Abstract
Introduction
β-Blockers are a heterogenous class of drugs that are no longer recommended for initial antihypertension monotherapy due to unfavorable long-term cardiovascular events observed with non-vasodilatory β-blockers. However, the comparative cardiovascular event risk between the vasodilatory β1-selective antagonist/β3 agonist nebivolol and non-vasodilatory β1-blockers, atenolol and metoprolol, is unknown.
Methods
Incident nebivolol, atenolol, or metoprolol monotherapy users with hypertension were identified using US claims data (2007–2014). The first β-blocker claim on/after 1/1/2008 defined the index drug/date. Hypertensive patients without pre-index cardiovascular history were followed until index drug discontinuation (> 90 day supply gap), use of other β-blockers, or end of continuous plan enrollment. Patients were pair-wise propensity score-matched using logistic regression, adjusted for baseline demographics, Charlson Comorbidity Index score, comorbid chronic pulmonary disease, rheumatic disease, renal disease, and diabetes, and use of other antihypertensive drugs during baseline. Time to first hospital claim for a cardiovascular event was assessed via Cox proportional hazards regression, adjusted for the variables above.
Results
Inclusion criteria were met by 81,402 patients (n = 27,134 in each matched treatment cohort), with no between-cohort differences in baseline characteristics, comorbid conditions, or average follow-up duration. Atenolol and metoprolol cohorts had greater risk of hospitalization for a composite event (myocardial infarction, angina, congestive heart failure, stroke) than nebivolol users (adjusted hazard ratios [95% confidence interval] atenolol: 1.68 [1.29, 2.17]; metoprolol: 2.05 [1.59, 2.63]; P < 0.001, both). Risks of most individual cardiovascular events were also lower with nebivolol, including myocardial infarction and angina versus atenolol, and myocardial infarction, congestive heart failure, and angina versus metoprolol (P < 0.05, all).
Conclusions
Nebivolol was associated with significantly lower risk of hospitalization due to composite cardiovascular events than atenolol or metoprolol in this large retrospective cohort study of monotherapy with three different β1-selective blockers in hypertensive patients.
Funding
Allergan plc, Madison, NJ, USA.
Similar content being viewed by others
Introduction
Hypertension is a major risk factor for cardiovascular (CV) morbidity and mortality [1], and antihypertensive drugs as a whole reduce that risk [2]. Questions remain, however, regarding the relative benefit of specific antihypertensive drugs or classes of drugs for preventing CV-related events, including myocardial infarction, congestive heart failure, stroke, and angina pectoris.
Several meta-analyses [3,4,5] and large randomized trials [6, 7] in hypertensive patients have shown that β-blockers do not reduce CV events to the extent of other antihypertensive drug classes. Such results prompted changes to the evidence-based guidelines for the management of high blood pressure in adults, with β-blockers no longer recommended as first-line antihypertensive treatments in the US [8]. Of note, the reports upon which the revised recommendations were based were non-vasodilatory β-blockers [9]. Similar studies on the effect of vasodilatory β-blockers (e.g., nebivolol and carvedilol) on CV-related events are lacking in hypertensive populations. Nebivolol—a β1-selective adrenergic blocker with β3 agonistic vasodilatory properties—may confer more protection against CV events than non-vasodilatory β-blockers through its unique mechanism of action: endothelium-dependent vasodilation via nitric oxide, decreased peripheral resistance, decreased myocardial contractility, and suppression of renin activity [10, 11].
Unlike atenolol, nebivolol does not increase the augmentation index (a measure of central blood pressure) [12], but increases cardiac stroke volume and decreases peripheral vascular resistance without reducing cardiac output [13]. Furthermore, nebivolol does not decrease heart rate to the same extent as atenolol [12, 13]. In addition to its cardiovascular effects, nebivolol has a tolerability profile similar to placebo (2.8% AE-related discontinuations for nebivolol vs. 2.2% placebo) [14] and better tolerability than several other antihypertensive drug classes, including other β-blockers [15]. Yet, little is known of the comparative effectiveness of monotherapy with nebivolol and two commonly prescribed non-vasodilatory β1-selective blockers, atenolol and metoprolol, in reducing CV event risks. The objective of this study was to compare the real-world risk of hospitalization due to a CV event in patients with uncomplicated hypertension receiving nebivolol, atenolol, or metoprolol monotherapy.
Methods
All study methods are described below or in the online-only Data Supplement.
Compliance with Ethics Guidelines
This study is based on de-identified data collected from a health care claims database and does not contain any studies with human participants or animals performed by any of the authors, therefore informed consent was not obtained.
