Abstract
Introduction
Tanezumab is a monoclonal antibody against nerve growth factor that is under investigation for the treatment of osteoarthritis (OA) pain. We conducted subgroup analyses of two randomized phase 3 studies to summarize efficacy, general safety, and adjudicated joint safety of tanezumab in Japanese patients with moderate-to-severe OA.
Methods
In Study 1 (NCT02528188), patients received subcutaneous tanezumab 2.5 mg or 5 mg every 8 weeks or daily oral nonsteroidal anti-inflammatory drugs (NSAID) for 56 weeks. The co-primary efficacy endpoints were change from baseline in the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Pain subscale score and WOMAC Physical Function subscale score at Week 16 (overall study and Japan-specific endpoints) as well as Patient Global Assessment (PGA)-OA score at Week 16 (overall study endpoint only). In Study 2 (NCT02709486), patients received subcutaneous tanezumab 2.5 mg, 5 mg, or placebo every 8 weeks for 24 weeks. Safety monitoring included adjudicated composite joint safety endpoint (CJSE) including rapidly progressive osteoarthritis type 1 (RPOA1), RPOA2, primary osteonecrosis, pathological fracture, or subchondral insufficiency fracture.
Results
For Study 1, Japanese patients (n = 200) treated with tanezumab 2.5 mg and 5 mg showed numerically greater improvements in WOMAC Pain, WOMAC Physical Function, and PGA-OA scores versus NSAID at Week 16. Incidences of treatment-emergent adverse events were generally similar between tanezumab 2.5 mg, 5 mg, and NSAID groups. In the integrated safety analysis (Studies 1 + 2; n = 306), ten patients were adjudicated to have a component of CJSE: RPOA1 [tanezumab 2.5 mg (n = 2), tanezumab 5 mg (n = 5)], RPOA2 [tanezumab 2.5 mg (n = 1), tanezumab 5 mg (n = 1)], or primary osteonecrosis [tanezumab 2.5 mg (n = 1)]. Time-adjusted adjudicated rates of RPOA1 and RPOA2 were higher with tanezumab than NSAID or placebo and increased with dose of tanezumab.
Conclusion
Observations from the Japanese subgroup were generally consistent with the overall study populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Tanezumab is a monoclonal antibody against nerve growth factor that is under investigation for the treatment of osteoarthritis (OA) pain. |
Tanezumab has demonstrated efficacy in OA clinical studies in both international and Japanese populations, but association of tanezumab treatment and an increase in rapidly progressive osteoarthritis (RPOA) has been reported in early trials. |
We conducted a subgroup analysis of two randomized phase 3 OA clinical studies to summarize the efficacy, overall safety, and adjudicated joint safety of tanezumab in Japanese patients with moderate-to-severe OA. |
What was learned from the study? |
In Japanese patients with moderate-to-severe OA, tanezumab showed numerically greater improvements in the Western Ontario and McMaster Universities Osteoarthritis Index Pain and Physical Function scores and in the Patient’s Global Assessment of OA at Week 16 versus nonsteroidal anti-inflammatory drug (NSAID); incidence of treatment-emergent adverse events was generally similar among tanezumab 2.5 mg, 5 mg, and NSAID groups; and adjudicated composite joint safety endpoint rates (time-adjusted) were higher with tanezumab than NSAID or placebo and increased with dose. |
Observations from the Japanese subgroup were generally consistent with the overall study populations. |
Introduction
Osteoarthritis (OA) is a common condition in Japan, with the incidence of radiographic knee and hip OA estimated at 61.9% and 15.7%, respectively, and the rate of symptomatic OA approximately 30% [1, 2]. The Japanese Orthopaedic Association guidelines for OA are based on those from the Osteoarthritis Research Society International and recommend nonsteroidal anti-inflammatory drugs (NSAIDs) and intra-articular injection of steroid and hyaluronate as first-line pharmacological treatments [3]. In a Japanese real-world study that reviewed hospital claims data, NSAIDs were the mainstay of OA treatment in Japan, with prescriptions for NSAIDs reported in 92% of Japanese patients with OA [4]. However, NSAID use is associated with an increased risk of gastrointestinal complications, cardiovascular events, and acute or chronic kidney injury [5,6,7,8,9]. Therefore, there is an unmet need for treatments that are safe and effective in pain management for patients with OA in Japan.
