Abstract
Introduction
Long-acting lipoglycopeptides such as dalbavancin may have utility in patients with Gram-positive bloodstream infections (BSI), particularly in those with barriers to discharge or who require prolonged parenteral antibiotic courses. A retrospective cohort study was performed to provide further multicenter real-world evidence on dalbavancin use as a sequential therapy for Gram-positive BSI.
Methods
One hundred fifteen patients received dalbavancin with Gram-positive BSI, defined as any positive blood culture or diagnosed with infective endocarditis, from 13 centers geographically spread across the United States between July 2015 and July 2021.
Results
Patients had a mean (SD) age of 48.5 (17.5) years, the majority were male (54%), with many who injected drugs (40%). The most common infection sources (non-exclusive) were primary BSI (89%), skin and soft tissue infection (SSTI) (25%), infective endocarditis (19%), and bone and joint infection (17%). Staphylococcus aureus accounted for 72% of index cultures, coagulase-negative Staphylococcus accounted for 18%, and Streptococcus species in 16%. Dalbavancin started a median (Q1–Q3) of 10 (6–19) days after index culture collection. The most common regimen administered was dalbavancin 1500 mg as one dose for 50% of cases. The primary outcome of composite clinical failure occurred at 12.2%, with 90-day mortality at 7.0% and 90-day BSI recurrence at 3.5%.
Conclusions
Dalbavancin may serve as a useful tool in facilitating hospital discharge in patients with Gram-positive BSI. Randomized controlled trials are anticipated to validate dalbavancin as a surrogate to current treatment standards.
Similar content being viewed by others
Why carry out this study? |
Gram-positive bacteremia requires extended durations of antibiotics, and it is difficult to guarantee treatment adherence in certain populations utilizing discharge to acute rehabilitation facilities with intravenous or oral antibiotics. |
Long-acting glycopeptides such as dalbavancin can provide a convenient option to assist in treatment completion, but dosing regimens for sequential glycopeptides are not standardized with treatment outcomes unclear. |
What was learned from the study? |
Sequential dalbavancin treatment after bloodstream infection was most often dosed at 1500 mg for one dose and had low composite clinical failure at 12.2% with 90-day mortality at 7.0%. |
Common patient populations were a bimodal age distribution younger than 40 years old and older than 50 years old, a large proportion who injected drugs (40%), and positive outcomes of dalbavancin occurred both in uncomplicated and complicated bacteremia. |
Introduction
Gram-positive bloodstream infections (BSI) represent a significant disease burden, for which treatment modalities have not changed for many decades. Certain pathogens, such as Staphylococcus aureus, require intravenous antibiotic therapy for at least 14 days according to conventional guidelines and often warrant longer durations of therapy for complicated infections [1]. Intravenous antibiotics can be generally expensive, require intensive monitoring, and subsequently, often act as a barrier to hospital discharge. Additionally, prolonged courses of parenteral antibiotics can be associated with deleterious adverse events such as line-related infections. An alternative treatment modality of oral antibiotics can be used as step-down therapy for a variety of infection types including BSI. These oral step-down therapies have been evaluated in randomized-controlled trials for complicated infections and Staphylococcus aureus BSI; however, not all patients may benefit from this treatment option due to adherence issues, less generalizable study populations, and other concerns [2,3,4,5]. Patients with disposition or other clinical challenges may preclude intravenous or oral antibiotic use, and they may benefit from long-term lipoglycopeptides such as dalbavancin. These antibiotics have long elimination half-lives and broad coverage against many Gram-positive organisms, allowing for weekly or biweekly dosing [6, 7].
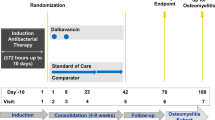
Dalbavancin was approved based on the DISCOVER 1 and 2 trials of 1312 patients with bacterial skin and soft tissue infection (SSTI) randomized to receive dalbavancin compared against vancomycin or linezolid. Dalbavancin was found to be non-inferior in patient outcomes and thus subsequently approved for use in SSTI [8]. Once approved, many providers and researchers began to investigate dalbavancin’s off-label use among uncomplicated and complicated invasive infections and in vulnerable populations [9,10,11,12,13,14,15,16,17,18,19]. There were positive phase II data showing dalbavancin as non-inferior to vancomycin in 2005 in catheter-associated BSI before the targeted trial for approval was done; however it was likely not a common enough indication for large phase III approval [20]. A subsequent randomized controlled trial post-approval was developed comparing dalbavancin against standard of care for complicated BSI or infective endocarditis but it was terminated for business reasons in 2017 [21]. At present, evidence regarding dalbavancin as a sequential step-down therapy for invasive infections is limited to case series, single-center observational cohort studies, and small randomized controlled trials focused on osteomyelitis [13,14,15,16,17,18,19]. Questions remain as to the optimal dosing, frequency, and indications for dalbavancin use [22,23,24,25]. Therefore, it is important to assess dalbavancin utilization, safety, and rates of cure for these infections in order to optimize treatment and decrease hospital length of stay.
