Abstract
Background
Guillain-Barré syndrome (GBS) is an acute inflammatory neuropathy. The Erasmus GBS Respiratory Insufficiency Score (EGRIS) and the modified Erasmus GBS Outcome Score (mEGOS) are prognostic models used in the prediction of mechanical ventilation and outcome. Thus far, there are only few biomarkers for the prognosis prediction of GBS patients, and albumin level is one that is promising.
Methods
Patients diagnosed with GBS from 2013 to 2022 at Renmin Hospital, Wuhan University, China, were included. Patients hospitalized between 2016 and 2022 underwent short- and long-term follow-ups. The correlations between EGRIS/mEGOS and mechanical ventilation and outcome were evaluated. Serum albumin level was examined the day after admission. Furthermore, we also investigated whether the level of serum albumin was useful in predicting disease severity or poor outcome.
Results
In all, 145 patients were enrolled. Nineteen patients (13.1%) who required mechanical ventilation had higher Hughes GBS disability score (HGDS) at admission and discharge (P < 0.05 and P < 0.0001, respectively), shorter time from onset to admission and treatment (P < 0.01 and P < 0.001, respectively) and longer hospital stays (P < 0.001) than patients who did not require mechanical ventilation. High EGRIS scores were linked with the need for mechanical ventilation (r = 0.427, P < 0.001, AUC = 0.623). Seventy-one patients were admitted between 2016 and 2022. Of these, 65 patients had a 4-week follow-up and 61 had a 6-month follow-up. Higher mEGOS scores at admission and 7 days after admission significantly correlated with short- (P < 0.0001 and P < 0.0001) and long-term (P < 0.05 and P < 0.05) outcomes, respectively. No significant difference in outcome was found between different subtypes (4 weeks [P = 0.099] and 6 months [P = 0.172]). Patients with lower albumin level tended to have higher HGDS (at admission P < 0.05, at nadir P < 0.001, and at discharge P < 0.001) and higher properties of the need of mechanical ventilation (P < 0.05) and ICU stay (P < 0.05) than those with normal albumin levels. Those with low albumin levels were also unable to walk independently at 6 months (P < 0.01).
Conclusions
mEGOS scores predicted the outcomes of GBS patients in China, and EGRIS score predicted the need for mechanical ventilation in these patients. Albumin level at admission correlated well with disease severity and outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
GBS is an acute peripheral neuropathy with a 5% mortality; 20% patients need mechanical ventilation, while one-third remain unable to walk independently after 6 months of disease onset |
Early recognition of the need of mechanical ventilation and prognostic factors of poor outcome are important for GBS patients |
Prognostic models of GBS were developed based on patients in western countries, but the validity of these models in Chinese patients remains unclear |
We found EGRIS and mEGOS were good prognostic models for GBS patients in China and surprisingly found no difference between subtypes and outcomes |
Albumin level could be a good biomarker for the prediction of disease severity and outcomes in GBS |
Introduction
Guillain-Barré syndrome (GBS) is an acute inflammatory neuropathy that has various subtypes and outcomes [1,2,3]. Most patients with GBS have a good prognosis. However, one-third remain unable to walk independently 6 months after disease onset, and about 5% die of respiratory failure or other complications [1, 2, 4, 5]. Several indicators have been correlated with a poor GBS disease outcome, including preceding diarrhea, hyponatremia, need for mechanical ventilation (MV) and axonal type electrodiagnosis [4, 6,7,8,9]. Early recognition of patients who are at a high risk of a poor outcome can help direct personalized management.
The Erasmus GBS Respiratory Insufficiency Score (EGRIS) was developed in 2012 to predict the need for MV in GBS patients within the first week of hospital admission [10]. Time from disease onset to admittion, facial and/or bulbar weakness and Medical Research Council (MRC) sum score are included in EGRIS. A higher EGRIS score is predictive of a higher risk of respiratory failure. The modified Erasmus GBS Outcome Score (mEGOS) is used to predict the ability of a GBS patient to walk independently 6 months after disease onset. Age, preceding diarrhea and muscle strength are the components of this score, which ranges from 0 to 9 at admission and from 0 to 12 a week after admission [7].