Tanezumab is a monoclonal antibody against nerve growth factor under investigation for the treatment of OA pain in patients who have not had an adequate response to or who cannot tolerate standard analgesics (i.e., NSAIDs, acetaminophen, tramadol, or opioids). It has demonstrated efficacy in patients with OA in both international and Japanese populations [10,11,12,13,14]. Some early clinical trials of tanezumab reported cases of rapidly progressive osteoarthritis (RPOA) [15]. Due to joint safety concerns in clinical studies and changes in the sympathetic nervous system observed in preclinical animal studies [15, 16], the US Food and Drug Administration placed partial clinical holds on studies of nerve growth factor antibodies, both of which were subsequently lifted following investigation. The tanezumab safety profile in patients with OA has been further evaluated in studies conducted since the partial clinical holds were lifted.
To determine whether the efficacy and safety of tanezumab for Japanese patients with OA are consistent with or similar to the overall population in the clinical trials, we conducted a subgroup analysis of two randomized phase 3 studies [13, 14]. These studies summarized the efficacy, overall safety, and adjudicated joint safety of tanezumab in Japanese patients with moderate-to-severe OA.
On October 26, 2021, Pfizer Inc. and Eli Lilly and Company announced discontinuation of the tanezumab global clinical development program as a result of the outcomes of regulatory reviews of tanezumab for the treatment of osteoarthritis pain by the US Food and Drug Administration and European Medicines Agency [17, 18].
Methods
Data Sources
Data were summarized from a phase 3, randomized, double-blind, multicenter, active-controlled (NSAID), parallel-group study (ClinicalTrials.gov: NCT02528188; Study 1) conducted between July 2015 and February 2019 [14] and a phase 3, randomized, double-blind, multicenter, placebo-controlled, parallel-group trial (NCT02709486; Study 2) conducted between March 2016 and November 2018 [13]. Both studies were conducted in accordance with the Helsinki Declaration and the ethical principles of Good Clinical Practice. Both studies were approved by the appropriate institutional review boards and regulatory agencies. Informed consent was obtained from individuals in each study.
Patient Population
The population for this analysis comprised patients enrolled at study centers in Japan. Patients eligible for the full study populations were age ≥ 18 years with a clinical diagnosis of OA of the hip/knee in the index joint (the most painful joint at baseline with a qualifying Western Ontario and McMaster Universities Osteoarthritis Index [WOMACFootnote 1] Pain subscale score) that fulfilled American College of Rheumatology classification criteria [19, 20], including radiographic confirmation (Kellgren-Lawrence grade ≥ 2) by the Central Reader [21]. Patients also had a history of inadequate pain relief with acetaminophen and inadequate pain relief with, contraindication to, or intolerance of tramadol or other non-tramadol opioid analgesics, or unwillingness to take opioid analgesics. For Study 2, eligible patients also needed to have a history of inadequate pain relief with, contraindication to, or intolerance of NSAIDs. For Study 1, administration of a stable dose of an oral NSAID for ≥ 30 days before screening was required. In addition, WOMAC [22] Pain and Physical Function subscale scores ≥ 5 in the index joint and a Patient’s Global Assessment of OA (PGA-OA) rating of “fair,” “poor,” or “very poor” (for Study 1, PGA-OA ratings were required while receiving stable doses of an oral NSAID for ≥ 2 weeks during screening and before randomization) were necessary study criteria.
In Study 1, specific eligibility criteria for the subgroup of Japanese patients were a stable dose regimen of celecoxib 100 mg twice daily with compliance ≥ 70% for ≥ 2 weeks of the screening period directly prior to the baseline (Day 1) visit. Japanese females were required to be of nonchildbearing potential in both studies.
Patients with evident (radiographic) rapidly progressive or atrophic OA, subchondral insufficiency or pathologic fractures, and osteonecrosis as confirmed by the Central Reader were not eligible. Those with a body mass index > 39 kg/m2 were also excluded. Further details of eligibility criteria have been published previously [13, 14].
Treatment
Study 1 (NCT02528188) [14]
During the screening period (≤ 37 days prior to randomization), Japanese patients maintained stable open-label oral celecoxib 100 mg twice daily for ≥ 2 weeks of the screening period. Patients were randomized (1:1:1) to subcutaneous tanezumab 2.5 mg or 5 mg at baseline and every 8 weeks, or twice-daily oral celecoxib, for a 56-week double-blind, double-dummy treatment period (Supplementary Fig. S1). At Week 16, patients were required to meet the following response criteria: ≥ 30% reduction in WOMAC Pain subscale score relative to baseline in the index joint and ≥ 15% reduction in the WOMAC Pain subscale score from baseline at Week 2, 4, or 8. If the criteria were not met, the patient was discontinued from the treatment period and entered the 24-week early termination safety follow-up period. Patients who completed the 56-week double-blind treatment period also entered a 24-week safety follow-up period.
