Abstract
Introduction
Oral administration of zeaxanthin (Zx) 20 mg daily in patients with unilateral neovascular age-related macular degeneration (nAMD) treated with triple therapy (photodynamic therapy/intravitreal bevacizumab/intravitreal dexamethasone) reduced fellow-eye 2-year nAMD incidence from 23 to 6% (p = 0.02) in a prior clinical trial. We questioned the long-term benefit and thus analyzed case–control 5-year patient data of trial participants and additional participants with 5-year follow-up, also performing cost-utility and cost–benefit analyses.
Methods
Consecutive, unilateral nAMD patient outcomes for those taking 20 mg Zx supplementation orally for ≥ 5 years were compared with the Comparison of AMD Treatments Trials (CATT) 5-year historical controls for fellow-eye nAMD conversion. Eleven-year mean life expectancy, cost-utility and cost–benefit models were undertaken employing a 3% discount rate and 2020 US real dollars.
Results
Among 227 consecutive patients with nAMD/Zx-supplementation, 202 (90%) had 5-year follow-up. The fellow-eye nAMD 5-year conversion incidence using a Kaplan–Meier cumulative event estimate was 22% (49/227), versus 48% (167/348) with CATT control data (p < 0.0001). An 11-year cost-utility model with estimates for years 6–11 demonstrated a 0.42 (7.7%) QALY (quality-adjusted life-year) gain, including 3 months of life saved per patient due to decreased nAMD fellow-eye conversion. This yielded a direct ophthalmic medical cost perspective, incremental cost-utility ratio (CUR) of −$576/QALY and a societal cost perspective CUR of −$125,071/QALY. Zx supplementation for all 2020 US unilateral nAMD cases would have theoretically saved society, primarily patients, $6.0 billion over 11 years, a 1531% return on investment (ROI), or 31.3% annual ROI, on Zx costs.
Conclusions
Oral zeaxanthin supplementation for unilateral nAMD patients appears to decrease fellow-eye long-term incidence and is cost-effective and financially rewarding. It is dominant vs. no supplementation in patients presenting with unilateral nAMD.
Trial Registration
ClinicalTrials.gov identifier, NCT01527435.
Similar content being viewed by others
A published 2-year randomized clinical trial previously revealed that oral zeaxanthin supplementation for patients with unilateral neovascular age-related macular degeneration (nAMD) reduced fellow-eye disease by 75%. Five-year case–control follow-up data herein revealed that zeaxanthin supplementation reduces atrophic fellow-eye conversion to nAMD from 48 to 22%, a 54% decrease. |
Zeaxanthin supplementation in patients with unilateral nAMD treated with triple therapy resulted in improved overall vision by preventing conversion of second eyes with atrophic macular degeneration to nAMD. Nonetheless, aside from the diminution of fellow eye conversion to nAMD in unilateral nAMD cases treated with zeaxanthin, there was no difference in vision between the groups with and without zeaxanthin supplementation. |
Cost–benefit analysis suggests that oral zeaxanthin supplementation in a 1-year cohort of all 114,000 unilateral US nAMD cases would net patients, insurers, and the American public a discounted US$ 6.0 billion above the cost of zeaxanthin over 11 years, a 1531% return on investment. |
Introduction
Age-related macular degeneration (AMD) is the leading cause of legal blindness in the United States, with neovascular age-related macular degeneration (nAMD) accounting for 90% of such cases [1]. Currently, intravitreal anti-VEGF (vascular endothelial growth factor-inhibitor) monotherapy is a mainstay of nAMD therapy [1, 2], though combination therapy [anti-VEGF monotherapy, corticosteroid, and photodynamic therapy (PDT)] can reduce patient treatment burden [1,2,3,4,5,6]. Combination therapy vision outcomes are typically similar to anti-VEGF monotherapy outcomes [2,3,4].
Antioxidants and other supplements have been recommended to prevent advanced dry AMD and nAMD [7,8,9,10,11,12,13,14], with retinal carotenoids zeaxanthin (Zx) and lutein utilized in combination. Zeaxanthin, the predominant carotenoid, is most concentrated in the macula [7,8,9,10]. It has been shown to prevent AMD in mice [7] and inhibit VEGF secretion by hypoxic retinal pigment epithelial cells in vitro [8]. Increased dietary carotenoids have been associated with decreased AMD [10] and nAMD [7] in humans, with the POLA (Pathologies Oculaires Liées à l’Age) Study Group [11] reporting that high plasma Zx and lutein levels were associated with a 93% decreased AMD risk versus low levels. Gale et al. [12] found that early and late AMD risk was higher with low plasma Zx levels.
In a non-randomized clinical trial of 424 nAMD participants, Olk et al. [5] noted that oral Zx supplementation to triple therapy reduced 2-year nAMD incidence in AMD fellow eyes from 12.5 to 6.25% (p = 0.03). In a subsequent 2-year, 144 nAMD-participant randomized clinical trial, Olk et al. [6] found that in patients with unilateral nAMD receiving no Zx supplementation, 23.0% of fellow eyes developed nAMD, while in participants receiving Zx supplementation, the conversion rate decreased by 75% to 5.8% (p = 0.02). Oral Zx supplementation with triple therapy was dominant vs. triple therapy alone, meaning it conferred a greater gain in quality-adjusted life-years (QALY) for less cost than triple therapy alone due to decreased fellow-eye nAMD conversion [6]. When decreased fellow eye conversions to nAMD in the zeaxanthin treated cohort were not considered, however, there was no difference in mean 2-year vision between the cohorts receiving Zx supplementation and receiving triple therapy alone (p = 0.50) [6].
Since prior studies have suggested that oral administration of Zx prevents nAMD [5,6,7, 9], we analyzed 5-year data of treatment with Zx supplementation to assess the unilateral nAMD conversion rate to bilateral nAMD and compare the conversion rate to historical controls not treated with Zx. Employing these data, we then considered an incremental cost-utility analysis (CUA) and cost–benefit analysis of Zx supplementation in cases with baseline unilateral nAMD.
The primary study outcome was fellow eye nAMD to assess if decreased nAMD conversion associated with oral supplementation of zeaxanthin at 2 years persisted with supplementation at 5 years. If it persisted, a cost-utility analysis would be undertaken to evaluate the cost-effectiveness of the supplementation. The secondary outcomes were (1) vision to assess if there was a 5-year vision difference between the cohorts with and without zeaxanthin supplementation who developed nAMD, and (2) a cost–benefit analysis to ascertain the cost of zeaxanthin supplementation versus the funds returned to society from the intervention.
Methods
Initial Analysis
An initial analysis was undertaken of 340 consecutive baseline participants from the practice of R. Joseph Olk, MD, in St. Louis, Missouri, enrolled between May 2012 and December 2015, with 5-year follow-up, who agreed to take supplemental Zx with triple therapy for presenting nAMD. Of the 340 patients, 227 (67%) had unilateral nAMD, while 113 had bilateral involvement. Three bilateral nAMD patients were excluded for non-compliance (taking less than 75% of Zx doses). Analyses were thus performed on 337 patients, with the primary cohort of interest consisting of the 227 participants who presented with baseline unilateral nAMD.
Demographics
Among the 337 participants enrolled at baseline, 205 (60.8%) were women and 132 (39.2%) were men. The median age was 80 years, and the mean age was 79.3 years (standard deviation [SD] = 8.8, 95% confidence interval [CI] = 78.3–80.1), ranging from 42–98 years.
In the 227-participant unilateral cohort, the baseline age was 79 years [SD = 8; 95% CI 78–80], with an 80-year median and range of 58–98 years. Women comprised 61% (138/227) and men 39% (89/227).
Inclusion Criteria
In our economic analyses we included consecutive participants with unilateral classic, minimally classic and/or occult nAMD who took 20 mg Zx orally each day in conjunction with triple therapy after careful explanation. Macular blood, subretinal fluid, subretinal pigment epithelial fluid, and/or hard exudate were typically present. Optical coherence tomography (OCT) confirmed the presence of subretinal fluid, subretinal pigment epithelial fluid and retinal edema. The presence of choroidal neovascularization was confirmed by intravenous fluorescein angiography and/or indocyanine green (ICG) angiography.