Thus far, only a few biomarkers have been proved to be effective to predict the prognosis of GBS patients. Neurofilament light protein levels, glial fibrillary acidic protein and neurofilaments were shown to be associated with the outcomes of GBS patients [11,12,13], but all of these biomarkers require special examinations and cannot be easily measured in standard clinical settings.
Albumin is an easily detected serum biomarker. Albumin level is influenced by various physiological factors and directly decreases with age [14]. Low albumin level after intravenous immunoglobulin (IVIg) treatment was shown to be associated with poor outcomes. However, whether albumin can be an early biomarker for GBS prediction still needs further investigation.
The EGRIS and mEGOS have been shown to be useful in many countries such as Japan, Europe, North America, Malaysia and Bangladesh [7, 15,16,17,18]. While its efficacy has been demonstrated in pediatric patients in China, it has not been evaluated on adult Chinese patients. We sought to predict the value of these two models in Chinese adult patients with GBS.
Methods
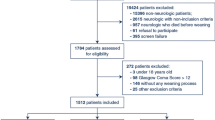
The study admitted patients diagnosed with GBS from 2013 to 2022 in Renmin Hospital. Classical GBS was confirmed using the criteria set forth by Asbury and Cornblath [19], and Miller-Fisher syndrome (MFS) was diagnosed according to the new diagnostic classification [20]. The exclusion criteria for the outcome study were age < 18 years and a hospitalization time of < 7 days. Age, sex, preceding events, time from onset to nadir/admission, cranial nerve involvement, time from onset to treatment, Medical Research Council sum score at admission and 1 week, Hughes GBS disability score (HGDS) at admission/nadir/discharge/follow-up, laboratory examinations and nerve conduction study findings were collected. Albumin level was examined the day after admission and before the start of immunotherapies. Subtypes of patients with GBS were classified according to the criteria that were widely accepted [21,22,23]. The detailed diagnostic criteria are shown in Supplementary Table 1. The HGDS was used to evaluate the walking ability of GBS patients at admission, nadir, discharge and follow-up [24]. The MRC sum score was evaluated at admission and 1 week after admission. The HGDS and MRC sum score were assessed separately by two investigators. Nadir was defined as the highest GBS disability score over the disease course. A poor outcome was defined as the inability to walk independently or a GBS disability score of > 2 points. Low albumin level was defined as < 40 g/l. Patients admitted between 2016 and 2022 participated in the follow-ups.
Missing data were eliminated from the analysis for non-outcome variables, which meant that if a patient missed the follow-up records at 6 months, their data would not be used to analyze the relationship between the outcome at 6 months and the variables.
This retrospective study was approved by the ethics committee of the Renmin Hospital of Wuhan University, Wuhan, China (WDRY2023-K012). This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
All statistical analyses were performed using IBM SPSS V.23 (Armonk, NY, USA). Categorical variables were evaluated using the chi-squared test, and continuous variables were described as the mean and SD, with comparisons performed using Student’s t-test for normally distributed data and a non-parametric test for non-normally distributed data. The Mann-Whitney U test was used to compare the HGDS and MRC sum score. Spearman and Pearson’s correlation tests were used to evaluate the correlation between HGDS and mEGOS/EGRIS. Receiver-operating characteristic (ROC) curve analysis was performed to assess the predictive ability of each variable. A two-sided P value < 0.05 was considered to indicate statistically significant differences.
Results
A total of 145 patients were included in our study. Briefly, 85 (58.62%) patients were male and 60 (41.38%) were female, yielding a male-to-female ratio of 1.4; The median age was 54 (44–66) years. Seventy-six patients had preceding events, of whom 40 (52.63%) had an upper respiratory tract infection (UTRI) and 11 (14.47%) had diarrhea. One hundred seven (73.79%) patients received immunotherapy (Table 1).
