Abstract
Introduction
The aim of this work is to investigate the differences in the measurement of foveal retinal thickness in myopic patients between two display modes (1:1 pixel and 1:1 micron) on optical coherence tomography (OCT).
Methods
Horizontal OCT line scan through the central fovea was used for manual measurement of foveal retinal thickness under the two display modes, and the values were compared using Wilcoxon signed-rank test. Correlations between the OCT image tilting angle (OCT ITA) and differences in OCT measurement were analyzed by Spearman’s test.
Results
127 participants with a median age of 28 years, a median spherical equivalent (SE) of − 8.5 D, and a median axial length (AL) of 27.04 mm. There were significant differences between the two display modes, with a median absolute difference (median relative difference) of 13.33 μm (2.75%) for the central foveal thickness (CFT), 5.33 μm (1.28%) for the Henle fiber and outer nuclear layer thickness (HFL + ONL), 3 μm (6.47%) for the external limiting membrane to ellipsoid zone distance (ELM-EZ), and 4 μm (8.77%) for the ellipsoid zone to retinal pigment epithelium distance (EZ-RPE) (all p < 0.05). The differences in foveal retinal thickness between the two display modes were significantly correlated with the OCT ITA (r = 0.732 for CFT, 0.561 for HFL + ONL, 0.642 for ELM-EZ, and 0.471 for EZ-RPE, all p < 0.05).
Conclusions
Disparities between the two display modes were found in the manual measurement of foveal retinal thickness and correlated to the OCT ITA.
Similar content being viewed by others
Previous studies investigated the differences between the display modes in choroidal thickness measurement and found differences between the measurements in the two display modes, but did not state the exact reason for the differences. |
The current study found that the retinal foveal thickness measurement is different in the two display modes, especially when the OCT B scan image is tilted, and these differences are correlated with the OCT B scan image tilting angle. Furthermore, we provided regression equations to correct the differences. |
Despite the previous attainments, one concern is that there is no agreement on whether to use 1:1 pixel display mode or 1:1 micron display mode for thickness measurement. Our research provided regression equations according to the tilting angle to correct the differences in the two display modes. The equations can be used to convert the retinal thickness between the two display modes. |
Introduction
Spectral-domain optical coherence tomography (SD-OCT) is a non-invasive imaging technique widely used to evaluate the microanatomical structures of the retina and for the detection and monitoring of retinal diseases [1,2,3,4]. The advent of SD-OCT has improved macular image quality by allowing a high-density sampling resolution while simultaneously increasing testing reliability and repeatability [5,6,7,8]. SD-OCT also provides helpful clinical information and allows clinicians to obtain cross-sectional quantitative macular thickness measurements for the early diagnosis and follow-up assessment of macular pathologies such as myopic retinoschisis, epiretinal membrane, and macular edema, macular hole, macular degeneration, and central serous retinopathy [9,10,11,12]. The manual measurement of retinal foveal thickness based on SD-OCT has been widely used to investigate characteristics of retinal structure [2, 6, 13]. Additionally, average thickness and volume can be determined for predefined portions of each retinal layer in the SD-OCT image [14].
It is noticeable that there are two display modes of OCT images (1:1 pixel display mode and 1:1 micron display mode). The 1:1 pixel mode is the most commonly used display mode for OCT images. The OCT machine uses the pixels between two points to measure the distance. In the 1:1 pixel mode, the ratio between vertical and horizontal scales is 3.775, and in 1:1 micron mode, the scale ratio is 1:1. When the OCT B-scan image is well horizontal, there would be no difference in values of the manually measured central foveal thickness (CFT) between the two display modes. However, when the OCT image is tilted, in theory, the CFT values in 1:1 pixel mode would be higher than those in the 1:1 micron mode.
Although the 1:1 pixel mode is commonly used in clinical practice, one concern is that no previous study has mentioned whether 1:1 pixel image is different from 1:1 micron image used for manual measurement of the retinal foveal thickness, especially when the OCT B-scan image is tilted. It is useful to consider the differences between the display modes of OCT to avoid measurement errors and misinterpretations and to plan for the most appropriate management of retinal diseases [10, 15,16,17].