Exclusion Criteria
Eyes with fibrotic nAMD were excluded, as were those with choroidal neovascularization exceeding 12 disc areas. Blood was not an exclusion criterion unless it covered > 12 disc areas [4, 5]. Patients with no posterior segment drusen in either eye were excluded.
Triple Therapy/Zx Treatment Cohort
All eyes with nAMD were treated with the regimen shown in Tables S1 and S2. One treatment cycle consisted of (1) fundus photographs, fluorescein angiography/indocyanine green angiography, (2) a 1.25-mg intravitreal injection of bevacizumab at baseline, 1 month, 2 months and 3 months, (3) a 1.0 mg intravitreal dexamethasone injection at baseline, (4) 40 mg of sub-Tenon’s methylprednisolone acetate within 1 week, and (5) reduced-fluence photodynamic therapy (PDT) within 2 weeks utilizing verteporfin (6 mg/m2 × body surface area in meters squared) given intravenously over 10 minutes, followed by a 689-nm wavelength light dose of 25 J/cm2 for 83 seconds. Optical coherence tomography was performed at the beginning and end of each treatment cycle.
Patients were re-examined at 4–6 weeks after each treatment cycle, and Early Treatment of Diabetic Retinopathy Study (ETDRS) best-corrected visual acuity was measured at every visit. If considered stable, patients were followed every 2 months for 6 months, and then every 3 months thereafter. Another 3-month cycle of triple therapy was administered when retreatment was indicated. Retreatment was predicated on the occurrence of subretinal blood, subretinal/intraretinal fluid on OCT, decreased vision, fluorescein angiographic leakage, or an occult plaque seen with ICG angiography.
The incidence of participants requiring topical anti-hypertensive therapy for increased intraocular pressure secondary to corticosteroid therapy with triple therapy was approximately 2%. No participant required glaucoma surgery. Five percent of patients developed cataracts in eyes treated with triple therapy attributable to the corticosteroid therapy over the 5-year period.
Oral Supplementation
Among all 337 nAMD patients presenting, (85/337 =) 25.2% took an AREDS oral supplement (PreserVision; Bausch & Lomb, Laval, Quebec, Canada), while all patients took AREDS2 supplements containing 2 mg Zx and 10 mg lutein after May 2013, throughout 5 years and beyond. Each patient was also placed on 20 mg of orally administered zeaxanthin (EyePromise, Chesterfield, MO) daily from baseline through at least 5 years. Patients were questioned about Zx usage at each visit, and its importance was emphasized. Pill counts were undertaken at 3 months, 6 months, 12 months, and 24 months.
Among all 337 nAMD participants, the 25.8% (87/337) presenting prior to May 2013 took a daily AREDS oral supplement (PreserVision; Bausch & Lomb, Rochester, NY, USA) which did not contain zeaxanthin or lutein for an average of 2.5 months, while all patients took a daily AREDS2 supplement containing 2 mg Zx and 10 mg lutein (PreserVision AREDS2; Bausch & Lomb, Rochester, NY, USA) from May 2013 forward, through 5 years and beyond. Thus, among all 337 patients in the study, 25.2% took AREDS supplements for 4.2% (2.5 months/60 months) of their 5-year study time and AREDS2 supplements for 95.8% of their 5-year study time. The remaining 74.8% of participants recruited from May 2013 forward took AREDS2 supplements for 100% of their 5-year study time. Thus, overall, participants on average took AREDS supplements for 1.06% of the study time and AREDS2 supplements for 98.94%.
Cost-Utility Analysis for Participants Presenting with Unilateral nAMD
A CUA was performed utilizing a Value-Based Medicine® (standardized) model with patient utilities [1, 15,16,17] and recommendations of the Second Panel on Cost-effectiveness in Health and Medicine [18] in conjunction with CHEERS criteria. The model features are listed in Table 1 [16,17,18,19,20,21,22,23,24,25,26,27,28].
Overview
The model compared the 5-year nAMD conversion incidence in fellow eyes treated with oral Zx supplementation versus historical controls not using Zx in an extrapolated 11-year (mean life expectancy of a patient presenting with unilateral nAMD [1, 28]) incremental cost-utility analysis. The analyses used a $/QALY (dollars expended per quality-adjusted life-year gained) outcome, the cost-utility ratio (CUR). This analysis included 227 consecutive patients with unilateral nAMD and atrophic AMD in the fellow eye. Atrophic fellow-eye conversion data from the Comparison of AMD Treatments Trials (CATT) [29, 30], a randomized clinical trial comparing the 5-year effects of ranibizumab and bevacizumab for the treatment of nAMD were used as comparators for nAMD fellow-eye conversion rates. Macular Photocoagulation Study Group data were also compared [31].
Patient, time trade-off, vision utilities, the 2020 non-facility, national average Medicare Fee Schedule [27] (Table S4) both health (direct ophthalmic medical) and societal cost perspectives, and a commonly employed 3%/year discount rate for QALYs and costs were used [18].
Utilities
Time trade-off vision utilities were acquired by direct interview from over 1400 ophthalmic patients to quantify the quality of life associated with vision in the better-seeing eye [19,20,21,22,23,24,25,26]. The utilities have excellent validity [19] and reliability [20, 21] and are typically unaffected by age, gender, ethnicity, level of education, underlying ophthalmic disease, and systemic comorbidities [19,20,21,22,23,24,25,26].
Time Frame
The duration of Zx therapy was 5 years. Table S5 shows total follow-up of the cohort receiving Zx over 5 years. Of the 227-baseline unilateral nAMD participants, 5-year follow-up was available for (202/227 =) 88.9%, while among all 337 patients with baseline unilateral or bilateral nAMD, the 5-year follow-up was 90.5% (305/557).
An 11-year cost-utility model was selected since the life expectancy of the average 79-year-old unilateral nAMD patient at baseline was 11 years [1, 28]. The Second Panel on Cost-Effectiveness in Health and Medicine recommends the longest reasonable time frame for a cost-utility analysis to aid with decision making [18]. A last observation carried forward methodology was employed for nAMD fellow-eye conversions from years 6–11 using an average of year 1–5 conversion rates for our cohort treated with Zx and the CATT control cohort [29]. Triple therapy frequency from years 6–11 assumed patients were seen 3x/year [1, 5, 6]. Optical coherence tomography was obtained at each visit.
Vision outcomes for nAMD with different anti-VEGF monotherapies [1] and multi-therapies [1,2,3,4] have been shown to be similar [1,2,3,4]. In addition, because our prior 2-year randomized trial [6] demonstrated similar visual outcomes in nAMD eyes receiving triple therapy and triple therapy with Zx supplementation, we assumed that Zx supplementation had no acute intrinsic effect upon individually treated nAMD vision. Instead, supplementation with Zx reduced atrophic AMD fellow-eye conversion in eyes with mean 20/40 mean to nAMD, thereby improving the mean vision overall for the cohort receiving Zx supplementation.
Direct Ophthalmic Medical Costs
Unless otherwise specified, costs were in 2020 US real dollars. For the 227 unilateral nAMD cases, we also accrued the Zx cost to second-eye treatment costs needed over the 5-year period. In essence, the costs of triple therapy + Zx supplementation for second-eye conversion to nAMD were compared to the cost of triple therapy alone for second-eye conversion to nAMD in our control cohort not treated with Zx. Direct ophthalmic medical costs did not include medical costs associated with extra time of life gained from Zx supplementation, though the societal costs did.
Societal Costs
These included direct ophthalmic medical costs, direct non-ophthalmic medical costs [27, 32, 33], direct non-medical costs [34, 35] and indirect medical costs [35,36,37,38]. The societal costs saved by decreased second-eye nAMD conversion were measured by comparing the economic loss associated with the resultant mean second-eye vision in the cohorts receiving treatment with and without Zx supplementation annually over 11 years in unilateral nAMD cases [32,33,34,35,36,37,38].