Study Design and Patients
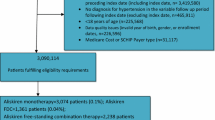
This was a retrospective claims analysis using data from IMS PharMetrics Plus™, a US national-level claims database comprising de-identified, HIPAA-compliant patient-level data. Patients with a diagnosis of hypertension (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM] codes 401.xx-405.xx) between January 1, 2007 and June 30, 2014 were identified. The index date and index drug were defined by the first claim for a β-blocker on or after January 1, 2008 (per National Drug Codes). Inclusion criteria were assessed during the baseline period, defined as the 6-month period prior to the index date (Fig. 1). Incident users of nebivolol, atenolol, or metoprolol with continuous plan enrollment during the baseline period were included. Any non-β-blocker antihypertensives taken during the baseline period were discontinued prior to the first β-blocker monotherapy claim. Key exclusion criteria included a history of CV disorders other than hypertension (e.g., myocardial infarction [MI]; congestive heart failure [CHF]; stroke; angina pectoris; coronary artery disease [CAD]; coronary artery bypass graft [CABG]; cardiovascular disease [CVD]; peripheral vascular disease [PVD]; percutaneous coronary intervention; angioplasty; or any heart rhythm or heart rate disorders) prior to the index date or use of non-index antihypertensive drugs during the follow-up period (Fig. 1; ICD-9 codes for the exclusion criteria are available at http://hyper.ahajournals.org). There was no minimum follow-up period; follow-up continued until discontinuation of the index drug (≥ 90 day gap in supply), a claim for non-index β-blockers, or the end of continuous plan enrollment, whichever came first.
Patient selection. aDiagnosis of hypertension was determined via ICD-9-CM codes 401.xx–405.xx. bCV events were defined as a primary or secondary diagnosis of MI, CHF, stroke, angina, CAD, CABG, percutaneous coronary intervention, angioplasty, CVD, PVD, ventricular arrhythmias, atrial fibrillation, supraventricular tachycardia or sinus tachycardia that occurred from 01/01/2007 to index date. CABG coronary artery bypass graft, CAD coronary artery disease, CHF congestive heart failure, CV cardiovascular, CVD cardiovascular disease, ICD-9-CM International Classification of Diseases, ninth revision, clinical modification, MI myocardial infarction, PVD peripheral vascular disease
Endpoints
The study endpoint was the risk of hospitalization due to a CV event during the follow-up period in patients with uncomplicated hypertension who newly initiated β-blocker monotherapy of nebivolol, atenolol, or metoprolol (determined via ICD-9-CM codes). Data were analyzed by hospitalizations due to individual CV events (MI, CHF, stroke, or angina pectoris) and due to a composite of CV events identified through inpatient claims with a principle diagnosis for any of the individual CV events. The ICD-9-CM codes used to identify MI were 410.xx and 412.xx; for CHF, the codes used were 428.xx, 402.01, 402.11, 402.91, 404.x1, and 404.x3; for stroke, 430.xx, 431.xx, 436.xx, 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, and 434.91; and for angina, 411.xx and 413.xx.
Statistical Analysis
The primary analysis consisted of propensity score-matching β-blocker cohorts using a pair-wise propensity score calculated via logistic regressions. Patients in the nebivolol cohort were 1:1 propensity matched two times: once to patients in the atenolol cohort and then again to those in the metoprolol cohort. Propensity matching was based on baseline demographics (age, sex, and geographical region; race was not included in the claims database), Charlson Comorbidity Index (CCI) score (a weighted index used to predict risk of death within 1 year of hospitalization in patients with certain comorbid diseases [16, 17]), diagnosis of comorbid chronic pulmonary disease, rheumatic disease, renal disease, and diabetes (per CCI), and use of other antihypertensive drugs during the baseline period. Additionally, the duration of the follow-up period was directly matched between cohorts. Balance between the cohorts was achieved via propensity score matching as determined by a standardized difference of < 0.1 at P > 0.05 for all variables included in the analysis. Time to first inpatient claim due to the composite CV event, as well as individual components of the composite, was assessed via multivariable Cox proportional hazards regression adjusting for the same covariates as those used in the propensity matching analysis. The hazard ratios (HR), 95% confidence interval (CIs), and statistical significance associated with the atenolol and metoprolol cohorts relative to nebivolol cohort were calculated.