The purpose of this study was to evaluate the differences in manual measurements of CFT based on 1:1 pixel images and 1:1 micron images in myopic patients. Furthermore, we investigated possible reasons for the difference in the two measurement display modes.
Methods
Participants
This was a retrospective, cross-sectional study performed on myopic patients at Guangzhou Aier Institute of Eye Refractive Surgery (GZAIER). The research was approved by the Institutional Review Board (IRB) of GZAIER and followed the Helsinki Declaration. Additionally, the same IRB waived the necessity for informed consent because the study only involved examining medical records and no specific patient could be identified from the data. All the patients underwent comprehensive baseline ophthalmologic examinations including refraction, best-corrected visual acuity with a decimal chart, slit-lamp biomicroscope examination of the anterior segment and the fundus, intraocular pressure, and axial length measurement, pachymetry, and SD-OCT scanning. Our study included individuals between 18 and 45 years of age, who visited GZAIER for refractive surgery, and underwent OCT imaging.
We excluded myopic eyes with concurrent ophthalmic disorders such as corneal disease, keratoconus, ocular trauma or ophthalmic surgery, uveitis, glaucoma, and patients younger than 18 years, patients with retinoschisis, choroidal neovascularization, and patients with macular hemorrhage.
Imaging
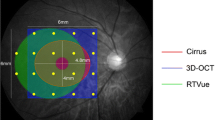
All eyes, after accomplishing satisfactory pupillary dilation with 0.5% tropicamide (SANTEN PHARMACEUTICAL CO, LTD.SHIGA PLANT), underwent SD-OCT scanning. The subjects were instructed to look at the fixation light in the machine, and the foveolar fixation was confirmed by observing the retinal image through the infrared monitoring camera. A high-resolution horizontal B-scan through the central fovea was performed for each eye, using SD-OCT (Spectralis, Heidelberg Engineering GmbH, Heidelberg, Germany). For each patient, an OCT image of the right eye image was used for manual measurement, and a left eye image was used if the right eye image was not available. OCT images were measured three times by an experienced technician (YG), and the average values were used for analysis. All the measurements were conducted for both display modes; i.e., 1:1 pixel mode and 1: 1 micron mode. The computer-based caliper measurement tool in the SD-OCT was used to manually measure different retinal layers in the two display modes (Fig. 1). ImageJ software (US National Institutes of Health, Bethesda, MD, USA. https://imagej.net/software/fiji/) was used to assess the OCT image tilting angle (OCT ITA).
Retinal bands/layers/zones as visualized by spectral-domain optical coherence tomography. The thickness of the Henle fiber layer and the outer nuclear layer (HFL + ONL) is measured as the distance between the inner limiting membrane and the inner border of the external limiting membrane (ELM) band. ELM–ellipsoid zone (EZ) thickness is the distance between the inner border of the ELM band and the outer border of the EZ. EZ–retinal pigment epithelium (RPE) thickness is the distance between the outer border of the EZ and the inner border of the RPE
The CFT is defined as the distance between the surface of the internal limiting membrane (ILM) and the outer border of the retinal pigment epithelium (RPE) at the central fovea. The distance between the inner border of the ILM (at the steepest section of the foveal excavation) and the inner border of the external limiting membrane (ELM) line in conjunction with the highest part of the foveal bulge was described as the HFL + ONL thickness. The distance between the inner border of the ELM line and the outer border of the ellipsoid zone (EZ) was defined as the ELM–EZ distance; the distance between the outer border of the EZ and the inner border of RPE layer was defined as the EZ-RPE distance (Fig. 2) [18]. For the measurement of the OCT ITA, we first drew a line tangent to the RPE line below the foveola. The angle alpha between this line and the bottom edge of the OCT image was defined as the OCT ITA (Fig. 3). It is noticeable that all the retinal thicknesses measured in the study are the “apparent thicknesses” based on the previous assumptions of the corresponding OCT layers to the histological slides [19, 20].