Study 2 (NCT02709486) [13]
Following the screening period (≤ 37 days prior to randomization), patients were randomized (1:1:1) to subcutaneous tanezumab 2.5 mg, tanezumab 5 mg, or matching placebo, administered at baseline and every 8 weeks of the 24-week double-blind treatment period. This was followed by a 24-week safety follow-up period (Supplementary Fig. S2).
Use of analgesics (including marijuana) except acetaminophen/paracetamol was prohibited through Week 64 (Study 1) and Week 32 (Study 2). In Study 1, use of non-assigned NSAIDs was also prohibited through Week 64. Occasional use of analgesics (including NSAIDs in Study 2) was permitted for self-limiting conditions unrelated to OA, but not within 48 h or 5 half-lives (whichever was greater) of study visits for efficacy assessment in either study. However, in Study 2, such limited concomitant use of NSAIDs should not have exceeded 40 days of use between baseline and Week 32, and other use of NSAIDs was prohibited. Patients in Study 2 could use NSAIDs beginning at Week 32. Acetaminophen was allowed as rescue therapy in patients with inadequate pain relief except for ≤ 24 h before study visits for efficacy assessment. In Study 1, acetaminophen was dosed at ≤ 3000 mg/day for ≤ 3 days/week to Week 16 and as needed thereafter to Week 64, then as needed (as permitted by local or national labeling) until the final study visit. In Study 2, the dose of acetaminophen was ≤ 4000 mg/day (or as permitted by local or national labeling) ≤ 5 days/week up to Week 24, and then as needed until the final study visit. Aspirin doses ≤ 325 mg/day were permitted for cardiovascular prophylaxis in both studies.
Endpoints and Assessments
The efficacy and general safety results of a subgroup analysis of the Japanese patients from Study 2 have been published [23]. In the current analysis, we included efficacy and overall safety findings of the Japanese patients from Study 1; Japanese patients from Study 2 were only included in the integrated safety analysis.
The three co-primary efficacy endpoints were change from baseline to Week 16 in (1) the WOMAC Pain subscale score, (2) the WOMAC Physical Function subscale score, and (3) the PGA-OA score. This study defined the Japanese specific co-primary endpoints which consisted of change from baseline to Week 16 in the WOMAC Pain subscale score and Physical Function subscale score.
Overall safety in Japanese patients in Study 1 was assessed by the incidence of treatment-emergent adverse events (TEAEs) using Medical Dictionary for Regulatory Activities v.21.1 coding. A serious TEAE was defined as any untoward medical occurrence at any dose that resulted in death, persistent or significant disability/incapacity (substantial disruption of the ability to conduct normal life functions), or congenital anomaly/birth defect; was life-threatening (immediate risk of death); or required inpatient hospitalization or prolongation of existing hospitalization. The maximum intensity of the TEAEs was reported by the investigator as mild (did not interfere with patient's usual function), moderate (interfered to some extent with patient's usual function), and severe (interfered significantly with patient's usual function). A severe TEAE was not necessarily a serious TEAE.
For the integrated safety analysis of Study 1 and Study 2, the incidence of the composite joint safety endpoint (CJSE) and its components are presented. The CJSE included any patient with an adjudicated outcome of primary osteonecrosis, RPOA type 1 (RPOA1) or type 2 (RPOA2), subchondral insufficiency fracture, or pathological fracture. RPOA1 was defined as those events considered to have significant loss of joint space width (≥ 2 mm) within approximately 1 year without gross structural failure. RPOA2 events were those considered to have abnormal loss or destruction of bone including limited or total collapse of at least one subchondral surface that is not normally present in conventional end-stage osteoarthritis [24,25,26]. The blinded adjudication committee comprised external experts in orthopedic surgery, rheumatology, orthopedic pathology, and radiology, with expertise in patients with end-stage OA and osteonecrosis. The committee reviewed all patients reported to have joint-related safety events identified during the study and all patients who underwent total joint replacement during the study.
See Supplementary Materials for more details of the two studies.