Direct Non-Ophthalmic Medical Costs
These vision loss-related costs, including those for depression, injury, facilities, Medicare, and nursing homes [32], were converted to 2020 real dollars utilizing the Consumer Price Index (CPI) for medical care [33]. Direct non-medical costs, or caregiver costs, included those for inside and outside activities of daily living, residence change and transportation [34, 35], while indirect medical costs encompassed primarily wage loss due to decreased vision [35,36,37,38]. The latter two category costs were adjusted to 2020 real US dollars using the CPI [35]. In addition, the medical costs incurred due to years of life saved from Zx supplementation were incorporated [1].
The net societal costs saved over and above the direct ophthalmic medical costs and medical costs incurred by extending life were accrued as negative costs against the Zx costs to obtain the 11-year Zx return on investment (ROI).
Statistics
The cumulative incidence of 5-year fellow-eye conversion to nAMD was calculated employing Kaplan–Meier product-limit method estimates [39]. The chi-square test compared categorical variables such as proportions with fellow eye progression to nAMD. Linear variables, such as vision, were compared using the t-test (Microsoft, Bellevue, WA, USA). Significance was presumed to occur at p < 0.05.
Sample Size
By employing prior data [5, 6] and two-sided equality, sample size analysis to compare nAMD conversion proportions in the cohort receiving triple therapy with Zx supplementation and historical controls not receiving Zx revealed that 85 participants in each unilateral nAMD sample were required for 90% power to detect a significant difference at p < 0.05 [40]. The numbers utilized were based primarily upon a previous 2-year clinical trial [6] in which 3 of 47 (6%) patients with atrophic AMD fellow eyes undergoing 20 mg daily oral zeaxanthin supplementation converted to nAMD, versus 12 of 53 (23%) patients with atrophic AMD fellow eyes in a cohort not receiving supplementation (p = 0.03; Fisher exact test).
Institutional Review Board (IRB) Approval
All subjects gave written informed consent for inclusion before participation. The Wills Eye Hospital IRB approved utility acquisition, and the study adhered to the Declaration of Helsinki and its amendments. The SSM Health Care Institutional Review Board approved triple therapy with Zx supplementation (approval number 14-07-0540). The ClinicalTrials.gov identifier for the original randomized clinical trial is NCT 01527435 [6].
Results
Clinical Data
The mean baseline vision in nAMD eyes in the complete 337-person unilateral and bilateral nAMD was 20/125, while at 5 years it was 20/160. Baseline nAMD vision in the CATT cohort treated with VEGF monotherapy was 20/63+2 and 5-year mean vision was 20/63–1 [2]. Shah and DelPriore [41], utilizing untreated Macular Photocoagulation Study cohort data, performed a Lineweaver-Burk meta-analysis demonstrating that mean vision in the untreated nAMD cohort decreased with increasing duration of nAMD. In addition, Boyer et al. [42] demonstrated that nAMD patients treated sooner with VEGF inhibitors had better vision outcomes. Thus, we did not have a comparable historical 5-year control cohort to demonstrate a 5-year vision benefit in treated nAMD eyes between our participants with nAMD receiving Zx supplementation and the CATT nAMD participants who did not receive Zx supplementation. We therefore confined our major clinical and economic analyses to nAMD fellow-eye conversions in our nAMD participants who received Zx supplementation and the CATT nAMD participants [2, 29, 30] who did not receive Zx supplementation.
Vision
Mean baseline visual acuity in the atrophic AMD fellow eyes of the 227-participant cohort presenting with unilateral nAMD was 20/40 (Table 2). This mean vision remained 20/40 at 5 years in fellow eyes if no nAMD conversion occurred and was assumed to remain so through the 11-year model. The mean vision in the fellow eyes developing nAMD in the cohorts receiving and not receiving Zx supplementation decreased over 11 years as the 20/40 atrophic AMD fellow eyes in each sub-cohort converted to the same 20/125–20/160 vision level associated with nAMD triple therapy. Since the atrophic AMD fellow-eye conversion rate to nAMD was greater in eyes of patients not receiving Zx supplementation, the mean fellow-eye vision in that sub-cohort deteriorated more rapidly.
The median baseline age in the comparator CATT cohort was 78 years (79 years in our cohort) with an age range of 59 to 92 years (58–98 in our cohort). In the CATT cohort, 65% of participants were female, versus 61% in our cohort (Table 2). Among CATT enrollees, 98.5% were Caucasian, while 223/227 (98.2%) in our cohort were Caucasian. CATT participants were enrolled from 2008 through 2009; ours were enrolled from 2012 to 2015.
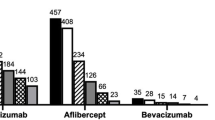
Conversion Rate of Fellow Eyes to nAMD
The 5-year conversion incidence in our cohort receiving Zx supplementation (n = 227) and that in patients in the CATT cohort who did not receive Zx (n = 348) [29, 30] are shown in a Kaplan–Meier cumulative event estimate [39] graph in Fig. 1. By 5 years, atrophic fellow eyes had converted to nAMD in 22% of our patients treated with Zx, whereas 48% of atrophic fellow eyes had converted in CATT [29] (p < 0.001), making our hazard ratio (22%/48% =) 0.46. The 5-year second-eye nAMD conversion rate in the patients not receiving Zx in the Macular Photocoagulation Study was 42%, and in the Three Continent Consortium Report it was 44% (Table 3) [2, 29, 30, 43,44,45,46,47,48]. The cumulative extrapolated conversion rate in our cohort treated with Zx was 41% at the end of 11 years, while in the CATT cohort it was 72% (Table 2). CATT 5-year data [29] were used in the cost-utility analysis comparing nAMD conversion rates since they were recent, included many patients taking AREDS2 supplements, and involved large numbers of participants. Annual conversion rates for our participants and CATT participants for years 6–11 were calculated using the average of the first 5-year annual percentage conversion rates for each cohort.
Kaplan–Meier cumulative event estimates of fellow eyes with incident nAMD in the cohort treated with zeaxanthin over a 5-year period (n = 227) and in the CATT (n = 348 at year 5). Events = fellow eyes converting to nAMD (neovascular age-related macular degeneration). Censored = number of patients who died or were lost to follow-up
Incremental Cost-Utility Analysis of 227 Baseline Patients with Unilateral nAMD Undergoing Triple Therapy with Zx Supplementation vs. Triple Therapy Alone
QALY Gain from Zx Supplementation
QALY gain was calculated in the 227-baseline unilateral nAMD cases by comparing the mean vision in fellow eyes of patients receiving Zx and those of patients not receiving Zx in CATT [29]. The major QALY gain occurred because the best-seeing eye utility remained at 0.8, correlating with 20/40 vision [16], in a greater proportion of eyes with Zx supplementation due to a lower incidence of conversion to nAMD in atrophic fellow eyes. The resultant 11-year QALY gain attributable to Zx supplementation, considering the adverse events of one case of endophthalmitis and irritation from the injections, was calculated to be 0.396, a 7.2% QALY gain over the 5.58 QALY accrual in the CATT cohort not treated with Zx. Nonetheless, as shown in Table S4, when the 0.25 year of life was gained as a result of better average vision from Zx supplementation because of decreased AMD conversion to nAMD (See Societal Costs below), another 0.027 QALY was gained for a total QALY gain of (0.396 + 0.027 =) 0.423 QALY. Thus, the quality-of-life component of QALY gain comprised (0.397/0.423 =) 93.7% of the total QALY gain and the length-of-life gain comprised (0.027/0.423 =) 6.3%. No serious adverse ocular or systemic events, including crystalline retinopathy, were noted due to Zx supplementation.
Costs
The 11-year, direct ophthalmic cost for triple therapy with Zx supplementation at baseline for an eye with nAMD in unilateral nAMD cases was $19,095 (Table 4). If a second eye presented with nAMD and the first eye was untreatable, or if both eyes were involved, the 11-year cost of treating the second eye was $15,664 (Table 4), the cost of treating the first eye minus the $3431 cost of Zx supplementation.