This investigation was developed with the aim of providing further multicenter evidence on dalbavancin use as sequential therapy for Gram-positive BSI and provide a current real-world comparison for past and future studies in the United States.
Methods
This is a retrospective, observational, multicenter, cohort study of patients with Gram-positive BSI, with or without suspected endocarditis, receiving dalbavancin from participating centers from May 2014 to December 2021. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. Approval was obtained from Wayne State University (#012019MP2E), Henry Ford Hospital (#14715) and all of the contributing medical centers with a waiver for informed consent due to the retrospective nature of the study design. We included adults (≥ 18 years) with ≥ 1 positive blood culture or diagnosed infective endocarditis who were treated with ≥ 1 dose of dalbavancin. Patients were excluded if they were pregnant, a prisoner, or had recent prior dalbavancin use in the past 90 days. Patient demographics, medical history, risk factors for multi-drug resistance (MDR) acquisition (e.g., prior antibiotic and healthcare exposures), clinical laboratory data, disease severity (APACHE-II score), microbiology, infection source, treatment parameters (antibiotic, dose, duration), and outcomes were collected from the electronic medical record retrospectively from collaborators at each institution.
Study variable definitions include complicated bacteremia defined as at least one of the following: infective endocarditis source of infection, isolation of a Gram-positive organism from blood cultures on at least 2 days through day 5 of assigned therapy, metastatic sites of infection, or infection involving prostheses not removed within 4 days [26]. Uncomplicated BSI was defined by at least one of the following factors with no criteria for complicated bacteremia: no implanted prostheses, follow-up blood cultures obtained 2–4 days after initial therapy finalized as no growth, defervescence within 72 h of initiating effective antimicrobial therapy, or no evidence of metastatic sites of infection.
Primary outcome was a composite of 90-day all-cause mortality from index culture, 90-day BSI recurrence from index culture, and 90-day infection-related readmission. Secondary outcomes were a composite of 90-day mortality or 90-day recurrence of infection (known as treatment failure), individual components of the composite outcomes, and 90-day all-cause readmission from discharge. A pre-specified subgroup analysis of uncomplicated and complicated BSI was compared using primary and secondary outcomes.
Descriptive statistics were calculated using IBM SPSS Statistics, version 28.0 (IBM Corp., Armonk, NY, USA). Missing values were omitted for variables collected and an updated denominator was noted in the variable row of descriptive tables. Comparisons between complicated and uncomplicated infections were performed using Chi-squared and Fisher’s exact tests as appropriate for nominal variables. Ordinal and continuous variables were analyzed using the Mann–Whitney U test and Student’s t test and central tendency was described using median and mean, for nonparametric and parametric data, respectively. Patient clinical data were collected and managed using the Research Electronic Data Capture (REDCap) tool hosted at Wayne State University [27].
Results
A total of 115 patient cases met inclusion and exclusion criteria from 13 unique urban academic medical systems across the United States (Table 1). Contributing cases were 32 (27.8%) from Brigham and Women’s, 13 (11.3%) from Augusta University Medical Center, 12 (10.4%) from Swedish American Health System, 12 (10.4%) from Beth Israel Deaconess Medical Center, 11 (9.6%) from State University of New York Upstate Medical Hospital, nine (7.8%) from St. Joseph’s Candler Health System, eight (7.0%) from University of Tennessee, seven (6.1%) from Brown Medical Center, five (4.3%) from Moses Cone Memorial Hospital, three (2.6%) from Sharp Memorial Hospital, one (0.9%) from Cone Health Alamance Regional Medical Center, one (0.9%) from Mon Health Medical Center, and one (0.9%) from Henry Ford Hospital. Patient visit dates ranged from July 2015 to July 2021. Patients included had a mean (SD) age of 48.5 (17.5) years in a bimodal distribution (Fig. 1), 54% were male, 84% Caucasian, median (Q1–Q3) BMI of 25.1 (21.8–29.3) kg/m2, and 40% were patients who inject drugs (PWID). The median (Q1–Q3) length of stay for BSI patients receiving dalbavancin was 10 (7–20) days, with 9.6% of patients having a ‘patient-directed discharge’ formerly known as leaving Against Medical Advice (AMA) [28]. The most common sources of infection (non-exclusive) were primary BSI (89%), SSTI (25%), infective endocarditis (19%), and bone and joint infection (17%).