Statistical Methods
The efficacy and general safety data are presented for Japanese patients who were randomized and received tanezumab or NSAID in Study 1. For efficacy analysis in Japanese patients in Study 1, least square (LS; i.e., model-estimated) mean change from baseline (per treatment group and for tanezumab groups versus NSAID) were calculated for efficacy endpoints using multiple imputation for missing data. The analysis of covariance (ANCOVA) model for imputed datasets included treatment, randomization stratification variables (index joint, highest Kellgren-Lawrence grade) as fixed effects, baseline value (i.e., PGA-OA score, WOMAC Pain subscale score, and WOMAC Physical Function subscale score for respective endpoint), and baseline diary average pain as covariates, and study site as a random effect. Joint safety data are presented for a pooled population of Japanese patients included in the safety population of Study 1 and Study 2. Baseline characteristics and safety data are summarized descriptively. Statistical significance was not evaluated. Comparisons between groups are descriptive only.
Results
Patient Disposition and Baseline Characteristics
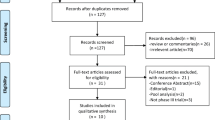
Efficacy and safety data for the overall study population and the Japanese patients in Study 2 have been previously presented [13, 14, 23]. The current efficacy and general safety analysis only included Study 1 patients enrolled in the study centers in Japan. In Study 1, 200 Japanese patients were randomized and were included in both the intent-to-treat and safety populations [tanezumab 2.5 mg, n = 74; tanezumab 5 mg, n = 59; NSAID, n = 67 (Fig. 1a)]. Baseline characteristics were well balanced across treatment groups (Table 1). Across the treatment groups most patients were female (62.7–71.6%), and the mean age was 63.6–66.7 (range 40–88) years. The mean body mass index was 26.4–27.1 kg/m2 (range 16–37 kg/m2), and the knee was the OA index joint for most patients (88.1–93.2%), followed by the hip (6.8–11.9%). Most patients had an index joint Kellgren-Lawrence grade of 3 (52.7–66.1%), on a scale of 0 (no radiographic OA) to 4 (severe radiographic OA). The means [standard deviation (SD)]) for the WOMAC Pain subscale score, WOMAC Physical Function subscale score, and the PGA-OA score were 6.55 (0.96)–6.74 (1.17), 6.60 (1.02)–6.87 (1.13), and 3.28 (0.45)–3.51 (0.57), respectively.
Patient disposition. a Japanese patients enrolled in Study 1. b Japanese patients in the pooled safety population. a Completed study: patients who completed the planned safety follow-up period. b Discontinued study: patients who did not enter or discontinued the planned safety follow-up period, either completed or discontinued the planned treatment period. c Only Japanese patients in Study 1 were included in the efficacy and general safety analysis. Efficacy and general safety results of the Japanese patients in Study 2 have been published previously [23]. d Adjudicated joint safety outcomes were reported for Japanese patients in both Study 1 and Study 2. NSAID nonsteroidal anti-inflammatory drug
In the pooled safety population from both studies, 306 Japanese patients were analyzed for safety (placebo, n = 34; tanezumab 2.5 mg, n = 112; tanezumab 5 mg, n = 93; NSAID, n = 67 (Fig. 1b). Baseline characteristics were comparable across the treatment groups (Table 2). Age ranged from 34 to 88 years, and most patients had a body mass index < 30 kg/m2. The most common OA index joint was the knee (87.1–92.9%), and > 50% of patients had an index joint of Kellgren-Lawrence grade 3. Similar to the patients in Study 1, WOMAC Pain subscale score [mean (SD)], WOMAC Physical Function subscale score, and the PGA-OA score were 6.4 (1.1)–6.7 (1.1), 6.5 (1.0)–6.8 (1.0), and 3.3 (0.5)–3.5 (0.6), respectively.
Efficacy: Study 1
At Week 16, Japanese patients treated with tanezumab 2.5 mg and 5 mg showed improvements in WOMAC Pain and Physical Function subscale scores and PGA-OA scores that were numerically greater than observed in the patients treated with NSAIDs (Table 3).
