arm and Hand Activity Inventory. Physiother Can. 2018;70(2):133–40. https://doi.org/10.3138/ptc.2016-70.
Uswatte G, Taub E, Morris D, Vignolo M, McCulloch K. Reliability and validity of the upper-extremity Motor Activity Log-14 for measuring real-world arm use. Stroke. 2005;36(11):2493–6. https://doi.org/10.1161/01.STR.0000185928.90848.2e.
Egger M, Smith GD. meta-analysis bias in location and selection of studies. BMJ. 1998;316(7124):61–6. https://doi.org/10.1136/bmj.316.7124.61.
Acknowledgements
I would like to thank Dr. Qusai Janada and Dr. Tareq Youssef, assistant professors in the physiotherapy department at Middle East University, for their general supervision in search strategy, data extraction, and methodological quality assessment.
Funding
This research did not receive any specific funding from public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
A.A: writing original draft, Search strategy, Quality assessment, Data extraction The author reviewed the manuscript
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Disclosure of interest
The author has nothing to disclose.
Permission
Permissions were approved by Dr. Qusai Janada and Dr. Tareq Youssef to include their names in acknowledgments.
Human and Animal Rights
Not applicable.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix A: Search strategy in MEDLINE
Appendix A: Search strategy in MEDLINE
(1) Stroke [MeSH].
(2) Cerebrovascular accident.
(3) CVA
(4) 1 OR 2 OR 3
(5) Noninvasive brain stimulation.
(6) transcranial direct current stimulation [MeSH].
(7) repetitive transcranial magnetic stimulation.
(8) Brain stimulation.
(9) rTMS.
(10) tDCs.
(11) Electric stimulation [MeSH].
(12) Electric stimulation therapy [MeSH].
(13) Neuromuscular electrical stimulation.
(14) NMES
(15) 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14
(16) Upper extremity [MeSH].
(17) Function.
(18) Disability.
(19) Muscle strength [MeSH].
(20) Motor.
(21) Physical.
(22) Independence.
(23) Range of motion.
(24) Muscle spasticity [MeSH].
(25) 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27
(33) 4 AND 15 AND 25
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alashram, A.R. Non-Invasive Brain Stimulation Combined with Neuromuscular Electrical Stimulation for Upper Limb Rehabilitation in Stroke Survivors: A Systematic Review. Curr Phys Med Rehabil Rep 12, 100–118 (2024). https://doi.org/10.1007/s40141-023-00428-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-023-00428-0