Abstract
Introduction
Intraocular inflammation (IOI)-related adverse events (AEs) that may result in severe vision loss have been associated with the anti-vascular endothelial growth factor brolucizumab. In this study, we investigate the timing, management and resolution of IOI-related AEs in a large cohort of patients treated with at least one injection of brolucizumab in routine clinical practice.
Methods
Retrospective review of medical records from patients with neovascular age-related macular degeneration treated with ≥ 1 brolucizumab injection between October 2019 and November 2021 at the Retina Associates of Cleveland, Inc. clinics.
Results
Of the 482 eyes included in the study, IOI-related AEs occurred in 22 (4.6%) eyes. Four (0.8%) eyes developed retinal vasculitis (RV) and of these, 2 (0.4%) had concomitant retinal vascular occlusion (RO). Most eyes [14/22 (64%)] developed the AE within 3 months and 4/22 (18%) within 3–6 months of the first brolucizumab injection. The median [interquartile range (IQR)] time from the last brolucizumab injection to development of the IOI-related AE was 13 (4–34) days. At the time of event, 3 (0.6%) eyes with IOI (no RV/RO) developed severe vision loss of ≥ 30 ETDRS letters, and a further 5 (1.0%) eyes (1 with IOI + RV, 1 with IOI + RV + RO) developed moderate vision loss of ≥ 15 letters compared with their last visual acuity (VA) prior to the AE. The median (IQR) vision loss was −6.8 (−19.9, –0.0) letters. Taking the best VA at either 3 or 6 months after AE resolution (or stability for occlusive events), VA decreased by ≥ 5 letters compared with prior to the AE in 3 (14%) of the 22 affected eyes, and was preserved (< 5-letter loss) in 18 (82%) eyes.
Conclusions
In this real-world study, most IOI-related AEs occurred early after brolucizumab treatment initiation. With appropriate monitoring and management of IOI-related AEs, vision loss associated with brolucizumab may be limited.
Similar content being viewed by others

Why carry out this study? |
Intraocular inflammation (IOI)-related adverse events (AEs) have been associated with the use of brolucizumab, but current real-world data are from studies with either small sample sizes or with a relatively short follow-up period. |
What was learned from the study? |
In the 482 patients who received ≥ 1 injection with brolucizumab between 1 October 2019 and 30 November 2021 at one of the Retina Associates of Cleveland Inc, clinics in Northeast Ohio, USA, IOI-related AEs were identified in 22 (4.6%) eyes. |
The risk of an IOI-related AE decreased with time since first brolucizumab injection and number of previous brolucizumab injections. Three of the 22 eyes (14%) eyes had ≥ 5-letter loss within 6 months of AE resolution (or stability for occlusions) compared with before the event. |
With appropriate monitoring, particularly during the first months of therapy, and management of IOI-related AEs, vision loss associated with brolucizumab may be limited. |
Introduction
Neovascular (wet) age-related macular degeneration (nAMD) is an advanced form of AMD characterized by choroidal neovascularization (CNV) and the accumulation of subretinal fluid (SRF) and intraretinal fluid (IRF) [1, 2]. Intravitreal anti-vascular endothelial growth factor (VEGF) agents are the current standard of care for treating nAMD [3]. Brolucizumab, a single-chain antibody fragment that inhibits all isoforms of VEGF-A [4], gained US Food and Drug Administration (FDA) approval for the treatment of nAMD in October 2019, based on the results from the Phase III HAWK and HARRIER trials [5,6,7,8].
Following FDA approval there were post-marketing reports of retinal vasculitis (RV), including retinal occlusive vasculitis [9]. Novartis initiated an internal review of these post-marketing reports, which included the establishment of an external Safety Review Committee to provide an independent objective review of these cases along with a comparison with events seen in HAWK and HARRIER. Subsequently, a safety signal of RV and/or retinal vascular occlusion (RO) that may result in severe vision loss was confirmed. Typically, these events occur in the presence of intraocular inflammation (IOI) [10].