Overall Safety: Study 1
In total, 200 Japanese patients were randomized to tanezumab 2.5 mg (n = 74), tanezumab 5 mg (n = 59), and NSAID (n = 67). Of the 104 patients [tanezumab 2.5 mg, n = 41 (55.4%); tanezumab 5 mg, n = 29 (49.2%); NSAID, n = 34 (50.7%)] who completed the 56-week treatment phase, 99 (49.5% of randomized) completed the following 24-week safety follow-up [tanezumab 2.5 mg, n = 39 (52.7%); tanezumab 5 mg, n = 27 (45.8%); NSAID, n = 33 (49.3%)]. Of the 96 patients who discontinued the treatment phase, 78 patients completed the safety follow-up; 2 (2.7%), 5 (8.5%), and 2 (3.0%) patients in the tanezumab 2.5 mg, 5 mg, and the NSAID groups, respectively, discontinued the safety follow-up and 3 (4.1%), 4 (6.8%), and 2 (3.0%) patients did not enter the safety follow-up.
During the treatment period (first dose to Week 56), TEAEs (all causalities) were reported in 81.1%, 74.6%, and 76.1% of patients in the tanezumab 2.5 mg, tanezumab 5 mg, and NSAID groups, respectively. The majority of TEAEs were mild or moderate in severity; 2 (2.7%), 5 (8.5%), and 3 (4.5%) patients in these treatment groups, respectively, experienced severe TEAEs. Serious TEAEs were reported in 8.1%, 11.9%, and 9.0% of patients in the tanezumab 2.5 mg, tanezumab 5 mg, and NSAID groups, respectively (Table 4). The most common serious TEAEs in tanezumab-treated patients were musculoskeletal and connective tissue disorders (4.1% in the tanezumab 2.5 mg group and 11.9% in the tanezumab 5 mg group) (Supplementary Table S1). Overall, the most common TEAEs reported during the treatment period in the tanezumab 2.5 mg, tanezumab 5 mg, and NSAID groups, respectively, were nasopharyngitis (24.3%, 16.9%, 26.9%), arthralgia (6.8%, 16.9%, 7.5%), osteoarthritis (5.4%, 11.9%, 6.0%), and back pain (4.1%, 6.8%, 7.5%) (Table 4). The incidence of study drug discontinuation due to TEAEs was lowest in the tanezumab 2.5 mg group (1.4%) and similar in the tanezumab 5 mg (6.8%) and NSAID (7.5%) groups. No deaths were reported during the study.
During the safety follow-up period (24-week period following 56-week treatment period), 52.1%, 50.9%, and 43.1% of patients in the tanezumab 2.5 mg, tanezumab 5 mg, and NSAID groups reported TEAEs (all causalities), with 2.8%, 3.6%, and 0% of patients reporting severe TEAEs. Similar to the treatment period, musculoskeletal and connective tissue disorders were the most common system organ class affected.
During the treatment period and up to the end of the study at Week 80 (the treatment period plus the 24-week safety follow-up), the incidence of TEAEs was generally similar among tanezumab 2.5 mg, 5 mg, and NSAID groups. Most TEAEs were mild or moderate in severity (Table 4, Supplementary Table 1).
Joint Safety: Studies 1 and 2
Overall, 28 (9.2%) Japanese patients were adjudicated for joint safety events in the pooled safety population (Table 5; Supplementary Table S2 summarizes joint safety events for Study 1). Most of these patients (n = 18) were adjudicated as normal OA progression. Ten patients were adjudicated to have a component of the CJSE, all in the tanezumab groups [2.5 mg, n = 4 (3.6%); 5 mg, n = 6 (6.5%)]. The observation time-adjusted rate [95% confidence interval (CI)] of the primary CJSE was 65.5 [29.4, 145.8] events/1000 patient-years in the tanezumab 5 mg group and 34.4 [12.9, 91.7] events/1000 patient-years in the 2.5 mg group.
Seven patients were adjudicated to have RPOA1, 2 (2/112, 1.8%) in the tanezumab 2.5 mg group and 5 (5/93, 5.4%) in the tanezumab 5 mg group. RPOA1 affected the knee in 2 (2/112, 1.8%) and 4 (4/93, 4.3%) patients in the tanezumab 2.5 mg and 5 mg groups, respectively. RPOA1 affected the hip in 1 (1/93, 1.1%) patient in the tanezumab 5 mg group. The affected joint was Kellgren-Lawrence grade 3 at baseline for both patients (index joint for both) in the tanezumab 2.5 mg group, and grade 1 (n = 2) or 2 (n = 3) for patients (non-index joint for all) in the tanezumab 5 mg group. For the tanezumab 2.5 mg group, one patient had RPOA1 during the follow-up period after completing the treatment period; the other patient had RPOA1 during the follow-up period after discontinuing the treatment period. For the tanezumab 5 mg group, two patients had RPOA1 during the treatment period, two patients had RPOA1 during the follow-up period after completing the treatment period, and one patient had RPOA1 after completing the follow-up period after the discontinued treatment period. The observation time-adjusted rate (95% CI) was higher in the tanezumab 5 mg group versus the 2.5 mg group [54.5 (22.7, 130.9) versus 17.2 (4.3, 68.7) events/1000 patient-years].