Unilateral Baseline nAMD Case, Mean Direct Ophthalmic Medical Costs for Treating Conversion of Atrophic AMD to nAMD in the Fellow Eye
Calculation of the cost differential between atrophic fellow eyes converting to nAMD with and without Zx-supplementation is shown in Table 5. The different triple therapy costs averaged $4765 in the Zx-supplemented cohort, although the 11-year, $3431 Zx cost, assuming all baseline unilateral nAMD participants were supplemented for 11 years, raised the mean ophthalmic treatment costs to $8196. For the non-Zx-treated cohort, the triple therapy costs were $8438, but no Zx costs were accrued. Thus, the mean 11-year, incremental, direct ophthalmic cost for treating second eyes converting to nAMD with triple therapy and Zx-supplementation in baseline unilateral nAMD patients was ($8196–$8438 =) −$242, less than without supplementation with Zx.
Societal Costs
Data from Christ et al. [49] referent to the Salisbury Eye Evaluation Study demonstrated that the incremental decreased vision in the cohort not treated with Zx was associated with a higher risk of premature death, specifically decreasing the life expectancy in this cohort from 11 years to 10.75 years for the average patient.
Premature mortality of a patient who did not receive Zx supplementation [49] also decreases the direct ophthalmic medical cost between years 10.76 and 11 for treating second eyes in the cohort not treated with Zx. This decreased cost totaled $23 and was considered in the direct ophthalmic medical cost perspective CUA (Table 5).
More relevant, the 0.25 years of life saved resulted in extra mean 2020 US real dollar healthcare cost (including nursing home cost) for a 90-year-old patient with baseline unilateral nAMD receiving Zx supplementation of $10,847 [50,51,52]. This direct non-ophthalmic medical cost was accrued in the cohort receiving Zx supplementation in the societal cost perspective analysis.
The mean 11-year societal costs saved per patient in the baseline unilateral nAMD, Zx-treated cohort by reducing the nAMD conversion incidence of second eyes totaled −$52,530 including the $10,847 11th-year direct non-ophthalmic medical cost addition during 0.25 years of saved life and the −$242 lower direct ophthalmic medical cost in the Zx cohort (Table 6). The costs were calculated by comparing fellow eye vision in patients receiving Zx supplementation and those not receiving Zx and correlating these with medical costs [27, 32], caregiver costs (transportation, inside and outside activities of daily living and residence change) [34] and wage differences associated with different vision levels [35,36,37]. No difference in wage costs was noted between our cohort and the CATT cohort at 11 years. There was, however, a caregiver cost gain of $63,135 saved by the average patient treated with Zx over 11 years.
Cost-Utility Ratios
The direct ophthalmic cost-utility ratio for Zx usage in patients with unilateral nAMD was (−$252/0.42 =) −$576/QALY and the societal cost-utility ratio was (−$52,530/0.42 =) −$125,071/QALY. The negative cost-utility ratios with each cost perspective indicate that Zx supplementation was dominant to no supplementation, since Zx supplementation conferred greater QALY (value) gain for less cost in each instance.
Incremental Cost-Utility Sensitivity Analysis on Zeaxanthin-Treated Baseline Unilateral nAMD Cases with Fellow-Eye Conversion
Conversion Rates of Fellow Eyes to nAMD
Considering the nAMD fellow-eye conversion ratio to be the least certain variable, we assessed alternatives shown in Table 7. Employing the direct ophthalmic medical cost perspective for a cost-utility upper limit of $100,000/QALY frequently used in the US [17], the average of nAMD relative, fellow-eye conversion rates over 11 years with Zx supplementation needed to be 2–3% less versus that of patients not treated with Zx. With the societal cost perspective, the $100,000/QALY ceiling was also reached at the 2–3% lower relative conversion rate of nAMD for fellow eyes receiving Zx supplementation. This occurred because caregiver societal costs and medical cost differences between the cohorts receiving and not receiving Zx did not differ appreciably when fellow-eye nAMD conversion incidence rate differences decreased to 5% or less.
Five-Year Model, Direct Ophthalmic Medical Cost Perspective
Changing the model time from 11 to 5 years produced a mean 0.10 QALY gain from Zx supplementation decreasing second-eye conversions in baseline unilateral nAMD cases. The direct ophthalmic medical costs, including Zx costs, expended during this time were $5081 for the cohort receiving Zx supplementation and $6167 for the cohort not receiving Zx supplementation, resulting in a comparative direct ophthalmic medical cost of −$1086 for Zx supplementation. The direct ophthalmic cost perspective CUR was (−$1086/0.10 =) −$10,860 QALY. Zeaxanthin supplementation was dominant vs. none, since Zx supplementation yielded greater patient value for less cost.
Five-Year Model, Societal Cost Perspective
The 0.10 QALY gain remained unchanged. The societal costs associated with Zx supplementation were (1) −$778 in direct non-ophthalmic medical costs, (2) $0 in caregiver costs, and (3) −$896 in wage loss, for a total of −$1674. In conjunction with the direct ophthalmic medical cost of −$1086, the total societal cost for Zx supplementation was (−$1674 + $1086 =) −$2760 per participant with baseline unilateral nAMD. The 5-year model societal CUR was thus (−$2760/0.42 =) −$6571/QALY, and Zx supplementation was again dominant versus no supplementation. No extra direct medical costs were accrued since we demonstrated that no time of life was saved.
Eleven-Year Model, Direct Ophthalmic Medical Cost Perspective Utilizing Bevacizumab Injections Instead of Triple Therapy
When intravitreal injections of bevacizumab were substituted for triple therapy at a frequency commonly utilized in the US for nAMD [1], and assuming visual outcomes were the same with only bevacizumab injections and triple therapy herein, the total direct ophthalmic medical cost per patient for second-eye therapy in the mean patient not receiving Zx supplementation averaged $7315, whereas the average per-patient second-eye cost for those receiving Zx supplementation was $4126. Adding the $3431 Zx cost to this cost ($4126) resulted in an average $7557 cost. Subtracting the cost for no Zx supplementation from the cost for Zx supplementation resulted in a ($7557–$7315 =) $242 direct ophthalmic medical cost when Zx supplementation was undertaken. This resulted in a direct ophthalmic cost-utility ratio of ($242/0.42 QALY =) $576/QALY, slightly higher than the −$576/QALY observed in our 227 patient, baseline unilateral nAMD cohort.
Cost–Benefit Analysis
It is estimated that 168,400 US cases of nAMD occurred in 2018 [52]. Extrapolating this number using the 327.1 million population in 2018 to 331.0 million in 2020 [51] suggests that 170,400 new nAMD cases developed in 2020.
If 67% of new patients presented with unilateral first-eye nAMD involvement, as was the case herein, the new 2020 US unilateral, first-eye nAMD patient number is (170,400 × 0.67 =) 114,173.
The cost–benefit ratio was calculated herein by dividing the $52,530 societal cost gain (benefit) per patient with Zx supplementation by the $3431 cost of Zx supplementation. The result was ($52,530/$3431 =) a discounted, 1531% 11-year return on investment (ROI).
The 11-year societal gain from treating all 114,173 patients with baseline unilateral nAMD was (114,173 × $52,530 =) $6.0 billion, while the Zx supplementation cost for the same cohort was (114,173 × $3431 =) $391.7 million. Thus, ($6.0 billion/$391.7 million) also yielded a 1531% ROI. This was equivalent to a 1-year ROI of 31.3%. When the difference between the relative conversion rate difference of fellow eyes between the Zx-treated and non-Zx-treated cohorts decreased to approximately 5%, caregiver cost differences became negligible. Minimal, if any, money was returned from Zx supplementation, as shown in the societal cost perspective cost–benefit sensitivity analysis in Table 8.
Average Cost-Utility Analysis of the Entire 337 Baseline Cohort Including Unilateral and Bilateral nAMD Cases
All treated 337 baseline eyes (Table S5) had mean 20/125+1 baseline vision and mean 20/160+1 vision at 5 years, carried forward to 6–11 years since data have shown that many VEGF-I-treated nAMD eyes maintain stable baseline vision over 10 years [53] (Table 9). For the historical comparative control cohort receiving no treatment whatsoever, mean nAMD vision was taken from 2-year clinical trial data [1], then by modeling from years 3–11 according to the Lineweaver-Burk meta-analysis by Shah and DelPriore [41] (Table 9).