The unadjusted incident rates of hospitalization due to the composite of CV event and its individual components were calculated as the number of patients with incident events divided by the total duration when the patients were at risk (per 1000 person-years). A 95% CI was calculated following Poisson distribution; the differences in incident rates were considered statistically significant if there was no overlap in 95% CIs. Analyses for this study were conducted using the Statistical Analysis System software (SAS; v 9.4) and Stata (v 12.0). All tests were two-tailed and conducted at a significance level of α < 0.05.
Results
A total of 185,374 patients met inclusion criteria (n = 29,300 in nebivolol; n = 58,279 in atenolol; n = 97,795 in metoprolol). After propensity score matching, 81,402 were included (n = 27,134 in each of the nebivolol, atenolol, and metoprolol cohorts). Patients in the nebivolol, atenolol, and metoprolol groups were an average of 49.0 (standard deviation: 10.4), 48.9 (10.8), and 49.0 (10.8) years of age, respectively and 52% were female; the average duration of follow-up ranged from 260.7 to 265.1 days. During the 6-month pre-index baseline period, 34% of patients had used non-β-blocker antihypertensives. There were no statistical differences in the baseline demographics, comorbid conditions, use of any antihypertensive drugs during the pre-index period, or average duration of follow-up between the nebivolol cohort and either the atenolol or metoprolol cohorts (Table 1).
After adjusting for baseline characteristics of the matched cohorts, the atenolol and metoprolol cohorts had a significantly greater risk of hospitalization due to a composite CV event (atenolol HR: 1.68 [95% CI: 1.29–2.17]; metoprolol: 2.05 [1.59–2.63]) vs. nebivolol (P < 0.001, both; Fig. 2). Atenolol and metoprolol users also had significantly increased risks of MI (1.82 [1.07–3.11]; 1.78 [1.04–3.06]) and angina (1.77 [1.19–2.64]; 2.74 [1.89–3.98]) vs. nebivolol (P < 0.05, all). CHF risk was significantly greater in the metoprolol cohort vs. nebivolol (2.26 [1.17–4.36]; P < 0.05); for atenolol users, the hazard ratio was 1.58 (0.79–3.18) compared with nebivolol, but did not reach statistical significance. While the point estimates for stroke risk were greater for atenolol (1.54 [0.90–2.64]) and metoprolol (1.15 [0.65–2.03]) than nebivolol users, the differences were not statistically significant (see Table S1 in the electronic Supplementary Material for the full propensity-matched regression results).
Adjusted hazard ratios (95% CI) of hospitalization due to CV events in propensity score-matched β-blocker users. Red or bold indicates significance vs. nebivolol, P < 0.05. Hazard ratios were adjusted for demographics (age, sex, and geographical region), CCI score, diagnosis of chronic pulmonary disease, rheumatic disease, renal disease, or diabetes (per CCI), and use of other antihypertensive drugs during baseline. CCI Charlson Comorbidity Index, CHF congestive heart failure, CI confidence interval, CV cardiovascular, MI myocardial infarction
The unadjusted incidence rates [95% CI] of hospitalization due to a composite CV event (per 1000 person-years) in the matched cohorts were higher for the atenolol (7.80 [6.61–9.13]) and metoprolol cohorts (9.45 [8.12–10.92]) than for nebivolol (4.69 [3.78–5.75]; all P < 0.05; Table 2). For each individual component of the composite CV event, only the incidence rate for angina in the metoprolol cohort reached statistical significance (metoprolol 5.23 [4.26–6.36]; nebivolol: 1.93 [1.37–2.65]; P < 0.05.
Discussion
In this large, retrospective, real-world cohort study of patients with uncomplicated hypertension, monotherapy with the β-blocker nebivolol was associated with a lower risk of hospitalization due to CV events than either atenolol or metoprolol monotherapy. In the US, β-blockers are no longer considered first-line treatments in uncomplicated hypertension [8] as this drug class has been associated with increased CV risks compared with other antihypertensive classes [3,4,5,6,7]. Unfortunately, the majority of studies on which these conclusions were based used non-vasodilating β-blockers (mainly atenolol and metoprolol). While it is possible that the vasodilating blockers (carvedilol and nebivolol) may confer more consistent CV risk reductions due to their distinct hemodynamic mechanisms, further studies into possible differences of vasodilating versus non-vasodilating β-blockers on CV outcomes may better inform clinical decisions.
In studies comparing the effects of different β-blockers on measures of central blood pressure, an independent predictor of CV morbidity and mortality [18], greater improvements occurred in hypertensive patients taking nebivolol than atenolol or metoprolol regardless of similar reductions in brachial blood pressure [12, 19]. Furthermore, nebivolol improves (i.e., reduces) the augmentation index independent of heart rate changes [20], which could contribute to the reduced risk of MI and angina with nebivolol observed in our multivariable hazard regression analysis. Improvements in central blood pressure parameters with nebivolol may reflect its endothelium-dependent vasodilation via nitric oxide [10].