In the study, 19 patients required MV during the disease course. Age, sex, UTRI and cranial nerve involvement (CNI) at admission showed no difference between patients that required MV and those that did not. IVIg was administered to most patients who required MV, and the hospital stay was significantly longer in those who required MV (P = 0.0005, Table 2). Patients requiring MV had higher HGDS at admission and discharge (at admission P < 0.05 and at discharge P < 0.0001, Fig. 1A), and the time from onset to admission or treatment was significantly shorter in patients who required MV (admission P < 0.01 and treatment P < 0.001, Fig. 1B). Fifteen patients who required MV within 7 days of admission had a mean EGRIS score of 4.1 ± 1.8, which was higher than the scores of patients who did not require MV (2.3 ± 1.5) (P = 0.0002, Fig. 2). Correlation analysis showed that higher EGRIS scores were significantly linked to disease severity as evaluated by the GBS disability score 7 days after admission (r = 0.427, P < 0.001, AUC = 0.623). Four patients required MV 7 days after admission.
Comparison between patients requiring mechanical ventilation and not requiring mechanical ventilation in GBS. A HGDS scores were higher in the MV group than in the non-MV group at admission (3.3 ± 1.1 vs. 2.7 ± 1.3, P = 0.026) and discharge (4.0 ± 1.2 vs. 1.9 ± 1.3, P < 0.0001). B Time from disease onset to admission (4.9 ± 4.7 vs. 8.6 ± 7.5, P = 0.0079) and treatment (5.7 ± 6.2 vs. 11.1 ± 8.8, P = 0.0003) was shorter in the MV group than in the non-MV group. *P < 0.05, ***P < 0.001, **P < 0.01, ****P < 0.0001
A total of 71 patients were admitted between 2016 and 2022. Sixty-five patients underwent a 4-week follow-up; six patients were not accessible or refused follow-up. Sixty-one underwent a 6-month follow-up, two did not reach the follow-up time, two died of other diseases (one each of stroke and psychological disorder), and six refused follow-ups. Patients with poor outcome 4 weeks after disease onset had a higher mEGOS at admission (r = 0.543, P = 0.000, AUC = 0.655) and on day 7 (r = 0.579, P = 0.000, AUC = 0.665) (Table 3). Twenty-five (38%) patients were unable to walk independently at 4 weeks, and the mEGOS scores at admission and day 7 were significantly higher in patients with poor outcome (5.1 ± 2.2 vs. 2.4 ± 1.7, P < 0.0001 and 7.4 ± 3.6 vs. 3.1 ± 3.1, P < 0.0001) than in those without. Patients with poor outcomes 6 months after disease onset had higher mEGOS scores at admission (r = 0.438, P < 0.01, AUC = 0.791) and day 7 (r = 0.506, P < 0.01, AUC = 0.802) (Fig. 3A, B). Eight (13.11%) patients were unable to walk independently at 6 months, and the mEGOS scores at admission and day 7 were significantly higher in patients with poor outcomes (5.0 ± 2.1 vs. 3.1 ± 2.2, P < 0.05 and 7.9 ± 3.2 vs. 4.3 ± 3.7, P < 0.05) (Fig. 3C, D).
Modified Erasmus GBS Outcome Score (mEGOS) at admission and day 7 in the study. Patients with poor outcomes 4 weeks after admission had higher mEGOS scores at admission and day 7 than those with good outcomes (A and B). Patients with poor outcomes 6 months after admission had higher mEGOS scores at admission and day 7 than those with good outcomes (C and D), *P < 0.05, ****P < 0.0001
Fifty-eight of the 68 classical GBS patients in the study underwent nerve conduction study (NCS). Twenty-two (37.93%) had the demyelinating subtype while 21 (36.21%) had the axonal subtype. There was no significant difference in outcome between the different subtypes (4-week follow-up, P = 0.099; 6-month follow-up, P = 0.172). Three patients were diagnosed with MFS, all of whom had good outcomes at 4 weeks and 6 months.