The weighted average of QALY gain per patient obtained with the direct ophthalmic cost perspective contribution in the entire 337-patient cohort for the average patient presenting with unilateral nAMD (first-eye model) who gained value because there was less second-eye conversion to nAMD from Zx was (67% × 0.42 QALY =) 0.281 QALY. The QALY contribution per patient (33% of the entire 337 cohort) with baseline second-eye or bilateral involvement (second-eye model) was (33% × 1.095 QALY =) 0.361 QALY. Adding the baseline first-eye model contribution per patient QALY gain to that of the presenting second-eye model patient QALY gain indicated that the mean 337-participant cohort patient gained (0.281 QALY + 0.361 QALY =) 0.643 QALY (12.4% QALY gain over no therapy). The 1.045 QALY gain, a 21.1% gain, for participants presenting with baseline second-eye involvement was calculated by comparing the mean utility based upon the mean vision of Zx-treated participants and non-treated patients at each year of the 11-year model (Table 10) and adjusting for one year of life lost from decreased vision associated with no treatment for nAMD.
The direct ophthalmic medical cost perspective, average (compared to no therapy) CUR for triple therapy costs in 337 nAMD patients in addition to Zx supplementation costs in eyes that presented with baseline unilateral nAMD was ($14,213)/0.643 QALY =) $22,105/QALY (Table 10).
The 337-patient societal cost perspective average cost-utility ratio integrated both societal costs and the extra direct medical costs incurred by a 0.25 mean added year of life in the first-eye model and 1.0 year of life gain [1] in the second-eye model (Table 10). The mean societal cost accrued for each study entrant, integrating the direct ophthalmic medical costs and the extra medical costs from prolonged life was −$68,588, the same amount returned to society over 11 years. The societal average cost-utility ratio was therefore (−$68,588/0.643 =) −$106,669/QALY, indicating that therapy was dominant vs. no therapy.
Cost–Benefit of Triple Therapy with Zx Supplementation
At a net societal treatment cost of −$68,293 per patient, the annual saving versus no nAMD therapy from treating the 2020 annual cohort of 170,400 nAMD patients with triple therapy and oral administration of Zx in baseline unilateral nAMD cases theoretically was (−$68,293 × 170,400 =) $11.78 billion returned to society over 11 years. This resulted in a ($68,293/$14,214 =) 480% 11-year ROI for the 11-year direct ophthalmic medical costs, including Zx supplementation. We did not model the entire 337-patient cohort gain of $68,293 utilizing the direct cost of Zx supplementation alone since we could not be certain that Zx benefitted baseline participants with fellow-eye nAMD.
Discussion
It was demonstrated in a 2-year randomized clinical trial that 20 mg daily of oral Zx supplementation significantly decreases conversion of atrophic AMD fellow eyes to nAMD in patients presenting with unilateral nAMD. The results herein further support those data [4, 5] and a very favorable cost-utility ratio for Zx supplementation in unilateral nAMD cases. We did not factor vision into the analysis since we noted similar vision outcomes after nAMD intravitreal treatment with and without Zx supplementation [6]. Because our baseline mean vision differed from that in monotherapy clinical trials [1], and because earlier treatment yields a better vision outcome [42], we also did not have ideal 5-year comparators for vision.
Zeaxanthin Incremental CUA
In a comparative interventional triple therapy study, we previously demonstrated that Zx decreased the 2-year fellow-eye nAMD conversion rate (p = 0.03) [5]. A 2-year randomized clinical trial comparing Zx supplementation and none showed that the Zx–decreased conversion rate relationship was stronger yet (p = 0.02) [6]. Widomska and colleagues [54] noted greater singlet oxygen quenching by Zx than lutein, suggesting a mechanism which might decrease nAMD occurrence.
Cost-Effectiveness
An oft-quoted US cost-effectiveness upper limit for healthcare interventions is $100,000/QALY, though the US has no formal standards [17]. The World Health Organization upper limit is 3 × gross domestic product (GDP) per capita (US 2020 = $195,073), while < 1 × GDP per capita (US 2020 = $65,024) is considered very cost-effective [17]. Zx supplementation with unilateral nAMD is incrementally cost-effective versus no Zx supplementation, and baseline triple therapy with Zx supplementation versus no nAMD therapy for all comers is also cost-effective. The contribution of Zx supplementation for patients presenting with baseline second-eye nAMD involvement, however, is uncertain.
Average prior CURs for nAMD anti-VEGF monotherapy [1] for all presenting new nAMD eyes were noted to be: bevacizumab = $11,033/QALY, ranibizumab = $79,600/QALY and aflibercept = $44,801/QALY, versus our $22,105/QALY with triple therapy/Zx, though 76 of our 399 (19%) participants had baseline 20/400–20/800 vision, versus baseline vision ≥ 20/320 in monotherapy trials [1]. Our $22,105/QALY CUR for triple therapy/Zx for all nAMD entrants is closer to monotherapy with bevacizumab based on CATT [1, 2] than to aflibercept or ranibizumab.
Zeaxanthin and Conversion Incidence
Our 5-year study demonstrated a decreased incidence of conversion to nAMD in second eyes of 22% versus a 48% conversion incidence (p < 0.0001) in CATT [29]. The 5-year, 42%, MPS conversion incidence [30] also differed dramatically from our 22% incidence (p < 0.0001). The Three Continent AMD Consortium Report [47] noted a 44% 5-year fellow-eye conversion rate (p < 0.0001) for someone presenting with unilateral nAMD. We believe these studies without Zx treatment support the concept that Zx supplementation decreases nAMD conversion.
Vision
While some studies suggest that carotenoid supplementation has improved vision [55], we could not demonstrate this in our previous clinical trial [6] or herein except by the mechanism of Zx supplementation reducing the incidence of nAMD in fellow eyes [6]. We are therefore uncertain whether Zx supplementation for eyes that already have nAMD leads to improved vision above that obtained with intravitreal injection therapy without Zx-supplementation.
Intravitreal Injections
While anti-VEGF monotherapy prevents PDT adverse events, ranibizumab and bevacizumab 11-year per-eye nAMD therapies both required a mean of 51.2 intravitreal injections [1], versus our triple therapy’s 19.3 intravitreal injections for bevacizumab and dexamethasone combined, approximately 38% of the intravitreal injections needed with anti-VEGF monotherapies [1].
Bilateral nAMD Treatment
We believe bilateral treatment, when indicated in the first-eye model, gives superior binocular vision, maximizes quality of life, and decreases overall blindness. Half of our baseline unilateral eyes receiving triple therapy had 5-year vision ≤ 20/200. Treating patients bilaterally, however, yields ≤ 20/200 vision in 25% (50% × 50%) of patients, rather than 50% [5]. Thus, we believe bilateral nAMD therapy should be undertaken when indicated.
Mechanisms of Zx Action [54]
Macula-concentrated Zx comprises 75% of retinal carotenoids, versus the peripheral 25% lutein component. Unlike lutein, Zx reduces light-induced cone/rod apoptosis in quail. Zeaxanthin also filters energy-containing blue light to a greater extent than lutein. This phenomenon limits destructive singlet oxygen production thought to play a role in nAMD formation. Furthermore, Zx may also promote macular retinal pigment concentration and increased cell survival [55].
Adverse events We observed no adverse events with Zx and are unaware of any reported. Rodents given 1000 mg/kg/day and dogs on 400 mg/kg/day also had none. The European Nutrition, Novel Foods and Food Allergens Panel recommended a safety factor not to exceed 53 mg/day for a 70-kg adult, well above our 20 mg daily dose [56].
Prevention Trumps Treatment
Our incremental CUA demonstrates that nAMD second-eye prevention is superior to treatment in baseline unilateral nAMD cases [1]. Not only does Zx supplementation prevention yield a greater QALY gain versus no supplementation, but it is less costly and results in a large ROI for the Zx supplementation cost. It has been previously shown that 80% of cost saving is returned to patients [1]. From a societal cost perspective, $63,135 is saved in caregiver costs, and most of $52,530 is returned to baseline unilateral nAMD patients, who spend less due to better vision from decreased nAMD conversion.