Table 2 details microbiology and BSI therapies received as inpatient prior to dalbavancin. S. aureus was present in the index culture in 72% of cases, with MRSA in 47% and MSSA in 25% of all cases. Coagulase-negative Staphylococcus was an index pathogen in 18% of cases, Streptococcus species in 16% of cases, Enterococcus in 2.6%, and one patient (0.9%) had Corynebacterium in index culture for BSI. Patients were classified as complicated BSI in 46% of cases, uncomplicated BSI in 44%, and unknown type in 10% of cases. The median (Q1–Q3) BSI duration was 56 (33–105) hours among patients with documentation of culture clearance and nearly all patients (98%) received an infectious diseases (ID) consult. Vancomycin was predominantly used (85%) prior to initiation of dalbavancin, with cefazolin (24%), and daptomycin (17%) used to lesser degrees. Dalbavancin treatment was started a median (Q1–Q3) of 10 (6–20) days after admission date and 10 (6–19) days after index culture collection (Table 3). Dalbavancin was most often given on the day of discharge (45%), but also given prior to discharge (27%) likely inpatient, and post-discharge (25%), which was likely given as outpatient. Dalbavancin courses averaged (SD) 1.7 (1.6) doses, with the most common initial dose being 1500 mg (68%) or 1000 mg (30%). The most common regimen was 1500 mg as a one-time dose (50%), with 1000 mg as a one-time dose the next most common regimen (15%). The most common reason for dalbavancin use was predominantly for convenience (87%), with ease of administration (41%) and inability to receive a peripherally inserted central catheter (PICC) due to PWID (34%) as the most common reasons under convenience (Table 3). Nearly all patients completed their planned dalbavancin therapy (90%) with the majority (71%) having follow-up after their last dalbavancin dose.
The primary composite outcome of clinical failure included 90-day mortality from index culture, 90-day recurrence of BSI, and 90-day infection-related readmission since discharge occurred in 12.2% of patients (Table 4). Composite 90-day treatment failure was low at 7.8%, which is consistent with low 90-day mortality (7.0%) and low 90-day recurrence (3.5%) from index culture. While 90-day readmission was higher (27% out of n = 81 available), infection-related readmissions were low (6.3% out of n = 79 available). Adverse events were low overall (9%). In addition, out of 97 evaluable patients in this cohort, only seven patients had a microbiological isolate with minimal inhibitory concentration (MIC) information 1 year after dalbavancin initiation. Four were Staphylococcus aureus, two were coagulase-negative Staphylococcus spp., one was Enterococcus gallinarum, and one was an unlabeled other pathogen. All seven isolates remained susceptible to vancomycin with MIC ≤ 2 mg/l.
A comparison between complicated vs. uncomplicated BSI is shown in Table 5. Patients with complicated BSI were younger, primarily Caucasian, more frequently received daptomycin prior to dalbavancin, and more frequently were PWID. Uncomplicated BSI patients more frequently had SSTI as the source of infection, more Streptococcus species in index culture, and shorter median BSI duration. Patients with complicated BSI started receiving dalbavancin at a median of 15 days post-index culture, compared to 8 days post-index culture among patients with uncomplicated infections. Repeat dalbavancin doses were more frequently given for complicated BSI, which also led to longer durations of treatment. Primary and secondary outcomes were not significantly different between the two BSI types.