The aim of this study was to investigate IOI-related and non-IOI-related adverse events (AEs) in a cohort of patients with nAMD who initiated brolucizumab treatment in routine clinical practice in the USA, in particular the timing of any IOI-related AEs and the associated visual outcomes. Three clinical cases are presented to provide insights into the management of IOI-related AEs associated with the use of brolucizumab.
Methods
Study Cohort
This retrospective real-world review is from medical records of patients with nAMD treated with brolucizumab 6 mg from the Retina Associates of Cleveland, Inc. (RACI), one of the largest retina practices in the USA, with 13 offices that serve Northeast Ohio. A study cohort comprised all patients who received their first brolucizumab injection (index) between 1 October 2019 and 30 November 2021 (the study period). Both treatment-naïve (not treated with any anti-VEGF therapy in the 12 months before index) and prior-treated eyes (treated with a different anti-VEGF therapy in the 12 months before index) were included. Anonymized patient data were extracted on 1 December 2021 and included all patient eyes who received ≥ 1 brolucizumab injection during the study period.
Ethics Statement
Patients provided consent to have their deidentified data used for research purposes. This study complied with the tenets of the Declaration of Helsinki and is based on a retrospective analysis of deidentified data obtained as part of routine clinical practice. All patient data were collected in accordance with the Health Insurance Portability and Accountability Act (https://www.cdc.gov/phlp/publications/topic/hipaa.html). As this study constituted a secondary analyses on fully anonymized data, Institutional Review Board or additional informed consent was not required in line with the Code of Federal Regulations Code 46.104 (d) (1) (2) (i).
Study Endpoints
Clinical characteristics of the study cohort collected at the time of the first brolucizumab injection (the index date) included visual acuity (VA), last injection interval for prior-treated eyes (defined as the time between the last preswitch anti-VEGF injection and the first brolucizumab injection), and central macular thickness (CMT). For the duration of the study period, the number of eyes with an IOI-related AE and with an ocular AE not associated with IOI were recorded by AE type. However, as the particular focus of this study was on RV and RO in the presence of IOI, the latter were not analyzed further. We also report the distribution of the number of brolucizumab injections in eyes with and without IOI-related AEs, the time from first brolucizumab injection to IOI-related AE (in eyes with IOI-related AE) or to end of follow-up (in eyes without AE), time from last brolucizumab injection to IOI-related AE, and the probability of experiencing an IOI-related AE during the follow-up period. Finally, we also investigate the time from AE to resolution (or stability in the case of occlusive events) and the visual outcomes in patients experiencing an IOI-related AE.
Statistical Methods
These analyses were descriptive in nature with the eye as the unit of analysis. Kaplan–Meier modelling of the real-world probability of brolucizumab-treated eyes experiencing an IOI-related AE after initiating brolucizumab treatment was performed and the detailed method is included in Supplementary Fig. 1. The change in VA at 3 or 6 months after AE resolution was derived by subtracting the most recent VA value pre-AE from the VA value after AE resolution. The VA value measured closest to day 90 and day 180 post-AE resolution was used to define the VA value at 3 months and 6 months, respectively. VA was converted from Snellen numerators, denominators and logMAR values to Early Treatment Diabetic Retinopathy Study (ETDRS) letters, as described by Gregori et al. [11].
Results
Characteristics of the Study Cohort
The study cohort comprised all eyes at RACI receiving at least one brolucizumab injection in the study period, totaling 482 eyes from 414 patients. Of these, 22 eyes were treatment-naïve, whereas the other 460 eyes had received a previous anti-VEGF in the 12 months prior to the index date. At the time of first brolucizumab injection, the mean [standard deviation (SD)] patient age was 81.1 (9.1) years, VA was 58.3 (21.6) letters, and CMT was 297.2 (102.9) μm (Table 1).