Nonetheless, because Zx supplementation saves 0.25 life-years at age 90 by reducing fellow-eye nAMD, there is $10,847 excess non-ophthalmic, direct medical cost over the 0.25 years accrued to insurers. This illustrates the important issue that time of life saved can increase overall medical costs [1]. For example, if all smokers stopped smoking, healthcare costs accrued with age would exceed those saved from not smoking by 15 years after tobacco cessation [57].
Prevention is superior to treatment for other conditions as well, including heart transplant rejection [58], recurrent ischemic stroke [59], wound site infection [60], malaria [61] and others.
Study Limitations
Comparing 11-year, unilateral nAMD treatment cohort data in patients with and without Zx supplementation would be ideal, rather than using post hoc historical control data with 2 mg Zx supplementation daily [6, 62]. We believe, however, that new drugs, delivery systems and other advances make the likelihood of an 11-year clinical trial low. Furthermore, deleting a daily 2-mg Zx dose now from unilateral nAMD cases is unethical [6, 62, 63]. That said, our previous 2-year clinical trial [5] did demonstrate a risk reduction for nAMD occurrence with 20-mg Zx supplementation versus a cohort control not receiving Zx supplementation when both took daily AREDS2 supplements containing 2 mg of Zx.
Testing each of the different anti-VEGF nAMD monotherapies with and without Zx-supplementation might also be highly desirable. The DENALI [64] and MONT BLANC [65] studies, however, both demonstrated similar vision outcomes with ranibizumab versus ranibizumab with PDT. From this information, our earlier clinical trial results [5, 6], and the current analysis, we believe the evidence is sufficiently robust to suggest a beneficial effect of Zx independent of monotherapy or triple therapy. We are not aware that PDT, intravitreal corticosteroids, or anti-VEGF monotherapies given unilaterally inhibit fellow-eye nAMD.
The fact that bevacizumab was the only anti-VEGF monotherapy we utilized could be a drawback, though vision outcomes for the three most commonly used intravitreal anti-VEGF monotherapies (ranibizumab, aflibercept and bevacizumab) have been shown to be similar [1]. CATT also previously showed that the risk of developing nAMD in fellow eyes is independent of whether ranibizumab or bevacizumab is used in initial eyes [2, 29, 30].
We are uncertain whether the use of predominantly AREDS2 supplements in our participants, which added 2-mg oral zeaxanthin daily to the 20-mg Zx supplemental therapy dose is relevant. The CATT participants (enrolled during 2008–2009) used supplements in 90% of cases but did not have the AREDS2 formula with 2 mg zeaxanthin/10 mg lutein available until 2013. The AREDS2 Research Group Report No. 3 [6] noted that the zeaxanthin 2 mg/lutein 10 mg combination did not influence vision, though the 10-year hazard ratio for progression to late AMD comparing lutein/zeaxanthin to no lutein/zeaxanthin was 0.91 (p = 0.02). Our 5-year hazard ratio was approximately 0.46 (p < 0.0001) with 20 mg of additional daily Zx supplementation over the 2 mg in AREDS2 supplements.
Study Strengths
A strength of this study is the 89% 5-year follow-up on the 227-patient unilateral nAMD cohort and 90.5% follow-up on all 337 baseline patients, both high relative to other studies [29, 30].
Our patient-acquired ocular utilities are also a strength. Reliable and validated, they are typically unaffected by age [16, 22, 23], gender [16, 22], educational level [16, 22], underlying ocular disease [24], systemic comorbidities [25, 26], or race [66], and are similar in multiple countries [66].
It bears repeating that our 2-year, triple-blind, randomized clinical trial demonstrated that Zx supplementation in unilateral baseline nAMD cases significantly reduced nAMD conversion in fellow eyes (p = 0.02) [6]. The current study was conducted to ascertain whether the nAMD reduction rate persisted at 5 years. While we lacked an internal 5-year control cohort, we believe that our data compared to CATT [2, 28, 39] and other clinical trial [31, 45, 47] results strongly support the protective effect of Zx in preventing nAMD.
Conclusions
Participants with baseline unilateral nAMD on long-term oral Zx supplementation demonstrated a reduction in fellow-eye nAMD conversion versus historical controls not receiving Zx supplementation at 5 years. Supplementation with zeaxanthin to prevent fellow-eye nAMD is extremely cost-effective by conventional US standards, returns monies to society, and likely prevents loss of life-years from poorer vision. Zx supplementation in an 11-year cohort of US unilateral nAMD patients would return a net $6.0 billion to society, predominantly to patients.
References
Brown GC, Brown MM, Rapuano SB, Boyer D. Patient preference-based cost-utility analysis of VEGF-inhibitor therapy for neovascular age-related macular degeneration in the United States in 2018. Am J Ophthalmol. 2020;218:225–41. https://doi.org/10.1016/j.ajo.2020.05.029. (Epub 2020 Jun 19).
Maguire M.G., Martin D.F., Ying G., et al., for the Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group Writing Committee. Five-year outcomes with anti-vascular endothelial growth factor treatment of neovascular age-related macular degeneration. The comparison of age-related macular treatments trials. Ophthalmology 2016; 123:1751–1761. doi: https://doi.org/10.1016/j.ophtha.2016.03.045. Epub 2016 May 2.
Ando R, Hirooka K, Saito M, et al. Two-year clinical outcomes of triple therapy with photodynamic therapy, anti-vascular endothelial growth factor agent, and triamcinolone acetonide for neovascular age-related macular degeneration. Jpn J Ophthalmol. 2023;67:50–8. https://doi.org/10.1007/s10384-022-00955-8. (Epub 2022 Nov 8).
Kovacs KD, Quirk MT, Kinoshita T, et al. A retrospective analysis of triple combination therapy with intravitreal bevacizumab, posterior sub-tenon's triamcinolone acetonide, and low-fluence verteporfin photodynamic therapy in patients with neovascular age-related macular degeneration. Retina. 2011; 31:446–52. doi: https://doi.org/10.1097/IAE.0b013e3181f6391f, http://www.ncbi.nlm.nih.gov/pubmed/21336068.
Olk RJ, Peralta E, Gierhart DL, et al. Triple combination therapy and zeaxanthin for the treatment of neovascular age-related macular degeneration: an interventional comparative study and cost-effectiveness analysis. Int J Retin Vitr. 2015. https://doi.org/10.1186/s40942-015-0019-2. (eCollection 2015).
Olk RJ, Peralta E, Gierhart DL, et al. Combination therapy with dietary zeaxanthin for neovascular age-related macular degeneration. A randomized clinical trial. J Clin Exp Ophthalmol. 2017;8:692. https://doi.org/10.4172/2155-9570.
The Age-Related Eye Disease Study 2 (AREDS2) Research Group. Secondary analyses of the effects of lutein/zeaxanthin on age-related macular degeneration progression: AREDS2 report No. 3. JAMA Ophthalmol. 2014;132:142–9. https://doi.org/10.1001/jamaophthalmol.2013.7376.
Biswal MR, Justis BD, Han P, Li H, et al. Daily zeaxanthin supplementation prevents atrophy of the retinal pigment epithelium (RPE) in a mouse model of mitochondrial oxidative stress. PLoS ONE. 2018;13(9): e0203816. https://doi.org/10.1371/journal.pone.0203816.
Rosen R, Vagaggini T, Chen Y, Hu DN. Zeaxanthin inhibits hypoxia-induced VEGF secretion by RPE cells through decreased protein levels of hypoxia-inducible factors-1a. Biomed Res Int. 2015. https://doi.org/10.1155/2015/687386. (Epub 2015 Jan 20).
Seddon JM, Ajani UA, Sperduto RD, et al. Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration. Eye Disease Case-Control Study Group. JAMA. 1994;272:1413–20 (PMID: 7933422).
Delcourt C, Carriere I, Delange M, and the POLA Study Group. Plasma lutein and zeaxanthin and other carotenoids as modifiable risk factors for age-related maculopathy and cataract: The POLA Study. Invest Ophthalmol Vis Sci. 2006;47:2329–35. https://doi.org/10.1167/iovs.05-1235.
Gale CR, Hall NF, Phillips DI, Martyn CN. Lutein and zeaxanthin status and risk of age-related macular degeneration. Invest Ophthalmol Vis Sci. 2003;44:2461–5. https://doi.org/10.1167/iovs.02-0929.