Representative optical coherence tomography images of the same eye showing the manual measurement of the central foveal thickness (CFT) under the two display modes (A CFT manual measurement in 1:1 pixel mode, B CFT manual measurement in 1:1 micron display mode). In the 1:1 pixel mode, the ratio between vertical and horizontal scales is 3.775, and in 1:1 micron mode, the scale ratio is 1:1 (arrowhead)
Statistical Analysis
The data are presented as median and interquartile range (IQR). All statistical analyses were performed using the SPSS 20.0 (SPSS. Inc., Chicago, IL, USA). Normality of the data was evaluated by Shapiro–Wilk test. The OCT measurement in the two display modes was compared using the Wilcoxon signed-rank test. The absolute difference in retinal thickness was calculated by retinal thickness in 1:1 pixel mode minus retinal thickness in 1:1 micron mode, and the relative difference in retinal thickness was defined as absolute difference divided by the retinal thickness in 1:1 micron mode. Spearman correlation tests and linear regressions were used to assess the correlations between the OCT ITA and the differences in OCT measurement under the two display modes. For all the tests, p < 0.05 was considered statistically significant.
Results
The baseline demographic characteristics of the eyes are shown in Table 1. We recruited a total of 127 participants with a median age of 28 years (interquartile range (IQR): 9 years), a median spherical equivalent (SE) of − 8.5D (IQR: − 6.62 D), and a median axial length (AL) of 27.04 mm (IQR: 3.42 mm).
The evaluation of the differences between the display modes is shown in Table 2. There were statistically significant differences between the two display modes in the measurement of retinal thickness, with the median (IQR) absolute difference and median (IQR) relative difference of 13.33 μm (22 μm) and 2.75% (15.39%) for CFT, 5.33 μm (11.33 μm) and 1.28% (19.39%) for HFL + ONL thickness, 3 μm (4.66 μm) and 6.47% (21.89%) for ELM-EZ distance, and 4 μm (2.67 μm) and 8.77% (26.74%) for EZ-RPE distance (all p < 0.05).
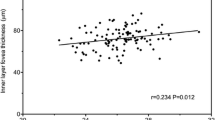
The correlations between the differences in the two display modes and the OCT ITA are shown in Tables 3 and 4. The absolute differences in OCT measurement were significantly correlated with the OCT ITA, with a correlation coefficient of 0.734 for CFT, 0.570 for HFL + ONL, 0.650 for ELM-EZ, and 0.487 for EZ-RPE and the relative differences correlated to the OCT ITA with a correlation coefficient of 0.732 for CFT, 0.561 for HFL + ONL, 0.642 for ELM-EZ, and 0.471 for EZ-RPE (all p < 0.05). Linear regressions of the OCT ITA and the differences in retinal thickness between the two display modes are shown in Figs. 4 and 5 along with the regression equations.