Incidence of Ocular Adverse Events and Associated Vision Loss
IOI-related AEs were identified in 22/482 (4.6%) eyes from 21 patients who received at least one injection with brolucizumab (Table 2). Characteristics of the subgroup of eyes with IOI-related AEs at the time of first injection were similar to the overall cohort except for a slightly higher proportion of female patients in the subgroup of eyes with IOI-related AEs (66.7% versus 58.0%, respectively) (Table 1). The most common single AE types were posterior uveitis (5 eyes, 1.0%), anterior uveitis (4 eyes, 0.8%), and panuveitis (4 eyes, 0.8%). Another 4 eyes (0.8%) had RV and of these, 1 had concomitant anterior uveitis, and 2 (0.4%) had concomitant RO [1 also with panuveitis (Table 2)].
At the time of event, 3 (0.6%) eyes with IOI-related AEs (but no RV/RO) developed severe vision loss of ≥ 30 letters compared with their last VA measurement prior to the AE, two with endophthalmitis and one with posterior uveitis (see clinical cases section for further details on this last case and Supplementary Table S1 for visual outcomes for all three cases). A further 5 (1.0%) eyes (3 with IOI alone, 1 with IOI + RV, and 1 with IOI + RV + RO) developed moderate vision loss of ≥ 15 letters compared with their last VA prior to the AE (Supplementary Table S1). Focusing on the eyes with RV/RO, the eye with IOI + RV had a pre-AE VA of 61 letters that decreased to 35 letters at the time of AE and the eye with IOI + RV + RO had a pre-AE VA of 55 letters decreasing to 35 letters (see clinical cases section for further details). This represents an overall risk of 0.4% (2/482) of developing IOI + RV and 0.2% (1/482) of developing IOI + RV + RO and experiencing at least moderate vision loss, defined as the loss of ≥ 15 letters. The other eye that developed IOI + RV + RO did not lose vision and the remaining eye with RV lost 11 letters (76 decreasing to 65 letters) at the time of event. The visual outcomes of all 22 eyes with IOI-related AEs following AE resolution/stability are described in the section below.
Ocular AEs that were not associated with IOI were identified in 6/482 (1.2%) eyes from 6 patients (Table 2). Two of these AEs [hemorrhage (submacular/subretinal) and retinal detachment] resulted in severe vision loss of ≥ 30 letters that was sustained for at least 6 months post-AE. Two eyes that developed punctate keratitis and macular hole initially lost 9 and 20 letters, respectively, and VA returned to pre-AE levels within 6 months; the other 2 eyes maintained vision throughout the event.
Number of Brolucizumab Injections in the Study Cohort
Until the end of the study period, the 460 (95.4%) brolucizumab-treated eyes that did not experience any IOI-related AEs received a median of five injections, with 172/460 (37%) of these eyes receiving at least nine injections with brolucizumab (Fig. 1A). As per label [5, 6], brolucizumab should be discontinued after an inflammatory event and accordingly, eyes with IOI-related AEs received a median of three brolucizumab injections (range, 1–8); 5 (23%) received one brolucizumab injection, 6 (27%) two injections, 5 (23%) three injections, and 6 (27%) four or more injections (Fig. 1A) before their IOI-related AE and their subsequent discontinuation of brolucizumab treatment.