Zhou H, Zhao X, Johnson E, et al. Serum carotenoids and risk of age-related macular degeneration in a Chinese population. Invest Ophthalmol Vis Sci. 2011;52:4338–44. https://doi.org/10.1167/iovs.10-6519.
Evans JR, Lawrenson JG. Antioxidant vitamin and mineral supplements for slowing the progression of age-related macular degeneration. Cochrane Database Syst Rev. 2017;7:CD000254. https://doi.org/10.1002/14651858.CD000254.pub4.
Brown GC, Brown MM, Busbee B. Cost-utility analysis of cataract surgery in the United States in 2018. J Cataract Refract Surg. 2019;45(7):927–38. https://doi.org/10.1016/j.jcrs.2019.02.006.
Brown MM, Brown GC, Sharma S, Landy J. Health care economic analyses and value-based medicine. Surv Ophthalmol. 2003;48:204–23. https://doi.org/10.1016/s0039-6257(02)00457-5.
Brown MM, Brown GC, Sharma S. Evidence-based to value-based Medicine. Chicago: AMA Press; 2005. p. 1–324.
Sanders GD, Neumann PJ, Basu A, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses, second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–103 (PMID: 27623463).
Sharma S, Brown GC, Brown MM, Hollands H, Robbins R, Shah G. Validity of the time trade-off and standard gamble methods of utility assessment in retinal patients. Br J Ophthalmol. 2002;86:493–6. https://doi.org/10.1136/bjo.86.5.493.
Brown GC, Brown MM, Sharma S, Beauchamp G, Hollands H. The reproducibility of ophthalmic utility values. Trans Am Ophthalmol Soc. 2001;99:199–203 (PMID: 11797307).
Hollands H, Lam M, Pater J, Albiani D, Brown GC, Brown MM, Cruess AF, Sharma S. Reliability of the time trade-off technique of utility assessment in patients with retinal disease. Can J Ophthalmol. 2001;36:202–9.
Brown MM, Brown GC, Sharma S, Kistler J, Brown H. Utility values associated with blindness in an adult population. Br J Ophthalmol. 2001;85:327–31. https://doi.org/10.1136/bjo.85.3.327.
Brown GC, Brown MM, Stein JD, Smiddy WE, Ophthalmic Utility Research Study Group. Vision-related quality-of-life associated with unilateral and bilateral ocular conditions. Ophthalmology. 2018;125:965–71. https://doi.org/10.1016/j.ophtha.2017.12.033. (Epub 2018 Feb 21).
Brown MM, Brown GC, Sharma S, Landy J. Quality of life with visual acuity loss from diabetic retinopathy and age-related macular degeneration. Arch Ophthalmol. 2002;120:481–4. https://doi.org/10.1001/archopht.120.4.481.
Brown MM, Brown GC, Sharma S, Hollands H. Quality-of-life and systemic comorbidities in patients with ophthalmic disease. Br J Ophthalmol. 2002;86:8–11. https://doi.org/10.1136/bjo.86.1.8.
Real FJ, Brown GC, Brown HC, Brown MM. The effect of comorbidities upon ocular and systemic health-related quality of life. Br J Ophthalmol. 2008;92:770–4. https://doi.org/10.1136/bjo.2007.127407. (Epub 2008 Apr 17).
CMS.gov. Search the physician fee schedule. From the Internet @ https://www.cms.gov/medicare/physician-fee-schedule/search. Accessed 12 Sep 2021.
Arias E, Xu JQ. United States life tables, 2017. National Vital Statistics Reports; vol 68 no 7. Hyattsville, MD: National Center for Health Statistics. 2019. (PMID: 32501200).
Maguire M, Pan W, Grunwald JE, et al. for the Comparison of AMD treatments trials study group. In: ARVO poster, ARVO Annual Meeting Abstract, June 2017. Investigative Ophthalmology & Visual Science June 2017, Vol.58, 2323.
Maguire MG, Daniel E, Shah AR, et al. Incidence of choroidal neovascularization in the fellow eye in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2013;120:2035–41. https://doi.org/10.1016/j.ophtha.2013.03.017. (Epub 2013 May 22).
Macular Photocoagulation Study Group. Risk factors for choroidal neovascularization in the second eye of patients with juxtafoveal or subfoveal choroidal neovascularization second to age-related macular degeneration. Arch Ophthalmol. 1997;115:741–7. https://doi.org/10.1001/archopht.1997.01100150743009.
Javitt JC, Zhou Z, Willke RJ. Association between visual loss and higher medical care costs in Medicare beneficiaries. Ophthalmology. 2007;114:238–45. https://doi.org/10.1016/j.ophtha.2006.07.054.
Consumer Price Index, U.S. Bureau of Labor Statistics. Price inflation for medical care since 1935. From the Internet @ https://www.in2020dollars.com/Medical-care/price-inflation, Accessed 14 Apr 2022.
Brown MM, Brown GC, Lieske HB, et al. Societal costs associated with neovascular age-related macular degeneration in the United States. Retina. 2016;36:285–98. https://doi.org/10.1097/IAE.0000000000000717.
Bureau of Labor Statistics. Employment status of the civilian noninstitutional population by age, sex, and race. From the Internet @ https://www.bls.gov/cps/cpsaat03.htm. Accessed 26 Oct 2021.
Taylor DM. Americans with Disabilities: 2014, Household Economic Studies, Current Population Reports. Washington, DC, U.S. Department of Commerce Economics and Statistics Administration U.S. CENSUS BUREAU, 2018; pp 1–32.
Statista. Annual wage and salary accruals per full-time equivalent in the United States from 2000 to 2020. From the Internet @ https://www.statista.com/statistics/243842/annual-mean-wages-and-salary-per-employee-in-the-us/#:~:text=In%202020%2C%20the%20average%20wage%20and%20salary%20per,States%20from%202000%20to%202020%20%28in%20U.S.%20dollars%29. Accessed 1 May 2022.
Consumer Price Index, U.S. Bureau of Labor Statistics. Consumer Price Index, U.S. Bureau of Labor Statistics. CPI for all urban consumers. From the Internet @ https://data.bls.gov/cgi-bin/surveymost, Accessed 14 Oct 2022.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–81.
Powerandsamplesize.com. 2 Proportions: 2-Sample, 2-Sided Equality. From the Internet @ http://powerandsamplesize.com/Calculators/Compare-2-Proportions/2-Sample-Equality. Accessed 28 June 2022.
Shah AR, Del Priore LV. Progressive visual loss in subfoveal exudation in age-related macular degeneration: a meta-analysis using Lineweaver-Burke plots. Am J Ophthalmol. 2007;143:83–9. https://doi.org/10.1016/j.ajo.2006.09.043. (Epub 2006 Oct 20).
Boyer DS, Antoszyk AN, Awh CC, et al. Subgroup analysis of the MARINA study of ranibizumab in neovascular age-related macular degeneration. Ophthalmology. 2007;114:246–52. https://doi.org/10.1016/j.ophtha.2006.10.045.
Zarranz-Ventura J, Liew G, Johnston RL, et al. The neovascular age-related macular degeneration database: report 2: incidence, management, and visual outcomes of second treated eyes. Ophthalmology. 2014;121(10):1966–75.
Fasler K, Fu DJ, Moraes G, et al. Moorfields AMD database report 2: fellow eye involvement with neovascular age-related macular degeneration. Br J Ophthalmol. 2020;104(5):684–90. https://doi.org/10.1136/bjophthalmol-2019-314446. (Epub 2019 Oct 14).
Starr MR, Xu D, Boucher N, et al. Characterizing progression to neovascular AMD in fellow eyes of patients treated with intravitreal anti-VEGF injections. Ophthalmic Surg Lasers Imaging Retina. 2021;52(3):123–8. https://doi.org/10.1016/j.ophtha.2014.04.026. (Epub 2014 Jun 20).
Barbazetto IA, Saroj N, Shapiro H, et al. Incidence of new choroidal neovascularization in fellow eyes of patients treated in the MARINA and ANCHOR trials. Am J Ophthalmol. 2010;149:939–46. https://doi.org/10.1016/j.ajo.2010.01.007. (Epub 2010 Apr 8).