Discussion
OCT is a standard ophthalmologist's tool for diagnosing and managing retinal pathologies [21,22,23]. Imaging of the retina has substantially advanced since the development of SD-OCT. Recent studies demonstrated SD-OCT retinal thickness measurements and some inaccuracies in SD-OCT retinal thickness measurements [6, 21, 24,25,26,27,28,29]. In pathologies where the OCT B-scan image is distorted, automated segmentation may produce inaccurate results due to segmentation errors. In such cases, manual measurements and/or manual correction of segmentation errors may provide more accuracy, which is essential in understanding the pathophysiology of numerous ocular diseases [14]. Subsequently in this study, we measured manually the CFT using the two OCT display modes, which revealed significant differences in retinal thickness measurements based on 1:1 pixel display mode compared to the measurements based on 1:1 micron display mode. Moreover, we found that the differences between the two display modes are correlated to the OCT ITA. The current study shows a significant difference in the measurement of CFT, HFL + ONL thickness, ELM-EZ distance, and EZ-RPE under the two OCT display modes. We found that there is an overestimation of CFT measurement in the 1:1 pixel mode when the OCT image is tilted. It is beneficial to consider the differences between OCT display modes to avoid measurement errors and misinterpretations and to plan for the best management of retinal diseases. In their study, Kim et al. also found differences between the two display modes for choroidal thickness measurement and they found that the subfoveal choroidal thickness (SFCT) was greater in measurements based on the 1:1 pixel mode. A critical overestimation of the SFCT was noted when it was measured on a 1:1 pixel mode. This finding suggested that the estimation of choroidal thickness should be performed based on a 1:1 µm display mode, particularly if the estimation line is not vertical. In addition, as demonstrated in some eyes for foveal retinal thickness, they believed that a similar measurement error can occur when measuring the thickness of other structures when the image of the structure is tilted, which is exactly the case in our current study. In their study, approximately 30% of the images with the 1:1 pixel setting showed a tilted view of the retina/choroid. Their study did not elucidate the exact reason for the tilted images, but suspected the curvature of the eye, especially in case of myopia, poor fixation, head tilt, or tilt OCT camera [30].
In their study, Cho et al. show that 1:1 µm images granted slightly better repeatability in interobserver measurements, and suggested that choroidal thickness measurements must be interpreted with caution, especially for a thick choroid. In their study for both image modes, the SFCT does not significantly vary between the observers (p = 0.5663 for the 1:1 pixel image and p = 0.2839 for the 1:1 micron image, respectively). The mean SFCT was 315.3 ± 89.2 mm in the 1:1 pixel images and 312.6 ± 88.4 mm in the 1:1 micron images based on the two observers’ initial measurements. However, in their study, statistical analysis of the 1:1 pixel images revealed significantly stronger repeatability than the 1:1 micron images [31]. Although Kim et al. showed overestimation in the 1:1 pixel images, these inaccuracies did not appear to have a substantial impact on reproducibility [30]. We realized that the differences between the two display modes in our study are statically more significant than the differences in their studies. This can be explained by the differentiation of the technique of measurement without considering the OCT ITA and also the measured parameters. Marcel et al. performed a study on the reproducibility of retinal thickness measurements in healthy subjects using Spectralis optical coherence tomography system. Their study shows a high reproducibility in the retinal thickness measurement for all the Early Treatment Diabetic Retinopathy Study areas. In their study, the mean foveal thickness is 286 ± 17 µm in the micron display mode in contrast, in our study the mean CFT is 213.33 μm (22.33 μm) in the 1:1 µm mode [6]. This difference can probably be explained by the differences in the study population (emmetropes vs. myopes), the technique of measurement (automatic vs. manual), and the model of OCT machine used (frequency-domain vs. spectral-domain). Previous studies have shown that retinal thickness may be affected by refractive status [32, 33], measurement technique [34], and OCT machine model [35,36,37].
Despite the reproducibility between the two display modes, previous studies mainly used 1:1 pixel display mode. Although 1:1 pixel display mode shows all acquired pixels, 1:1 micron display mode organizes the pixels using the same scale horizontally and vertically. As a result, to reflect the physical dimensions, the 1:1 micron display mode must be vertically compressed approximately threefold. Even though the 1:1 pixel display mode can more clearly show a precise structural change, a slight deviation from the perpendicular measuring can lead to a large error during manual measurement [31]. However, there is no consensus on whether to use a 1:1 pixel display mode or a 1:1 micron display mode for manual retinal thickness measurement. As a result, the type of image used for measuring CFT is at the discretion of each investigator the same as for CT manual measurement. In some previous studies, measurements were based on 1:1 pixel display mode [38,39,40,41,42,43,44], whereas others used 1:1 micron display mode [45,46,47,48].