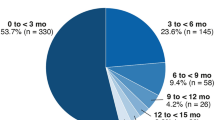
A Brolucizumab injection distribution in eyes with and without IOI-related AEs. B Time from the first brolucizumab injection until the IOI-related AE (dark grey bars) or end of follow-up (light grey bars). Percentages are presented above bars, and the absolute numbers of eyes in each category are presented at bar base. AE, adverse event; IOI, intraocular inflammation
Time from First Brolucizumab Injection to IOI-Related AE or End of Follow-Up
The majority of eyes [14/22 (64%)] developed the IOI-related AE within 90 days of the first brolucizumab injection: 3 (14%) in the first 30 days, 5 (23%) between 31 and 60 days, and 6 (27%) between 61 and 90 days inclusive (Fig. 1B). The median time between the first brolucizumab injection and the AE was 68 days (IQR, 50–160 days) and all IOI-related AEs occurred within 540 days (~ 18 months) of initiating brolucizumab treatment. The median (IQR) follow-up time (i.e., from first to the last brolucizumab injection) for the subgroup with IOI-related AEs was 57 (30–126) days and 340 (89–586) days for the eyes without IOI-related AEs. Kaplan–Meier modelling of the real-world probability of brolucizumab-treated eyes experiencing an IOI-related AE after initiating brolucizumab treatment is shown in Supplementary Fig. S1.
Time from the Last Brolucizumab Injection to an IOI-Related AE
The median (IQR) time from the last brolucizumab injection to the development of the IOI-related AE was 13 (4–34) days (Supplementary Fig. S2). Approximately one-third of eyes [8/22 (36%)] developed the AE within 5 days of the brolucizumab injection.
Visual Outcomes Following AE Resolution/Stability
The IOI-related AEs fully resolved or stabilized in 20 of the 22 eyes (91%). One eye developed vasculitis that did not resolve and the other eye experienced anterior uveitis and vasculitis on the same day, and only the anterior uveitis had resolved at the end of the study period (292 days after the AE onset). The median (IQR) time to AE resolution/stability was 64 (42–130) days.
Eyes with IOI-related AEs lost a median (IQR) of –6.8 (–19.9, 0.0) letters in VA measured at the time of AE compared with their last VA measurement prior to the AE. The median (IQR) change in VA from the last VA prior to AE to 3 months after AE resolution/stability was 0.0 (–6.2, 3.3) letters (n = 21), and –4.8 (–6.2, 2.9) letters at 6 months after AE resolution/stability (n = 18). Taking the best VA at either 3 months or 6 months after AE resolution/stability, VA decreased by < 5 letters compared with the last VA measurement prior to the AE in 18 (82%) of the total 22 affected eyes (Fig. 2) and in 3 out of 4 of the eyes that developed IOI + RV (the AE resolved in the remaining eye at the last visit so no 3- or 6-month VA measurement is available).
VA at 3 months or 6 months (whichever is the higher VA of the two) after resolution/stability of an IOI-related AE compared with the last VA measurement prior to the AE. *AE unresolved at the last visit before the end of the study period, so no 3- or 6-month VA measurement was available for one eye. AE, adverse event; IOI, intraocular inflammation
Clinical Cases
Each IOI-related AE was managed on an individual basis depending on the patient and the nature and severity of the inflammation. Nevertheless, the majority of the 22 cases were mild to moderate and were treated successfully with topical corticosteroids (see Supplementary Table S2 for a breakdown of the treatments administered to the eyes with IOI-related AEs). The clinical management and outcomes of three cases are described in detail below, and these were selected to represent the variability of different inflammatory disease states. The first case was moderate in severity and developed vision loss that returned to pre-AE levels, the second case described is the severe adverse event with vision loss and the third is a case of mild IOI with stable VA throughout the event. The first and third cases also showed favorable changes in retinal morphology and choroidal vascularity after brolucizumab treatment initiation, as also observed by other authors [12]; however, this could not be ascertained in the second case due to the poor view of the retina.