RPOA2 occurred in the hip joint of two patients, one (1/112, 0.9%) in the tanezumab 2.5 mg group and one (1/93, 1.1%) in the tanezumab 5 mg group. The Kellgren-Lawrence grades of the affected joints at baseline were 4 (index joint) in the 2.5 mg group and 0 (non-index joint) in the 5 mg group. Both patients had RPOA2 during the treatment period. Similar observation time-adjusted rates (95% CI) were observed between the tanezumab 5 mg group [10.7 (1.5, 76.1) events/1000 patient-years] and the tanezumab 2.5 mg group [8.6 (1.2, 60.7) events/1000 patient-years]. No RPOA1 and RPOA2 occurred in the NSAIDs or placebo group.
One patient in the tanezumab 2.5 mg group had primary osteonecrosis in the hip (non-index joint), with a baseline Kellgren-Lawrence grade of 0. This patient had a history of alcoholic liver disease which may have predisposed the patient to osteonecrosis. The observation time-adjusted rate (95% CI) was 8.5 (1.2, 60.7) events/1000 patient-years. No patients were adjudicated as having pathological fracture or subchondral insufficiency fracture.
Discussion
This subgroup analysis of two phase 3 trials [13, 14] assessed the efficacy, overall safety, and joint safety of tanezumab in Japanese patients with OA. Study 1 was NSAID-controlled [14], whereas Study 2 was placebo-controlled [13]. Based on data from Study 1, Japanese patients who received tanezumab 2.5 mg and 5 mg showed improvements from baseline to Week 16 in WOMAC Pain subscale score, WOMAC Physical Function subscale score, and PGA-OA score. These improvements were numerically greater than observed in the patients treated with NSAID, although no statistical significance testing was performed. In the overall population of Study 1, numerical improvements were also observed with tanezumab 2.5 and 5 mg from baseline to Week 16 in WOMAC Pain subscale, WOMAC Physical Function subscale, and PGA-OA scores that were larger than those in NSAIDs. The changes from baseline at Week 16 observed with tanezumab 5 mg were statistically significant for WOMAC Pain and WOMAC Physical Function subscale scores compared with NSAIDs. This was not observed for tanezumab 2.5 mg [14].
For the full study population, pain and physical function improved with tanezumab; AEs were similar for placebo, NSAID, and tanezumab 2.5 mg groups, with numerically more AEs in the tanezumab 5 mg group; and more joint safety events occurred in the tanezumab group compared with the placebo and the NSAID group [13, 14]. Overall safety was assessed using data from Study 1 in the current analysis. In Japanese patients, the incidence of TEAEs was generally similar among the tanezumab (2.5 mg and 5 mg) and NSAID treatment groups. Most TEAEs were mild or moderate in severity.
Joint safety was evaluated in a pooled safety population of Japanese patients from Study 1 and Study 2. In the overall population in Study 1, the adjudicated joint safety endpoint occurred most frequently in patients receiving tanezumab 5 mg (7.1%) compared with 2.5 mg (3.9%) and NSAID (1.5%) [14]. The result of Japanese subpopulation analysis was similar to that in the overall population; the adjudicated joint safety endpoint did not occur in the placebo and NSAID groups but only in tanezumab-treated patients at an incidence of 3.6% in the tanezumab 2.5 mg group and 6.5% in the 5 mg group. Similarly, in Study 2, the adjudicated CJSE occurred in 3.2% and 1.8%, respectively, of patients in the tanezumab 5 mg and 2.5 mg groups [13]. RPOA1 was the most common joint safety event in the pooled analysis, similar to the overall study populations in Study 1 and Study 2 [13, 14].