Discussion
To our knowledge, this is the largest real-world, multicenter study of dalbavancin use for Gram-positive BSI. Dalbavancin has recently become more accepted as an option for step-down therapy for BSI. Patients were more frequently PWID (40%) who received dalbavancin for BSI in this study compared to other recent single-center US studies examining dalbavancin for osteomyelitis, deep-seated infections, or Staphylococcus BSI [15, 17, 18]. The high proportion of PWID is demographically consistent with the average patient age in our series, along with the bimodal distribution of age centered on patients 30 and 60 years old (Fig. 1). Dalbavancin is used in the PWID population due to difficulties in discharge, placement, and the tendency to avoid central lines. Indeed, 34% of patients received dalbavancin because the patient could not be discharged with a PICC in our analysis. The pathogens targeted by dalbavancin were similar to European real-world studies, with Staphylococcus aureus being the most prevalent, and coagulase-negative Staphylococcus, Streptococcus spp., Enterococcus spp., and other pathogens less common [12, 13]. However, the higher proportion of MRSA in our real-world cohort compared to these previous studies reflects the high prevalence of PWID in urban US hospitals.
Our cohort also found a high proportion of complicated BSI treated with dalbavancin compared to other observational studies. The recommended length of therapy for uncomplicated BSI is 2 weeks, and 4 weeks for complicated BSI. Importantly, the median length of stay with dalbavancin use in our study was much shorter than the recommended durations of treatment for Gram-positive BSI. If patients had not received dalbavancin, then they may not have been able to be discharged due to complex discharge situations. Therefore, dalbavancin administration may have saved upwards of a median 5 inpatient days for uncomplicated BSI and a median 15 inpatient days for complicated BSI. Administration was timed primarily on the day of discharge (45%), next most prior to discharge which was likely inpatient (27%), and lastly received post-discharge or assumed outpatient (25%) or only treated outpatient/in clinics (2.6%). Reimbursement for drug administration in addition to saving inpatient hospital days may play a large role in the timing of administration. As expected, complicated BSI had numerically worse outcomes compared to uncomplicated BSI, although the difference was not statistically significant. This was likely the result of longer bacteremia durations, reflecting higher disease burden, difficult source control, and higher-risk patients. It should be noted that in both complicated and uncomplicated BSI, the majority of patients completed the planned duration of dalbavancin therapy.
Literature supports dalbavancin attaining adequate staphylococcal coverage for 5–8 weeks when using two 1500-mg doses 1 week apart, which adds heterogeneity to defining the “duration of dalbavancin coverage” that classically is thought to last 7–14 days [22,23,24,25]. While dalbavancin 1500 mg was most common for BSI (68%), the timing of subsequent doses was variable. Differences in institutional clinical preferences and experience may explain the variable dalbavancin regimens and their timings relative to discharge (Table 3), highlighting a possible need for further standardization. Another important consideration is whether the BSI is uncomplicated or complicated, as dalbavancin doses averaged more than two in complicated BSI (Table 5). Despite rather heterogeneous dosing regimens, outcomes were favorable with low rates of 90-day mortality, 90-day recurrence, 90-day infection-related readmission, and low adverse-event rates. In fact, most patients (70%) completed dalbavancin treatment without a negative outcome. Although, the all-cause 90-day readmission rate in this population may seem high at 27%, it is in line with other dalbavancin studies such as Molina et al., with 26.2% and Veve et al. with 26–32% 90-day all-cause readmission rates compared with standard of care [15, 18]. These readmission rates are likely due to the vulnerability of the study patient population that are diagnosed with these infections.
The results from our study can provide real-world context to compare against the upcoming results from the DOTS randomized controlled trial [29]. The DOTS study has begun recruitment to answer the clinical question of dalbavancin (1500 mg on day 1 and 1500 mg on day 8) against standard of care in complicated S. aureus BSI, after blood culture clearance. Results are anticipated for this study some time in 2023–2024 [29, 30]. The positive outcomes on 90-day mortality, 90-day recurrence, 90-day infection-related readmission, and low adverse events in our study all compare favorably to the standard of care intravenous arms in single-center retrospective studies and in smaller randomized controlled trials [11, 14, 15, 17, 18]. These data suggest that dalbavancin can theoretically save inpatient days of therapy and possibly have non-inferior outcomes compared with standard of care, but more rigorous prospective randomized trials are needed. Even though our study did not have a comparator arm, smaller observational studies and randomized controlled trials have shown similar success rates to our own, as well as similar success rates to standard of care intravenous antibacterials [11, 14, 15, 17, 18].