Case 1: The patient was an 86-year-old female who had received 11 intravitreal anti-VEGF injections following nAMD diagnosis. Despite anti-VEGF treatment every 8 weeks (q8w), persistent nAMD and active CNV with worsening SRF was observed and the patient was switched to brolucizumab (Fig. 3A). VA at the time of switch was 51.9 letters. A total of four brolucizumab injections were given, initially at 4-week intervals, then extended to q8w, and SRF was resolving (Fig. 3B). At an unscheduled visit, 42 days after the fourth brolucizumab injection and 160 days after initiating brolucizumab, the patient presented with ocular pain and redness of 3 weeks duration. Two plus cells in the anterior chamber and vitreous, vascular sheathing, and cotton wool spots were all identified and indicative of RV, RO, and panuveitis, respectively. Cultures to rule out subacute endophthalmitis were negative. The patient was placed on topical antibiotics (ofloxacin) and steroids (Pred Forte), both four times daily, and a 25-gauge pars plana vitrectomy and vitreous biopsy were scheduled for 5 days later. Intraocular vancomycin and ceftazidime were administered at the time of surgery, and there were no resulting complications with clearing of vitreous debris and the patient subsequently improved over time (Fig. 3C-J). Antibiotic drops were tapered off over the following month and the nAMD was monitored with no further brolucizumab treatment. VA at the visit prior to the development of uveitis was 54.9 letters, which decreased to 35.0 letters during the AE, and VA at 3 and 6 months after AE resolution was 54.9 letters and 57.8 letters, respectively.
Images from case 1, an 86-year old female with AE occurring 160 days after initiating brolucizumab. A OCT image on the day of switch to brolucizumab, B OCT on the day of fourth and last brolucizumab injection, C, D OCT 1-day post-surgery, E–H OCT 1-week post-surgery, I OCT 6-weeks post-surgery, and J OCT 12-weeks post-surgery
Case 2: The second case was a 66-year-old male with a medical history of thyroid disease. He received 23 intravitreal anti-VEGF injections in the 26 months following nAMD diagnosis and was then switched to brolucizumab due to worsening nAMD and active CNV as seen by persistent edema and SRF (Supplementary Figs. S3A and S3B). When the patient returned for his follow-up visit 28 days after his first and only brolucizumab injection, he was found to have a profound loss of vision from 58.8 letters to hand motion. He denied pain, but complained of floaters and progressive loss of VA 2 weeks after the injection. Despite receiving and understanding the warning signs of IOI (including redness, increased light sensitivity, pain, floaters, and loss of vision), he did not call the office or come in sooner to be seen as he thought his vision would improve. At this visit, increased edema was seen and posterior uveitis was detected. No clear view of the posterior segment was possible during the slit lamp examamination due to media opacity. Vitreous findings noted were severe vitritis and vitreous debris, which heavily impacted the signal strength (0/10) and the quality of the optical coherence tomography (OCT) images (Supplementary Figs. S3C and S3D). Central macular thickness increased from 259 µm to 322 µm and most swelling was localized inferno-temporal to the macula. It was recommended that prompt pars plana vitrectomy be performed, but the patient was not able to get transportation. The posterior uveitis was therefore treated via intravitreal (Ozurdex injection) and oral (Medrol Dosepak) steroids with close monitoring and the AE resolved after 28 days. Once the vitritis cleared, there were no signs of RV or RO (Supplementary Figs. S3E and S3F). VA remained at 19.9 letters at both 3 and 6 months after AE resolution with no recurrence of IRF or SRF.
Case 3: This case was a 78-year-old female with a medical history of Crohn’s disease, hypertension, and type 2 diabetes. At the time of initiation of brolucizumab treatment, the patient had persistent SRF despite four previous anti-VEGF injections (Supplementary Fig. S4A) and VA was 53.9 letters. She received a total of two brolucizumab injections. SRF resolved after the first brolucizumab injection and VA increased to 57.8 letters, but pigment epithelial detachment persisted (Supplementary Fig. S4B). Eleven days after the second brolucizumab injection, the patient presented at an unscheduled clinic visit complaining of hazy vision and worsening floaters. She was diagnosed with posterior uveitis and trace vitreous cells were noted during a slit lamp examination. VA remained stable at 57.8 letters (Supplementary Fig. S4C). The IOI was treated with oral prednisone and trace vitreous cells resolved. The AE resolved completely after 98 days and VA at 3 and 6 months after recovery was 61.1 and 65.1 letters, respectively. The patient was switched back to the previous anti-VEGF on an 8-week dosing interval with a concomitant recurrence of SRF (Supplementary Figs. S3D and S3E).