Limitations of this subgroup analysis included the small sample size of Japanese patients, which may limit the analyses of efficacy and safety and the conclusions that can be drawn. This was a descriptive analysis, and statistical conclusions were not made. In addition, although excessive malalignment of the knee was an exclusion criterion, the presence of varus and valgus malalignment of the knee may contribute to the progression of OA; if the baseline stage of disease is more advanced, a more rapid progression of OA may be observed [27].
Conclusions
A descriptive profile of the efficacy, overall safety, and joint safety outcomes of subcutaneous tanezumab among Japanese patients has been presented. Both the results of the current analysis and those of the subgroup analysis of Study 2 [23] were generally consistent with the overall study populations for Japanese patients with moderate-to-severe OA in the hip or knee who have experienced inadequate pain relief with standard analgesic treatment.
Notes
1996 Nicholas Bellamy. WOMAC® is a registered trademark of Nicholas Bellamy (CDN, EU, USA).
References
Muraki S, Oka H, Akune T, et al. Prevalence of radiographic knee osteoarthritis and its association with knee pain in the elderly of Japanese population-based cohorts: the ROAD study. Osteoarthr Cartil. 2009;17:1137–43.
Iidaka T, Muraki S, Akune T, et al. Prevalence of radiographic hip osteoarthritis and its association with hip pain in Japanese men and women: the ROAD study. Osteoarthr Cartil. 2016;24:117–23.
OARSI. Current status of and prospects for osteoarthritis treatment—development of Japanese OA guidelines based on OARSI part 2. 2011. https://oarsi.org/education/oarsi-resources/current-status-and-prospects-osteoarthritis-treatment-development-japanese. Accessed 02 Feb 2022.
Akazawa M, Mimura W, Togo K, et al. Patterns of drug treatment in patients with osteoarthritis and chronic low back pain in Japan: a retrospective database study. J Pain Res. 2019;12:1631–48.
Bally M, Dendukuri N, Rich B, et al. Risk of acute myocardial infarction with NSAIDs in real world use: bayesian meta-analysis of individual patient data. BMJ. 2017;357:j1909.
Bhala N, Emberson J, Merhi A, et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 2013;382:769–79.
Fairweather J, Jawad ASM. Cardiovascular risk with nonsteroidal anti-inflammatory drugs (NSAIDs): the urological perspective. BJU Int. 2012;110:E437.
Ungprasert P, Srivali N, Thongprayoon C. Nonsteroidal anti-inflammatory drugs and risk of incident heart failure: a systematic review and meta-analysis of observational studies. Clin Cardiol. 2016;39:111–8.
Harirforoosh S, Asghar W, Jamali F. Adverse effects of nonsteroidal antiinflammatory drugs: an update of gastrointestinal, cardiovascular and renal complications. J Pharm Pharm Sci. 2013;16:821–47.
Nagashima H, Suzuki M, Araki S, Yamabe T, Muto C. Preliminary assessment of the safety and efficacy of tanezumab in Japanese patients with moderate to severe osteoarthritis of the knee: a randomized, double-blind, dose-escalation, placebo-controlled study. Osteoarthr Cartil. 2011;19:1405–12.
Schnitzer TJ, Marks JA. A systematic review of the efficacy and general safety of antibodies to NGF in the treatment of OA of the hip or knee. Osteoarthr Cartil. 2015;23(Suppl 1):S8-17.
Schnitzer TJ, Easton R, Pang S, et al. Effect of tanezumab on joint pain, physical function, and patient global assessment of osteoarthritis among patients with osteoarthritis of the hip or knee: a randomized clinical trial. JAMA. 2019;322:37–48.
Berenbaum F, Blanco FJ, Guermazi A, et al. Subcutaneous tanezumab for osteoarthritis of the hip or knee: efficacy and safety results from a 24-week randomised phase III study with a 24-week follow-up period. Ann Rheum Dis. 2020;79:800–10.
Hochberg MC, Carrino JA, Schnitzer TJ, et al. Long-term safety and efficacy of subcutaneous tanezumab versus nonsteroidal antiinflammatory drugs for hip or knee osteoarthritis: a randomized trial. Arthritis Rheumatol. 2021;73:1167–77.
Hochberg MC, Tive LA, Abramson SB, et al. When Is osteonecrosis not osteonecrosis?: adjudication of reported serious adverse joint events in the tanezumab clinical development program. Arthritis Rheumatol. 2016;68:382–91.