Parikh R, Avery RL, Saroj N, Thompson D, Freund KB. Incidence of new choroidal neovascularization in fellow eyes of patients with age-related macular degeneration treated with intravitreal aflibercept or ranibizumab. JAMA Ophthalmol. 2019;137(8):914–20. https://doi.org/10.1001/jamaophthalmol.2019.1947.
Joachim N, Colijn JM, Kifley A, et al. Five-year progression of unilateral age-related macular degeneration to bilateral involvement: the Three Continent AMD Consortium report. Br J Ophthalmol. 2017;101:1185–92. https://doi.org/10.1136/bjophthalmol-2016-309729. (Epub 2017 Jan 20).
Christ SL, Zheng DD, Swenor BK, et al. Longitudinal relationships among visual acuity daily functional status, and mortality. The Salisbury Eye Evaluation Study. JAMA Ophthalmol. 2014;132:1400–6. https://doi.org/10.1001/jamaophthalmol.2014.2847.
Webb A, Zhivan N. How much is enough? The distribution of lifetime health care costs. From the Internet @ https://crr.bc.edu/wp-content/uploads/2010/02/wp_2010-1-508.pdf Accessed 29 10 2021.
MacroTrends. US population 1950–2021, from the Internet @ www.macrotrends.net/countries/USA/united-states/population, Accessed 28 Oct 2022.
Brown GC, Brown MM, Rapuano SB, Boyer D. A cost-benefit analysis of VEGF-Inhibitor therapy for neovascular age-related macular degeneration in the United States. Am J Ophthalmol. 2021;223:405–29. https://doi.org/10.1016/j.ajo.2020.07.010. (Epub 2020 Jul 16).
Spooner K, Fraser-Bell S, Thomas Hong T, et al. Long-term anti-vascular endothelial growth factor treatment for neovascular age-related macular degeneration: the LATAR Study: report 1: ten-year real-world outcomes. Ophthalmol Retina. 2021;5:511–8. https://doi.org/10.1016/j.oret.2020.09.019. (Epub 2020 Sep 29).
Widomska J, SanGiovanni JP, Subczynski WK. Why is zeaxanthin the most concentrated xanthophyll in the central fovea? Nutrients. 2020;12:1333. https://doi.org/10.3390/nu12051333.
Le, DW, Davey PG, Gierhart DL, Rosen RB. A systematic review of carotenoids in the management of age-related macular degeneration. Antioxidants. 2021;10:1255. https://doi.org/10.3390/antiox10081255.
Edwards JA. Zeaxanthin: review of toxicological data and acceptable daily intake. J Ophthalmol. 2016. https://doi.org/10.1155/2016/3690140. (Article ID 3690140, Epub 2016 Jan 13).
Barendregt JJ, Luc Bonneaux MA, van der Mass PJ. The health care costs of smoking. N Engl J Med. 1997;337:1052–70. https://doi.org/10.1056/NEJM199710093371506.
Knechtle SJ, Kwun J, Iwakoshi N. Prevention trumps treatment of antibody-mediated transplant rejection. J Clin Invest. 2010;120(4):136–9. https://doi.org/10.1172/JCI42532. (Epub 2010 Mar 24).
Oza R, Rundell K, Garcellano M. Recurrent ischemic stroke: Strategies for prevention. Am Fam Physician. 2017;96(7):436–40 (PMID: 29094912).
Allegranzi B, Zayed B, Bischoll P, et al. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;12:e288–303. https://doi.org/10.1016/S1473-3099(16)30402-9. (Epub 2016 Nov 2).
Van Vught M, van Beest A, Sicuri E, et al. Malaria treatment and prophylaxis in endemic and nonendemic countries: evidence on strategies and their cost-effectiveness. Future Microbiol. 2011;6(12):1485–500. https://doi.org/10.2217/fmb.11.138.
Chew EY, Clemons TE, Agrón E, for the AREDS2 Research Group, et al. Long-term Outcomes of adding lutein/zeaxanthin and ω-3 fatty acids to the AREDS supplements on age-related macular degeneration progression: AREDS2 report 28. JAMA Ophthalmol. 2022;140:692–8. https://doi.org/10.1001/jamaophthalmol.2022.1640.
Scoles D, Ying GS, Maguire MG. Characteristics of eyes with good visual acuity at 5 Years after initiation of treatment for age-related macular degeneration but not receiving treatment from years 3 to 5. Post hoc analysis of the CATT randomized clinical trial. Supplementary Materials. JAMA Ophthalmol. 2020;138(3):276–94. https://doi.org/10.1001/jamaophthalmol.2019.5831.
Kaiser PK, Boyer DS, Cruess AF, on behalf of the DENALI Study Group, et al. Verteporfin plus ranibizumab for choroidal neovascularization in age-related macular degeneration. Twelve-month results of the DENALI Study. Ophthalmology. 2012;119:1001–10. https://doi.org/10.1016/j.ophtha.2012.02.003. (Epub 2012 Mar 22).
Larsen M, Schmidt-Erfurth U, Lanzetta P, on behalf of the MONT BLANC Study Group, et al. Verteporfin plus ranibizumab for choroidal neovascularization in age-related macular degeneration. Twelve-month MONT BLANC Study results. Ophthalmology. 2012;119:992–1000. https://doi.org/10.1016/j.ophtha.2012.02.002. (Epub 2012 Mar 17).
Brown GC, Brown MM. A preference-based comparison of the quality-of-life associated with vision loss in Black and White American populations. Can J Ophthalmol. 2022. https://doi.org/10.1016/j.jcjo.2022.11.003.
Acknowledgements
The authors want to thank Sharon Christ PhD, Department of Human Development and Family Studies, Purdue University, West Lafayette, Indiana, for her assistance providing mortality data associated with vision loss. The authors also want to thank Maureen Maguire, PhD, Professor of Ophthalmology and Director of the Center for Preventive Ophthalmology and Biostatistics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA for providing 5-year and other information on the Comparison of AMD Treatments Trials. The authors thank the participants in the study for their roles in advancing scientific knowledge.
Funding
Performance of the study, manuscript preparation, and the Rapid Service Fee were supported in part by a grant from ZeaVision, Inc., Chesterfield, MO. Dr. G. Brown had full control of all data and agreed to allow the grantor to review the data upon request. The funder played no role in the design, conduct, or reporting of the analysis.
Medical Writing and Editorial Assistance
This article did not receive any medical writing support or editorial assistance.
Author Contributions
Gary C. Brown, Melissa M. Brown, Dennis Gierhart, and R. Joseph Olk participated in the conceptualization of the study and the design of the study. R. Joseph Olk enrolled and examined the participants. Gary C. Brown and Melissa M. Brown performed the analyses. Gary C. Brown, Melissa M. Brown, Dennis Gierhart and R. Joseph Olk wrote the manuscript. All authors read, critiqued, and approved the final manuscript.
Prior Presentation
Data herein were presented in part at following 2020 virtual meetings: Jules Gonin Society, Retina Society, and the American Society of Retina Specialists.
Disclosures
R. Joseph Olk and Dennis Gierhart have shares in ZeaVision. Gary C. Brown and Melissa M. Brown are shareholders in the Center for Value-Based Medicine®, a healthcare economic research organization that received grant funding for data analysis and writing the manuscript.
Compliance with Ethics Guidelines
The Wills Eye Hospital IRB approved utility acquisition, and adherence to the Declaration of Helsinki and its amendments was observed. The SSM Health Care Institutional Review Board approved triple therapy with Zx-supplementation (approval number 14–07-0540). The ClinicalTrials.gov identifier for the original randomized clinical trial was NCT 01527435.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Brown, G.C., Brown, M.M., Gierhart, D. et al. Prevention Surpasses Treatment: 5-year Follow-Up, Cost-Utility, and Cost–Benefit of Zeaxanthin Therapy for Neovascular Age-Related Macular Degeneration. Ophthalmol Ther 12, 2583–2608 (2023). https://doi.org/10.1007/s40123-023-00742-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00742-9