Discussion
In this real-world study of a large cohort of patients with nAMD receiving at least one injection of brolucizumab, the overall incidence of IOI was 4.6%, IOI + RV was 0.8%, and IOI + RV + RO was 0.4%. There was a slight imbalance towards these events occurring in females, as has been noted in other real-world studies [13, 14]. Furthermore, there was an overall risk of 0.4% (2/482) of developing IOI + RV and 0.2% (1/482) of developing IOI + RV + RO and experiencing at least moderate vision loss (≥ 15 letters) at the time of event.
The Safety Review Committee review of the Phase 3 HAWK and HARRIER studies reported a rate of IOI in 4.6% (50/1088) of brolucizumab-treated eyes, and a rate of 3.3% (36/1088) for RV and 2.1% (23/1088) for RO [10]. The lower incidence of RV and RO in this real-world study may in part be due to the more flexible dosing schedule in the real world compared with HAWK and HARRIER, in which patient eyes were injected on a fixed 8- or 12-week dosing regimen, including if their retina was dry.
Since the safety signal was confirmed, evidence-based recommendations have been developed by different groups of ophthalmologists, recommending that monitoring and vigilance for signs of IOI throughout treatment should play a key role in the management of patients treated with brolucizumab [10,15,16,17,18,19,20,21,22]. This includes a thorough examination of the eye for inflammation prior to injection and instructing patients to report any change in vision or symptoms of IOI (including RV) and/or RO without delay, to ensure timely intervention [15,16,17,18,19,20,21,22]. In addition, if an IOI-related AE occurs, brolucizumab should be withdrawn and the AE addressed with prompt and intensive treatment as per standard of care [16, 18,19,20,21,22]. With this increased understanding of IOI-related AEs associated with brolucizumab use, real-world evidence has shown that long-term vision loss following an IOI-related AE may be limited [23,24,25]. In this real-world cohort, with appropriate management of the AEs, 3 (14%) eyes had ≥ 5-letter loss and 18 (82%) had < 5-letter loss within 6 months after AE resolution/stability compared with before the event.
Regarding the timing of the events, 83% of IOI-related AEs occurred in the initial 6 months of follow-up. In HAWK and HARRIER, approximately 74% of IOI-related AEs occurred within the initial 6 months after the first injection with brolucizumab [10]. Therefore, although patients should be monitored throughout treatment, the first months of therapy require particularly careful monitoring for such events.
A key strength of the study is that this is, to the best of our knowledge, the largest real-world safety study of eyes treated with at least one injection of brolucizumab, which reports on timing, management, and resolution of these events. The eyes also have differing lengths of treatment history prior to starting brolucizumab, which provides a very broad, heterogeneous study population that reflects real-world treatment conditions. A limitation is that the geographical range of the data is restricted as they are from a single practice network with 13 locations. In addition, by the nature of studying AEs, the number of patient eyes with an IOI-related AE (n = 22) is relatively small.
Conclusion
In summary, this real-world study demonstrates that with appropriate monitoring and management of IOI-related AEs, the incidence of RV and/or RO may be reduced and although not zero, vision loss may be limited.
References
Chakravarthy U, Havilio M, Syntosi A, et al. Impact of macular fluid volume fluctuations on visual acuity during anti-VEGF therapy in eyes with nAMD. Eye (Lond). 2021;35(11):2983–90.
Chakravarthy U, Pillai N, Syntosi A, et al. Association between visual acuity, lesion activity markers and retreatment decisions in neovascular age-related macular degeneration. Eye (Lond). 2020;34(12):2249–56.
Flaxel CJ, Adelman RA, Bailey ST, et al. Age-Related Macular Degeneration Preferred Practice Pattern®. Ophthalmology. 2020;127(1):1-P65.