Since there is no agreement on whether to use 1:1 pixel display mode or 1:1 micron display mode for thickness measurement, methods to convert the values between different display modes are warranted. Our research found correlations between the differences in retinal thickness and the OCT ITA. We found that the more the OCT B-scan image was tilted, the more differences in retinal thickness were observed. This finding may be due to different vertical-to-horizontal scale ratios in the two display modes. As the ITA is increased, the CFT is more over-estimated by the 1:1 pixel mode because the ratio is 3.775 in this mode while it is 1 in the 1:1 micron mode. We then provided equations produced by the regression models to calculate the differences between the two display modes according to the OCT ITA on the B-scan image. Further studies are needed to validate the reliability of these equations, and before that they should be applied with caution.
The differences in retinal thickness between the two display modes were correlated with the OCT ITA, but not with SE or AL. Such differences could also be affected by the angle kappa and shape of the posterior pole, since both can affect the horizontality of the OCT B-scans. Therefore, in any case, where the OCT B-scan image is tilted, the difference in retinal thickness measurement should be considered. The limitation of the current study is that it only describes the differences at a single center and in myopic patients, and the retinal thickness was only measured at the central fovea. Whether our findings can be generalized to other patients (hyperopes or emmetropes) and other retinal locations needs to be validated.
Conclusions
Our study found that retinal thickness measurements in myopic patients under the two display modes were different, and the differences were correlated with OCT ITA. Using regression equations, we could correct the differences between the two display modes.
References
Wang KL, et al. Understanding the variability of handheld spectral-domain optical coherence tomography measurements in supine infants. PLoS ONE. 2019;14(12): e0225960.
Mahmoudzadeh R, et al. Agreement of optical coherence tomography thickness measurements between Heidelberg Eye Explorer and ImageJ software. Can J Ophthalmol. 2022;57(5):344–49.
Choovuthayakorn J, et al. Spectral-domain optical coherence tomography of macula in myopia. Int Ophthalmol. 2016;36(3):319–25.
Inoue M, et al. Long-term results of intravitreal ranibizumab for the treatment of retinal angiomatous proliferation and utility of an advanced RPE analysis performed using spectral-domain optical coherence tomography. Br J Ophthalmol. 2014;98(7):956–60.
Kiernan DF, Mieler WF, Hariprasad SM. Variety, variability and veracity: macular thickness and reproducibility among optical coherence tomography systems. Am J Ophthalmol. 2010;150(2):138-140.e2.
Menke MN, et al. Reproducibility of retinal thickness measurements in healthy subjects using Spectralis optical coherence tomography. Am J Ophthalmol. 2009;147(3):467–72.
Domalpally A, et al. Repeatability of retinal thickness measurements between spectral-domain and time-domain optical coherence tomography images in macular disease. Ophthalmic Surg Lasers Imaging. 2010;41(Suppl):S34-41.
Hanumunthadu D, et al. Spectral-domain optical coherence tomography retinal and choroidal thickness metric repeatability in age-related macular degeneration. Am J Ophthalmol. 2016;166:154–61.
Wakitani Y, et al. Macular thickness measurements in healthy subjects with different axial lengths using optical coherence tomography. Retina. 2003;23(2):177–82.
Lim MC, et al. Use of optical coherence tomography to assess variations in macular retinal thickness in myopia. Invest Ophthalmol Vis Sci. 2005;46(3):974–8.
Wong BM, et al. Validation of optical coherence tomography retinal segmentation in neurodegenerative disease. Transl Vis Sci Technol. 2019;8(5):6–6.
Giammaria D, et al. A new method to assess foveal morphology with optical coherence tomography. Clin Ter. 2019;170(3):e192–8.
Al-Badawi AH, et al. Efficacy of non-fovea-sparing ILM peeling for symptomatic myopic foveoschisis with and without macular hole. Br J Ophthalmol. 2019;103(2):257–63.
Govetto A, et al. Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol. 2017;175:99–113.
Kim H, et al. Optical coherence tomography measurement and visual outcome in acute central retinal artery occlusion. Korean J Ophthalmol. 2018;32(4):303–11.
Song AP, et al. Measurement of retinal thickness in macular region of high myopic eyes using spectral domain OCT. Int J Ophthalmol. 2014;7(1):122–7.