This study has several limitations. First, it was a retrospective study that captured data mostly from large academic centers, which may not be applicable to smaller community hospitals, especially given the high cost of dalbavancin. Second, there was no comparator group. Third, some patients were lost to follow-up leading to missing values. This is particularly important given the concern for development of drug-resistant isolates over time, due to the long half-life of dalbavancin resulting in potentially sub-inhibitory concentrations for long periods of time. Investigators have documented at least four cases of resistance to dalbavancin, and this remains a concern for real-world practice [31,32,33,34]. However, no rise in dalbavancin or vancomycin MIC was noted in our study, although only seven isolates were available in 1 year of isolate follow-up. Lastly, certain data were not consistently available, such as any information on reimbursement or specific locations for dalbavancin administration, whether in an infusion center or inpatient.
Conclusions
In summary, dalbavancin appears to offer a viable antimicrobial disposition option for the outpatient management of Gram-positive BSI. More rigorous prospective trials will be needed to definitively offer practice-changing evidence adopting dalbavancin in the treatment of Gram-positive BSI. Further randomized-controlled trials are needed to clarify: (a) optimal clinical scenarios for use of dalbavancin, (b) ideal dosing and duration of treatment and (c) the extent towards possible development of resistance to vancomycin and/or dalbavancin.
Data Availability
The data sets during and/or analyzed during the current study are available from the corresponding author on reasonable request via a data use agreement from all contributing data collection sites.
References
Cooper GL, Given DB. Vancomycin: a comprehensive review of 30 years of clinical experience. Park Row Publishing Incorporated A Wiley and Sons Medical Group Comp; 1986.
Ramos-Otero GP, Sarangarm P, Walraven C. A retrospective analysis of intravenous vs oral antibiotic step-down therapy for the treatment of uncomplicated streptococcal bloodstream infections. J Clin Pharmacol. 2022. https://doi.org/10.1002/jcph.2097.
Al-Hasan MN, Rac H. Transition from intravenous to oral antimicrobial therapy in patients with uncomplicated and complicated bloodstream infections. Clin Microbiol Infect. 2020;26(3):299–306.
Li HK, Rombach I, Zambellas R, et al. Oral versus intravenous antibiotics for bone and joint infection. N Engl J Med. 2019;380(5):425–36.
Iversen K, Ihlemann N, Gill SU, et al. Partial oral versus intravenous antibiotic treatment of endocarditis. N England J Med. 2019. https://doi.org/10.1056/NEJMoa1808312.
Krsak M, Morrisette T, Miller M, et al. Advantages of outpatient treatment with long-acting lipoglycopeptides for serious gram-positive infections: a review. Pharmacotherapy. 2020;40(5):469–78.
Agarwal R, Bartsch SM, Kelly BJ, et al. Newer glycopeptide antibiotics for treatment of complicated skin and soft tissue infections: systematic review, network meta-analysis and cost analysis. Clin Microbiol Infect. 2018;24(4):361–8.
Boucher HW, Wilcox M, Talbot GH, Puttagunta S, Das AF, Dunne MW. Once-weekly dalbavancin versus daily conventional therapy for skin infection. N Engl J Med. 2014;370(23):2169–79.
Bryson-Cahn C, Beieler A, Chan J, Senter S, Harrington R, Dhanireddy S. A little bit of dalba goes a long way: dalbavancin use in a vulnerable patient population. Open Forum Inf Dis. 2017;4(1):336–7.
Gatti M, Andreoni M, Pea F, Viale P. <p>real-world use of dalbavancin in the era of empowerment of outpatient antimicrobial treatment: a careful appraisal beyond approved indications focusing on unmet clinical needs</p>. DDDT. 2021;15:3349–78.
Gonzalez PL, Rappo U, Akinapelli K, McGregor JS, Puttagunta S, Dunne MW. Outcomes in patients with Staphylococcus aureus bacteremia treated with dalbavancin in clinical trials. Infect Dis Ther. 2022;11(1):423–34.
Wunsch S, Krause R, Valentin T, et al. Multicenter clinical experience of real life Dalbavancin use in gram-positive infections. Int J Infect Dis. 2019;81:210–4.
Hidalgo-Tenorio C, Vinuesa D, Plata A, et al. DALBACEN cohort: dalbavancin as consolidation therapy in patients with endocarditis and/or bloodstream infection produced by gram-positive cocci. Ann Clin Microbiol Antimicrob. 2019;18:30.