Tietz J, Spohn G, Schmid G, et al. Affinity and potency of RTH258 (ESBA1008), a novel inhibitor of vascular endothelial growth factor a for the treatment of retinal disorders. Invest Ophthalmol Vis Sci. 2015;56(7):1501.
Beovu® [Summary of Product Characteristics], Basel, Switzerland, Novartis Pharma AG. Available at: www.ema.europa.eu/en/documents/product-information/beovu-epar-product-information_en.pdf. Accessed 3 April 2023.
Beovu® [Prescribing Information]. East Hanover, NJ: Novartis Pharmaceuticals Corp. Available at: https://www.novartis.us/sites/www.novartis.us/files/beovu.pdf . Accessed 3 April 2023.
Dugel PU, Koh A, Ogura Y, et al. HAWK and HARRIER: Phase 3, multicenter, randomized, double-masked trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology. 2020;127(1):72–84.
Dugel PU, Singh RP, Koh A, et al. HAWK and HARRIER: Ninety-six-week outcomes from the phase 3 trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology. 2021;128(1):89–99.
Safety of Beovu® (brolucizumab). Available at: https://www.brolucizumab.info/. Accessed 3 April 2023.
Monés J, Srivastava SK, Jaffe GJ, et al. Risk of inflammation, retinal vasculitis, and retinal occlusion-related events with brolucizumab: Post hoc review of HAWK and HARRIER. Ophthalmology. 2021;128(7):1050–9.
Gregori NZ, Feuer W, Rosenfeld PJ. Novel method for analyzing snellen visual acuity measurements. Retina. 2010;30(7):1046–50.
Viggiano P, Oliva Grassi M, Boscia G, et al. Short-term morphofunctional changes in previously treated neovascular AMD eyes switched to brolucizumab. J Clin Med. 2022;11(19):5517.
Khanani AM, Zarbin MA, Barakat MR, et al. Safety outcomes of brolucizumab in neovascular age-related macular degeneration: Results From the IRIS registry and Komodo Healthcare map. JAMA Ophthalmol. 2022;140(1):20–8.
Wykoff CC, Matsumoto H, Barakat MR, et al. Retinal vasculitis or vascular occlusion after brolucizumab for neovascular age-related macular degeneration: a systematic review of real-world evidence. Retina. 2023 Mar 8. Epub ahead of print. DOI: https://doi.org/10.1097/IAE.0000000000003769
Baumal CR, Spaide RF, Vajzovic L, et al. Retinal vasculitis and intraocular inflammation after intravitreal injection of brolucizumab. Ophthalmology. 2020;127(10):1345–59.
Baumal CR, Bodaghi B, Singer M, et al. Expert opinion on management of intraocular inflammation, retinal vasculitis, and vascular occlusion after brolucizumab treatment. Ophthalmol Retina. 2021;5(6):519–27.
Kilmartin D. Proposed best practice for Irish ophthalmologists: monitoring of patients following intra-vitreal brolucizumab therapy. Available at SSRN. 2021;3937320(2):1–18.
Holz FG, Heinz C, Wolf A, Hoerauf H, Pleyer U.Intraocular inflammation with brolucizumab use: Patient management-diagnosis-therapy. Ophthalmologe. 2021;118(3):248–56.
Pearce I, Amoaku W, Bailey C, et al. The changing landscape for the management of patients with neovascular AMD: Brolucizumab in clinical practice. Eye (Lond). 2022;36(9):1725–34.
Fonollosa A, Gallego-Pinazo R, Sararols L, Adán A, López-Gálvez M, Figueroa MS. Guidance on brolucizumab management recommendations. Arch Soc Esp Oftalmol (Engl Ed). 2022;S2173–5794(22):00084–6.