Patients with low serum albumin level were slightly older than those with normal albumin level, but this difference was not significant (Table 4). Higher HGDS at admission, nadir and discharge were found in patients with low albumin levels (at admission P < 0.05, at nadir P < 0.001 and at discharge P < 0.001). Patients with low albumin levels had higher rate of MV and ICU admission. No significant difference was found between patients with low or normal albumin levels in sex, preceding events and CNI at admission.
Fifty-nine patients with follow-ups had data on albumin levels. Poor outcome at 6 months was also associated with lower albumin level (40.5 ± 3.6 vs. 35.4 ± 3.3, P < 0.01) (Fig. 4A). Liner regression analysis showed that lower albumin level was significantly associated with higher HGDS scores in GBS patients (r = − 0.316, P < 0.05) (Fig. 4B).
Discussion
This study evaluated the use of the mEGOS and EGRIS scoring systems in patients diagnosed with GBS, regardless of subtypes and disease severity. The study showed that high mEGOS scores correlated with poor outcome 4 weeks and 6 months after disease onset. Such findings were useful for both patients who were unable to walk independently at admission and those with less severe symptoms. The mEGOS score was previously validated in Japan, Malaysia, Bangladesh and the IGOS group [15,16,17, 25]. All validation studies identified a significant correlation between mEGOS score at admission and day 7 with the 6-month outcome. A study of Chinese children also found that mEGOS scores were helpful indicators of clinical outcome 6 months after disease onset [18]. The findings of the present work indicate that the mEGOS may be useful to predict the outcome of adult GBS patients in China.
The AUC values for the mEGOS ranged from 0.66 to 0.80 in the study. A Malaysian study reported AUCs of 0.85–0.92 at 4 weeks, which is higher than the values reported in our study, and of 0.69–0.78 at 6 months [17]. The AUC value for the mEGOS in Chinese pediatric patients was previously found to be 0.78–0.88, suggesting better predictability of the mEGOS in children than adults [18]. The proportion of patients who could walk independently at 6 months was 88%, which is similar to the findings of a Japanese study (89%) [15] and higher than the results found in a Malaysian study (69%) [17]. Ninety-five percent of children could walk independently after 6 months, indicating better GBS outcomes in children compared than adults [18].
Previous studies concluded that age, sex and facial nerve paralysis could not be predicting factors of MV in GBS [26]; our study showed similar results. Time from disease onset to admission and limb weakness were regarded as risk factors for MV and shorter time or lower MRC score mean higher risk of MV for GBS patients [6, 10, 27]. In our study, patients requiring MV showed significantly shorter time from onset to admission and treatment, and higher HGDS scores at admission and discharge were also found in mechanically ventilated patients.
EGRIS was significantly higher in patients who needed MV in our study. A total of seven patients required MV during their care, and those requiring MV during the disease course had significantly higher EGRIS scores. Our findings are in line with those from studies in Japan, Malaysia and Jilin Province in China [15, 17, 28]. Clinicians should be alert for the early signs of respiratory failure and prepare for MV of patients with EGRIS ≥ 5.
The axonal subtype of GBS has been considered to be predictive of a poor outcome [27, 29,30,31,32], while the demyelinating subtype was predictive of MV [33]. Our study found no differences in outcomes of patients with demyelinating or axonal GBS, which is consistent with the findings of similar studies from Malaysia and Japan, but differs from that of an American study. A possible cause for this disagreement is that the number of patients with axonal damage was too small to permit the measurement of a significant difference. Further large-scale studies are needed to validate correlations between subtypes and outcomes.