Rappo U, Puttagunta S, Shevchenko V, et al. Dalbavancin for the treatment of osteomyelitis in adult patients: a randomized clinical trial of efficacy and safety. Open Forum Inf Dis. 2019. https://doi.org/10.1093/ofid/ofy331.
Veve MP, Patel N, Smith ZA, Yeager SD, Wright LR, Shorman MA. Comparison of dalbavancin to standard of care for outpatient treatment of invasive Gram-positive infections. Int J Antimicrob Agents. 2020. https://doi.org/10.1016/j.ijantimicag.2020.106210.
Tobudic S, Forstner C, Burgmann H, et al. Dalbavancin as primary and sequential treatment for gram-positive infective endocarditis: 2-year experience at the general hospital of Vienna. Clin Infect Dis. 2018;67(5):795–8.
Antosz K, Al-Hasan MN, Lu ZK, et al. Clinical utility and cost effectiveness of long-acting lipoglycopeptides used in deep-seated infections among patients with social and economic barriers to care. Pharmacy. 2022;10(1):1.
Molina KC, Lunowa C, Lebin M, et al. Comparison of sequential dalbavancin to standard-of-care treatment for Staphylococcus aureus bloodstream infections. Open Forum Inf Dis. 2022. https://doi.org/10.1093/ofid/ofac335.
Evins C, Lancaster H, Schnee AE. Successful use of dalbavancin in the treatment of gram positive blood stream infections: a case series. Ann Clin Microbiol Antimicrob. 2022;21:16.
Raad I, Darouiche R, Vazquez J, et al. Efficacy and safety of weekly dalbavancin therapy for catheter-related bloodstream infection caused by gram-positive pathogens. Clin Infect Dis. 2005;40(3):374–80.
AbbVie (2022) Phase 2, Open-label, randomized, multicenter study to compare the efficacy and safety of dalbavancin to standard of care antibiotic therapy for the completion of treatment of patients with complicated bacteremia or documented infective endocarditis. clinicaltrials.gov
Dunne MW, Puttagunta S, Sprenger CR, Rubino C, Van Wart S, Baldassarre J. Extended-duration dosing and distribution of dalbavancin into bone and articular tissue. Antimicrob Agents Chemother. 2015;59(4):1849–55.
Cojutti PG, Rinaldi M, Zamparini E, et al. Population pharmacokinetics of dalbavancin and dosing consideration for optimal treatment of adult patients with Staphylococcal osteoarticular infections. Antimicrob Agents Chemother. 2021;65(5):e02260-e2320.
Baklouti S, Marolleau S, Chavanet P, Bonnet E, Concordet, Gandia P (2021) Letter to the Editor on: “Population pharmacokinetics of dalbavancin and dosing considerations for optimal treatment of adult patients with Staphylococcal osteoarticular Infections”. Antimicrob Agents Chemother. Published online October 18, 2021:AAC.01493-21
Cooper MM, Preslaski CR, Shihadeh KC, Hawkins KL, Jenkins TC. Multiple-dose dalbavancin regimens as the predominant treatment of deep-seated or endovascular infections: a scoping review. Open Forum Inf Dis. 2021. https://doi.org/10.1093/ofid/ofab486.
Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52(3):e18–55.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Eaton EF, Westfall AO, McClesky B, et al. In-hospital illicit drug use and patient-directed discharge: barriers to care for patients with injection-related infections. Open Forum Inf Dis. 2020;7(3):074.
Turner NA, Zaharoff S, King H, et al. Dalbavancin as an option for treatment of S. aureus bacteremia (DOTS): study protocol for a phase 2b, multicenter, randomized, open-label clinical trial. Trials. 2022;23:407.
National Institute of Allergy and Infectious Diseases (NIAID) (2021) Dalbavancin as an option for treatment of S. aureus bacteremia (DOTS): a phase 2b, multicenter, randomized, open-label, assessor-blinded superiority study to compare the efficacy and safety of dalbavancin to standard of care antibiotic therapy for the completion of treatment of patients with complicated S. aureus Bacteremia. clinicaltrials.gov
Steele JM, Seabury RW, Hale CM, Mogle BT. Unsuccessful treatment of methicillin-resistant Staphylococcus aureus endocarditis with dalbavancin. J Clin Pharm Ther. 2018;43(1):101–3.