Sadda SR, Guymer R, Holz FG, et al. TThe importance of imaging to identify early signs of intraocular inflammation: Expert opinion for brolucizumab. Ophthalmologica. 2022;245(6):588–91.
Holz FG, Iida T, Maruko I, Sadda SR. A consensus on risk mitigation for brolucizumab in neovascular age-related macular degeneration: Patient selection, evaluation, and treatment. Retina. 2022;42(9):1629–37.
Kurup SK, Tabbaa T, Echegaray JJ, Oliver AL. Intraocular inflammation secondary to intravitreal brolucizumab treated successfully with sub-tenon triamcinolone: A case report. Am J Ophthalmol Case Rep. 2022;25: 101289.
Kataoka K, Horiguchi E, Kawano K, et al. Three cases of brolucizumab-associated retinal vasculitis treated with systemic and local steroid therapy. Jpn J Ophthalmol. 2021;65(2):199–207.
Haensli C, Pfister IB, Garweg JG. Switching to brolucizumab in neovascular age-related macular degeneration incompletely responsive to ranibizumab or aflibercept: Real-life 6 month outcomes. J Clin Med. 2021;10(12):2666.
Acknowledgements
The authors wish to thank Dr Arnold F. Nothnagel from Retina Associates of Cleveland Inc. for providing information on clinical cases. Support was also provided by Lujia Zhou and Zheng Si (KMK Consulting, Morristown, NJ, USA) for QC programming.
Funding
Financial support was provided by Novartis Pharma AG (Basel, Switzerland). The sponsor or funding organization participated in the design of the study, management, analysis, and interpretation of the data, preparation, review, and approval of the manuscript, and funded the journal’s rapid service fee.
Medical Writing and Editorial Assistance
Medical writing support was provided by Susan Simpson, PhD (Novartis Ireland Ltd.), in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3). The funding for this writing support was provided by Novartis Pharma AG.
Author Contributions
Ryan Zubricky, Jasmyne McCoy, Richard Donkor, David G. Miller, and Joseph M. Coney were involved in data capture and Nina Sonbolian, Andrew Heaney, Ver Bilano, and Helene Karcher were involved in data analyses. All authors made substantial contributions to the study design, interpretation of data, drafting the article, and revising it critically, and final approval of the version to be submitted.
Prior Presentation
These data have been presented at The Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting, April 23–27, 2023, New Orleans, LA, USA.
Disclosures
Nina Sonbolian, Andrew Heaney, Ver Bilano, and Helene Karcher are Novartis employees and Helene Karcher is a Novartis shareholder. David G. Miller reports consultancy fees and Speakers’ Bureau honoraria from Regeneron Pharmaceuticals. Joseph M. Coney has received grants from Alimera Sciences, Allergan/Abbvie, Apellis, Genentech, MacTel, National Eye Institute, Novartis, Regeneron, and RegenexBio, consulting fees from Alimera Sciences, Apellis, and RegenexBio, and honoraria from Alimera Sciences, Allergan/Abbvie, Apellis, Genentech, Novartis, Regeneron, and RegenexBio.
Compliance with Ethics Guidelines
Patients provided consent to have their deidentified data used for research purposes. This study complied with the tenets of the Declaration of Helsinki and is based on a retrospective analysis of deidentified data obtained as part of routine clinical practice. All patient data were collected in accordance with the Health Insurance Portability and Accountability Act (https://www.cdc.gov/phlp/publications/topic/hipaa.html). As this study constituted a secondary analyses on fully anonymized data, institutional review board or additional informed consent was not required in line with the Code of Federal Regulations Code 46.104 (d) (1) (2) (i).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zubricky, R., McCoy, J., Donkor, R. et al. Real-World Frequency and Management of Ocular Adverse Events in Eyes with Neovascular Age-Related Macular Degeneration Treated with Brolucizumab. Ophthalmol Ther 12, 2397–2408 (2023). https://doi.org/10.1007/s40123-023-00741-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00741-w