Albumin level was a promising biomarker for early judgment of disease severity and outcome of GBS. Our study showed that patients with low albumin level had higher HGDS at admission, nadir and discharge. Furthermore, the albumin level and HGDS scores were negatively correlated. Patients with low albumin level had higher percentage of ICU admission and MV. Since it is a retrospective study, the albumin level was not exact in some patients without follow-ups. Some medical records only contained a description of albumin level declaring that it is normal in this patient, but did not provide the exact figure, but patients with abnormal albumin levels were all provided the exact level of albumin, so the average serum albumin of the entire population could not be calculated because of the significant bias. Another previous study showed that hypoalbuminemia after IVIg was related to a more severe clinical course and poorer outcome, and the serum albumin level at 2 weeks after treatment correlated with clinical recovery [34]. A case report in 2020 also advised serum albumin level as a biomarker for the decision regarding the second course of IVIg [35]. Our study showed that the albumin level at admission is a good biomarker for disease severity and outcome of GBS; moreover, patients with low albumin level attained higher HGDS scores at admission and nadir and showed poorer outcome after 6 months. The reasons why serum albumin level decreased in GBS patients is still unclear. Hypoalbuminemia can be attributed to three basic reasons, the increase of loss or breakdown, dilution and decrease of synthesis [36]. Serum albumin was detected at the 2nd day after admission, before the immunotherapies started; thus, we excluded the influences of IVIg or other therapies. Albumin is synthesized in the liver; hence, liver disease, inflammation and infections can influence the synthesis of albumin. The underlying inflammatory reactions in GBS and/or co-infections with GBS likely reduce albumin synthesis. Albumin level decreases with advancing age, and older age is a risk factor for GBS patients with poor outcomes. The comorbidities can influence the prognosis of GBS patients, but even if the hypoalbumin was caused by the comorbidities, the low albumin level was still associated with disease severity and outcomes. A prospective study is needed to further evaluate why the albumin level decreased and how it influences disease severity in GBS.
Although the patients with hypoalbumin showed no significant differences in hospitalization stay, the higher disability scores and higher percentage of the requirement of MV and ICU still show the predicting value of albumin. Serum albumin is an easy and early accessible biomarker for every hospital; although patients requiring MV had longer hospital stays, MV as a marker for predicting disease severity and outcomes came up too late for GBS patients. Early recognition of disease severity and outcome can help patients get medical care in time.
Our study has some limitations. The sample size was small for an outcome study. Despite this, we still found significant correlations of outcomes and mEGOS scores and found that mEGOS and EGRIS scores were useful in GBS patients in China. Second, some patients refused their 6-month follow-up visit, resulting in missing data. A prospective, multicenter, large-scale study that includes both children and adults is needed for further analysis.
In conclusion, mEGOS scores are useful to predict the short- and long-term outcomes of GBS patients, and EGRIS score is helpful at identifying patients who may progress to respiratory failure. Albumin level at admission was well correlated with disease severity and outcomes. Future large-scale studies researching biomarkers that correlate with disease severity are still needed.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Shahrizaila N, Lehmann HC, Kuwabara S. Guillain-Barré syndrome. Lancet. 2021;397(10280):1214–28.
van Doorn PA, Ruts L, Jacobs BC. Clinical features, pathogenesis, and treatment of Guillain-Barré syndrome. Lancet Neurol. 2008;7(10):939–50.
Doets AY, Verboon C, van den Berg B, Harbo T, Cornblath DR, Willison HJ, et al. Regional variation of Guillain-Barré syndrome. Brain. 2018;141(10):2866–77.
Rajabally YA, Uncini A. Outcome and its predictors in Guillain-Barre syndrome. J Neurol Neurosurg Psychiatry. 2012;83(7):711–8.
Willison HJ, Jacobs BC, van Doorn PA. Guillain-Barré syndrome. Lancet. 2016;388(10045):717–27.
Arami MA, Yazdchi M, Khandaghi R. Epidemiology and characteristics of Guillain-Barré syndrome in the northwest of Iran. Ann Saudi Med. 2006;26(1):22–7.
Walgaard C, Lingsma HF, Ruts L, van Doorn PA, Steyerberg EW, Jacobs BC. Early recognition of poor prognosis in Guillain-Barre syndrome. Neurology. 2011;76(11):968–75.
Strauss J, Aboab J, Rottmann M, Porcher R, Polito A, Ikka L, et al. Plasma cortisol levels in Guillain-Barré syndrome. Crit Care Med. 2009;37(8):2436–40.