Werth BJ, Jain R, Hahn A, et al. Emergence of dalbavancin non-susceptible, vancomycin-intermediate Staphylococcus aureus (VISA) after treatment of MRSA central line-associated bloodstream infection with a dalbavancin- and vancomycin-containing regimen. Clin Microbiol Infect. 2018;24(4):429.e1-429.e5.
Kussmann M, Karer M, Obermueller M, et al. Emergence of a dalbavancin induced glycopeptide/lipoglycopeptide non-susceptible Staphylococcus aureus during treatment of a cardiac device-related endocarditis. Emerg Microbes Infect. 2018;7:202.
Zhang R, Polenakovik H, Barreras Beltran IA, et al. Emergence of dalbavancin, vancomycin, and daptomycin non-susceptible Staphylococcus aureus in a patient treated with dalbavancin: case report and isolate characterization. Clinl Inf Dis. 2022. https://doi.org/10.1093/cid/ciac341.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work, and have given their approval for this version to be published. Nicholas Rebold contributed to the concept and design, recruitment of sites/co-investigators, statistical analysis and drafting the and revising the final manuscript, Sara Alosaimy contributed to the concept and design, recruitment of sites and co-investigators, editing and revising the final manuscript, Jeffrey C. Pearson, Brandon Dionne, Ahmad Taqi, Mark Biagi, Nicholas Lombardo, Joshua Eudy, Daniel T. Anderson, Monica V. Mahoney, Wesley D. Kufel, Joseph A. D’Antonio, Bruce M. Jones, Jeremy J. Frens, Tyler Baumeister, Matthew Geriak, George Sakoulas, Dimitrios Farmakiotis, Dino Delaportas, Jeremy Larew and Michael P. Veve contributed to data collection and manuscript editing and revisions, Abdalhamid Lagnf, Kristen Lucas contributed to data collection, cleaning and editing and revision of final manuscript, Michael J. Rybak contributed to the concept and design, data analysis, overall supervision of the development of the paper and editing and revisions of the final manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
Nicholas Rebold, Jeffery C. Pearson, Brandon Dionne, Ahmad Taqi, Abdalhamid Lagnf, Kristen Lucas, Mark Biagi, Nicholas Lombardo, Joshua Eudy, Daniel T. Anderson, Joseph A. D’Antonio, Jeremy J Frens, Tyler Baumeister, Matthew Geriak, Dino Delaportas, Jeremy Larew, and Michael P. Veve have no conflicts of interest to report. Sara Alosaimy is a current employee of Seres Therapeutics. Monica V. Mahoney has received funds for research from Merck; consulting funds from Cidara, Melinta, Merck, Pfizer, Qpex, and Spero; speaker honoraria from Paratek. Wesley D. Kufel has received research grants from Merck and Melinta; served on the advisory board for Theratechnologies, Inc.; Bruce M. Jones has received funds for consulting or participated in speaking bureaus for AbbVie, Melinta, Merck, Paratek, and La Jolla. George Sakoulas has consulted for Octapharma, AbbVie, and Paratek Pharmaceuticals and is on the speakers bureau for AbbVie and Paratek Pharmaceuticals. Dimitrios Farmakiotis has received research support from Astellas, Viracor and Merck, and consultation fee from Viracor. Michael J. Rybak has received funds for research and consulting or participated in speaking bureaus for AbbVie, Ferring, Melinta, Merck, Paratek Pharmaceuticals, Shionogi, Spero, La Jolla, and T2 Bioscience and was/is partially supported by National Institute of Allergy and Infectious Diseases R01 AI121400 and R21 AI163726. Michael J. Rybak is Editor in Chief of Infectious Diseases and Therapy. Michael J. Rybak was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Ethical Approval
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. Approval was obtained from Wayne State University (#012019MP2E), Henry Ford Hospital (#14715), and all of the contributing medical centers with a waiver for informed consent due to the retrospective nature of the study design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Rebold, N., Alosaimy, S., Pearson, J.C. et al. Dalbavancin Sequential Therapy for Gram-Positive Bloodstream Infection: A Multicenter Observational Study. Infect Dis Ther 13, 565–579 (2024). https://doi.org/10.1007/s40121-024-00933-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-024-00933-2