Takahashi H, et al. Ultra-widefield optical coherence tomographic imaging of posterior vitreous in eyes with high myopia. Am J Ophthalmol. 2019;206:102–12.
dell’Omo R, et al. Restoration of foveal thickness and architecture after macula-off retinal detachment repair. Invest Ophthalmol Vis Sci. 2015;56(2):1040–50.
Poornachandra B, et al. Quantifying microstructural changes in retinitis pigmentosa using spectral domain—optical coherence tomography. Eye Vis (Lond). 2019;6:13.
Alvarez-Guzman C, et al. The impact of central foveal thickness and integrity of the outer retinal layers in the visual outcome of uveitic macular edema. Int J Retina Vitreous. 2021;7(1):36.
Sadda SR, et al. Errors in retinal thickness measurements obtained by optical coherence tomography. Ophthalmology. 2006;113(2):285–93.
Trichonas G, Kaiser PK. Optical coherence tomography imaging of macular oedema. Br J Ophthalmol. 2014;98(Suppl 2):ii24–9.
Mitsch C, et al. Systematic ultrastructural comparison of swept-source and full-depth spectral domain optical coherence tomography imaging of diabetic macular oedema. Br J Ophthalmol. 2020;104(6):868–73.
Chhablani J, et al. Influence of scanning density on macular choroidal volume measurement using spectral-domain optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2013;251(5):1303–9.
Cai S, Therattil A, Vajzovic L. Optical coherence tomography imaging of the pediatric retina. J AAPOS. 2020;24(5):261–7.
Gella L, Raman R, Sharma T. Macular thickness measurements using Copernicus spectral domain optical coherence tomography. Saudi J Ophthalmol. 2015;29(2):121–5.
Al-Zamil WM, Al-Zwaidi FM, Yassin SA. Macular thickness in healthy Saudi adults. A spectral-domain optical coherence tomography study. Saudi Med J. 2017;38(1):63–9.
Ghazi NG, et al. Quantification of error in optical coherence tomography central macular thickness measurement in wet age-related macular degeneration. Am J Ophthalmol. 2009;148(1):90-6.e2.
Ray R, Stinnett SS, Jaffe GJ. Evaluation of image artifact produced by optical coherence tomography of retinal pathology. Am J Ophthalmol. 2005;139(1):18–29.
Kim JH, et al. Overestimation of subfoveal choroidal thickness by measurement based on horizontally compressed optical coherence tomography images. Graefes Arch Clin Exp Ophthalmol. 2013;251(4):1091–6.
Cho AR, Choi YJ, Kim YT. Influence of choroidal thickness on subfoveal choroidal thickness measurement repeatability using enhanced depth imaging optical coherence tomography. Eye (Lond). 2014;28(10):1151–60.
Cheng SC, Lam CS, Yap MK. Retinal thickness in myopic and non-myopic eyes. Ophthalmic Physiol Opt. 2010;30(6):776–84.
Ismael ZF, et al. Relationship between functional and structural retinal changes in myopic eyes. Clin Exp Optom. 2017;100(6):695–703.
Yoon YS, et al. Comparison of retinal layer thickness measurements obtained using two different swept-source optical coherence tomography imaging modes. Int Ophthalmol. 2020;40(5):1111–21.
Sull AC, et al. Comparison of spectral/Fourier domain optical coherence tomography instruments for assessment of normal macular thickness. Retina. 2010;30(2):235–45.
Ho J, et al. Assessment of artifacts and reproducibility across spectral- and time-domain optical coherence tomography devices. Ophthalmology. 2009;116(10):1960–70.
Sayanagi K, et al. Comparison of spectral-domain versus time-domain optical coherence tomography in management of age-related macular degeneration with ranibizumab. Ophthalmology. 2009;116(5):947–55.
Chung SE, et al. Choroidal thickness in polypoidal choroidal vasculopathy and exudative age-related macular degeneration. Ophthalmology. 2011;118(5):840–5.