Kuwabara S, Mori M, Ogawara K, Hattori T, Yuki N. Indicators of rapid clinical recovery in Guillain-Barré syndrome. J Neurol Neurosurg Psychiatry. 2001;70(4):560–2.
Walgaard C, Lingsma HF, Ruts L, Drenthen J, van Koningsveld R, Garssen MJ, et al. Prediction of respiratory insufficiency in Guillain-Barré syndrome. Ann Neurol. 2010;67(6):781–7.
Axelsson M, Sjögren M, Andersen O, Blennow K, Zetterberg H, Lycke J. Neurofilament light protein levels in cerebrospinal fluid predict long-term disability of Guillain-Barré syndrome: a pilot study. Acta Neurol Scand. 2018;138(2):143–50.
Notturno F, Caporale CM, De Lauretis A, Uncini A. Glial fibrillary acidic protein: a marker of axonal Guillain-Barrè syndrome and outcome. Muscle Nerve. 2008;38(1):899–903.
Petzold A, Hinds N, Murray NM, Hirsch NP, Grant D, Keir G, et al. CSF neurofilament levels: a potential prognostic marker in Guillain-Barré syndrome. Neurology. 2006;67(6):1071–3.
Chiò A, Calvo A, Bovio G, Canosa A, Bertuzzo D, Galmozzi F, et al. Amyotrophic lateral sclerosis outcome measures and the role of albumin and creatinine: a population-based study. JAMA Neurol. 2014;71(9):1134–42.
Yamagishi Y, Suzuki H, Sonoo M, Kuwabara S, Yokota T, Nomura K, et al. Markers for Guillain-Barré syndrome with poor prognosis: a multi-center study. J Peripher Nerv Syst. 2017;22(4):433–9.
Papri N, Doets AY, Mohammad QD, Endtz HP, Lingsma HF, Jacobs BC, et al. Validation and adjustment of modified Erasmus GBS outcome score in Bangladesh. Ann Clin Transl Neurol. 2022;9(8):1264–75.
Tan CY, Razali SNO, Goh KJ, Shahrizaila N. The utility of Guillain-Barré syndrome prognostic models in Malaysian patients. J Peripher Nerv Syst. 2019;24(2):168–73.
Qinrong H, Yuxia C, Ling L, Huayu L, Lei X, Xiaoli L, et al. Reliability and validity of prognostic indicators for Guillain-Barré syndrome in children. Dev Med Child Neurol. 2022;65(4):563–70.
Asbury AK, Cornblath DR. Assessment of current diagnostic criteria for Guillain-Barré syndrome. Ann Neurol. 1990;27(Suppl):S21–4.
Wakerley BR, Uncini A, Yuki N. Guillain-Barré and Miller Fisher syndromes–new diagnostic classification. Nat Rev Neurol. 2014;10(9):537–44.
Ho TW, Mishu B, Li CY, Gao CY, Cornblath DR, Griffin JW, et al. Guillain-Barré syndrome in northern China. Relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain. 1995;118(Pt 3):597–605.
Hadden RD, Cornblath DR, Hughes RA, Zielasek J, Hartung HP, Toyka KV, et al. Electrophysiological classification of Guillain-Barré syndrome: clinical associations and outcome. Plasma Exchange/Sandoglobulin Guillain-Barré Syndrome Trial Group. Ann Neurol. 1998;44(5):780–878.
Hughes RA, Cornblath DR. Guillain-Barré syndrome. Lancet. 2005;366(9497):1653–66.
van Koningsveld R, Steyerberg EW, Hughes RA, Swan AV, van Doorn PA, Jacobs BC. A clinical prognostic scoring system for Guillain-Barré syndrome. Lancet Neurol. 2007;6(7):589–94.
Doets AY, Lingsma HF, Walgaard C, Islam B, Papri N, Davidson A, et al. Predicting outcome in Guillain-Barré syndrome: international validation of the modified Erasmus GBS outcome score. Neurology. 2022;98(5):e518–32.