Belanger P, Butler P, Butt M, et al. From the cover: evaluation of the effects of tanezumab, a monoclonal antibody against nerve growth factor, on the sympathetic nervous system in adult cynomolgus monkeys (Macaca fascicularis): a stereologic, histomorphologic, and cardiofunctional assessment. Toxicol Sci. 2017;158:319–33.
Pfizer. Pfizer reports third-quarter 2021 results. 2021. https://investors.pfizer.com/investor-news/press-release-details/2021/PFIZER-REPORTS-THIRD-QUARTER-2021-RESULTS/default.aspx. Accessed 19 Apr 2022.
Eli Lilly and Company. Lilly Reports Robust Third-Quarter 2021 Financial Results as Pipeline Success Strengthens Future Growth Potential. 2021. https://investor.lilly.com/static-files/a0b77c52-a997-41c1-9534-5f465903a0b4. Accessed 19 Apr 2022.
Altman R, Alarcón G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34:505–14.
Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29:1039–49.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502.
Theiler R, Spielberger J, Bischoff HA, et al. Clinical evaluation of the WOMAC 3.0 OA Index in numeric rating scale format using a computerized touch screen version. Osteoarthr Cartil. 2002;10:479–81.
Berenbaum F, Langford R, Perrot S, et al. Subcutaneous tanezumab for osteoarthritis: Is the early improvement in pain and function meaningful and sustained? Eur J Pain. 2021;25:1525–39.
Roemer FW, Hayes CW, Miller CG, Hoover K, Guermazi A. Imaging atlas for eligibility and on-study safety of potential knee adverse events in anti-NGF studies (Part 1). Osteoarthr Cartil. 2015;23(Suppl 1):S22-42.
Roemer FW, Hayes CW, Miller CG, Hoover K, Guermazi A. Imaging atlas for eligibility and on-study safety of potential hip adverse events in anti-NGF studies (Part 2). Osteoarthr Cartil. 2015;23(Suppl 1):S43-58.
Roemer FW, Hayes CW, Miller CG, Hoover K, Guermazi A. Imaging atlas for eligibility and on-study safety of potential shoulder adverse events in anti-NGF studies (Part 3). Osteoarthr Cartil. 2015;23(Suppl 1):S59-68.
Cerejo R, Dunlop DD, Cahue S, et al. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46:2632–6.
Acknowledgements
Funding
This study was sponsored by Pfizer and Eli Lilly & Company. The journal’s Rapid Service Fee was funded by the sponsors.
Medical Writing Assistance
Medical writing support was provided by Neel Misra, MSc CMPP, and Shuang Li, PhD CMPP, of Engage Scientific Solutions and funded by Pfizer and Eli Lilly and Company.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors critically reviewed the draft manuscript and approved the final version of the manuscript for publication.
Prior Presentation
Part of the content has been presented as an oral presentation at the Japanese Orthopaedic Association—94th Annual Meeting (20–23 May 2021, Tokyo, Japan).
Disclosures
Kenji Miki has received payment from Merck, Pfizer, Lilly, Ayumi, Mundi Pharma, Janssen, Nippon Zoki, and Daiichi Sankyo. Makoto Ohta, Manabu Abe, Hiroki Yoshimatsu, Koichi Fujii, Nozomi Ebata, Christine R. West, Mark T. Brown, and Glenn Pixton are full-time employees of, and own stock and/or options in, Pfizer. Naoki Isogawa was an employee of Pfizer when the studies were carried out; he is an employee of UCB Japan Co. Ltd. Pfizer and Eli Lily and Company contributed to the study design; Pfizer contributed to the management and collection of data. In their role as authors, employees of Pfizer and Eli Lilly were involved in the interpretation of data, preparation, review, and approval of the manuscript and the decision to submit for publication, along with their co-authors. The study sponsors approved the manuscript from an intellectual property perspective but had no right to veto the publication.
Compliance with Ethics Guidelines
The studies (ClinicalTrials.gov: NCT02528188 and NCT02709486) were conducted in accordance with the Helsinki Declaration and the ethical principles of Good Clinical Practice. Both studies were approved by the appropriate institutional review boards and regulatory agencies. Informed consent was obtained from individuals in each study.
Data Availability
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Miki, K., Ohta, M., Abe, M. et al. Efficacy, General Safety, and Joint Safety of Tanezumab in Japanese Patients with Osteoarthritis: Subgroup Analyses from Two Randomized, Phase 3 Studies. Pain Ther 11, 827–844 (2022). https://doi.org/10.1007/s40122-022-00384-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00384-y