Koizumi H, et al. Subfoveal choroidal thickness in typical age-related macular degeneration and polypoidal choroidal vasculopathy. Graefes Arch Clin Exp Ophthalmol. 2011;249(8):1123–8.
Kim SW, et al. Comparison of choroidal thickness among patients with healthy eyes, early age-related maculopathy, neovascular age-related macular degeneration, central serous chorioretinopathy, and polypoidal choroidal vasculopathy. Retina. 2011;31(9):1904–11.
Manjunath V, et al. Analysis of choroidal thickness in age-related macular degeneration using spectral-domain optical coherence tomography. Am J Ophthalmol. 2011;152(4):663–8.
Maruko I, et al. Subfoveal choroidal thickness after treatment of central serous chorioretinopathy. Ophthalmology. 2010;117(9):1792–9.
Maruko I, et al. Subfoveal retinal and choroidal thickness after verteporfin photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2011;151(4):594-603.e1.
Branchini L, et al. Reproducibility of choroidal thickness measurements across three spectral domain optical coherence tomography systems. Ophthalmology. 2012;119(1):119–23.
Margolis R, Spaide RF. A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol. 2009;147(5):811–5.
Imamura Y, et al. Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Retina. 2009;29(10):1469–73.
Tan CS, et al. Diurnal variation of choroidal thickness in normal, healthy subjects measured by spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53(1):261–6.
Querques G, et al. Choroidal changes associated with reticular pseudodrusen. Invest Ophthalmol Vis Sci. 2012;53(3):1258–63.
Acknowledgements
Funding
This work was supported by the National Natural Science Foundation of China (81870663 and 82171075), the Science and Technology Program of Guangzhou (20220610092), the Outstanding Young Talent Trainee Program of Guangdong Provincial People’s Hospital (KJ012019087), the GDPH Scientific Research Funds for Leading Medical Talents and Distinguished Young Scholars in Guangdong Province (KJ012019457), the Talent Introduction Fund of Guangdong Provincial People’s Hospital (Y012018145), the launch fund of Guangdong Provincial People’s Hospital for NSFC (8217040546), the Medical Scientific Research Foundation of Guangdong Province, China (A2021378). The sponsors or funding organizations had no role in the design or conduct of this research. The journal’s Rapid Service Fee was funded by the authors.
Author Contributions
Xiaohong Yang, Honghua Yu, and Yijun Hu contributed to the conception and design of the study. Dan Jouma Amadou Maman Lawali, Yunxiang Guo, and Ying Fang performed data collection and Yunxiang Guo performed OCT measurements. Dan Jouma Amadou Maman Lawali and Guanrong Wu performed the statical analysis. Dan Jouma Amadou Maman Lawali, Zhangjie Lin, and Abdou Amza interpreted the results and co-wrote the manuscript. All authors contributed to the drafting and revision of the manuscript, and final approval of the manuscript.
Disclosures
Dan Jouma Amadou Maman Lawali, Guanrong Wu, Yunxiang Guo, Zhangjie Lin, Qiaowei Wu, Abdou Amza, Zijing Du, Yun Ren, Ying Fang, Xinran Dong, Yunyan Hu, Yongyi Niu, Hongyang Zhang, Honghua Yu, Xiaohong Yang, and Yijun Hu have nothing to disclose.
Compliance with Ethics Guidelines
The research was approved by the Institutional Review Board of Guangzhou Aier Institute of Eye Refractive Surgery (GZAIER2019IRB20) and followed the Helsinki Declaration.
Data Availability
The data used during the current study are available from the corresponding authors on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lawali, D.J.A.M., Wu, G., Guo, Y. et al. Measurement of Foveal Retinal Thickness in Myopic Patients Using Different Display Modes on Optical Coherence Tomography: A Retrospective, Cross-Sectional Study. Ophthalmol Ther 12, 167–178 (2023). https://doi.org/10.1007/s40123-022-00584-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00584-x