Green C, Baker T, Subramaniam A. Predictors of respiratory failure in patients with Guillain-Barré syndrome: a systematic review and meta-analysis. Med J Aust. 2018;208(4):181–8.
Verma R, Chaudhari TS, Raut TP, Garg RK. Clinico-electrophysiological profile and predictors of functional outcome in Guillain-Barre syndrome (GBS). J Neurol Sci. 2013;335(1–2):105–11.
Cheng Y, Liu K, Li C, Zhang W, Wu X, Fang S. Risk factors for mechanical ventilation in patients with Guillain-Barré syndrome. Neurocrit Care. 2022;37(1):121–8.
Cornblath DR, Mellits ED, Griffin JW, McKhann GM, Albers JW, Miller RG, et al. Motor conduction studies in Guillain-Barré syndrome: description and prognostic value. Ann Neurol. 1988;23(4):354–9.
Group TIG-BS. The prognosis and main prognostic indicators of Guillain-Barré syndrome. A multicentre prospective study of 297 patients. The Italian Guillain-Barré Study Group. Brain. 1996;119(6):2053–25061.
Zhang G, Li Q, Zhang R, Wei X, Wang J, Qin X. Subtypes and Prognosis of Guillain-Barré Syndrome in Southwest China. PLoS One. 2015;10(7): e0133520.
González-Suárez I, Sanz-Gallego I, Rodríguez de Rivera FJ, Arpa J. Guillain-Barré syndrome: natural history and prognostic factors: a retrospective review of 106 cases. BMC Neurol. 2013;13:95.
Durand MC, Porcher R, Orlikowski D, Aboab J, Devaux C, Clair B, et al. Clinical and electrophysiological predictors of respiratory failure in Guillain-Barré syndrome: a prospective study. Lancet Neurol. 2006;5(12):1021–8.
Fokkink WR, Walgaard C, Kuitwaard K, Tio-Gillen AP, van Doorn PA, Jacobs BC. Association of albumin levels with outcome in intravenous immunoglobulin-treated Guillain-Barré syndrome. JAMA Neurol. 2017;74(2):189–96.
Shalman A, Savir S, Mechnik Steen Y, Ovanyan A, Boniel N, Koyfman L, et al. Albumin levels as a biomarker for second Intravenous Immunoglobulin (IVIG) treatment in Guillain-Barre syndrome (GBS). J Clin Neurosci. 2020;74:247–9.
Rothschild MA, Oratz M, Schreiber SS. Regulation of albumin metabolism. Annu Rev Med. 1975;26:91–104.
Acknowledgements
We thank the participants of the study. We are thankful to the clinicians from the Department of Neurology at Renmin Hospital of Wuhan University for their help with this study.
Medical Writing and Editorial Assistance
The authors thank Charlesworth Author Services (https://www.cwauthors.com) for English language editing and review services, which were funded by the authors.
Funding
This work was supported by grants from the Open Project of Key Laboratory of Hubei Province (2021KFY041); the project funded the study. The journal’s Rapid Service fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Jiajia Yao and Zuneng Lu provided the idea for the study, Rumeng Zhou, Yue Liu, Yin Liu and Qian Cao collected the clinical data, Jiajia Yao analyzed the data and wrote the manuscript. All authors read and approved the final version of the manuscript and agreed with its submission for publication.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical Approval
This study received approval from the institutional review board of Renmin Hospital of Wuhan University (WDRY2023-K012). Formal consent was not required because of the retrospective nature of this study. Since our study did not harm the patients without privacy exposure, and only analyzed baseline data and clinical outcomes, the informed consent form was waived. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yao, J., Zhou, R., Liu, Y. et al. Predicting of Mechanical Ventilation and Outcomes by Using Models and Biomarker in Guillain-Barré Syndrome. Neurol Ther 12, 2121–2132 (2023). https://doi.org/10.1007/s40120-023-00546-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-023-00546-w