Real-world data from the current study show that physicians prescribe β-blockers as monotherapy in treating hypertension and maintain patients at different doses than recommended in the prescribing inserts. For example, mean daily doses of atenolol (45.2 mg), and metoprolol tartrate (66.8 mg) were lower than recommended daily doses in the prescribing inserts (atenolol 50–100 mg [25 mg for renally impaired patients] [21]); metoprolol tartrate 100–450 mg [22]), while the daily nebivolol dose was at the low end of the recommended daily dose range (mean dose: 7.4 mg; recommended: 5–40 mg [14]). It is possible that patients in the atenolol and metoprolol groups could have had greater reductions in CV event rates if they had been prescribed the recommended dosages; however, the data from large clinical trials in which atenolol was prescribed at the recommended dosages (50–100 mg/day) found that CV risks were higher with atenolol than with the comparator treatments [6, 7]. The real-world data from the present study indicate that atenolol and metoprolol are typically prescribed at lower than recommended monotherapy doses for hypertension, whereas nebivolol is prescribed within the recommended daily dose range. This apparent discrepancy in clinical use versus recommended use may be a reflection of physician experience. As such, it is important for the prescriber to not only consider data from prospectively designed clinical trials in which recommended doses were prescribed, but also those that are derived from real-world clinical experience wherein lower than recommended doses are often prescribed.
Many studies have shown that response to antihypertensive drugs can depend on individual patient characteristics, including age, race, ethnicity, sex, and genetic polymorphisms [23,24,25]. While nebivolol is effective and has a positive safety profile in many different hypertensive patient populations [26,27,28,29], the observed differences in CV event rates reported here may be due to dissimilarities in patient race or ethnicity across treatment cohorts. However, race and ethnicity were not captured in this dataset.
This study had several limitations due to the retrospective nature of the analyses. Despite the adjustments and matching for relevant baseline characteristics and demographics (except for race/ethnicity, which were not available in the database), unobserved differences due to treatment selection bias cannot be completely ruled out. Results may not be generalizable to uninsured populations, Medicaid recipients, or the US population as a whole. As medication use was assessed via pharmacy claims record, consumption of the medication cannot be confirmed. Prescribing bias due to physicians’ prior experience with or knowledge of certain β-blockers cannot be ruled out. Patients with exclusionary medical conditions may have been included in this analysis as data coding may not have fully captured their medical histories. Blood pressure and heart rate information were only available for 10% of the study population in this claims database, and thus were not included in this analysis. Doses and dosages of other antihypertensive drugs used during baseline were not examined. As there was no wash-out period, we cannot account for any residual effects of baseline medications on the study outcomes. Finally, this study of β-blocker monotherapy may not be representative of real-world β-blocker use as 75% of hypertensive patients require combination antihypertensive treatment to control their BP [30].
Conclusion
The results of this large retrospective, propensity-matched–cohort study of adult hypertensive patients are consistent with the notion that the large degree of heterogeneity among β-blockers may differentially impact CV outcomes. Long-term outcome studies are needed to fully examine how antihypertensive treatment with different β-blockers may affect CV event risk, especially when combined with other drug classes.
References
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 4. Effects of various classes of antihypertensive drugs—overview and meta-analyses. J Hypertens. 2015;33(2):195–211.
Lindholm LH, Carlberg B, Samuelsson O. Should β-blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366(9496):1545–53.
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665.
Wiysonge CS, Bradley HA, Volmink J, Mayosi BM, Mbewu A, Opie LH. Beta-blockers for hypertension. Cochrane Database Syst Rev. 2012;11:Cd002003.
Dahlöf B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995–1003.
Dahlöf B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895–906.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). J Am Med Assoc. 2014;311(5):507–20.
Pedersen ME, Cockcroft JR. The vasodilatory beta-blockers. Curr Hypertens Rep. 2007;9(4):269–77.
Munzel T, Gori T. Nebivolol: the somewhat-different beta-adrenergic receptor blocker. J Am Coll Cardiol. 2009;54(16):1491–9.
Fongemie J, Felix-Getzik E. A review of nebivolol pharmacology and clinical evidence. Drugs. 2015;75(12):1349–71.
Redon J, Pascual-Izuel JM, Rodilla E, Vicente A, Olivan J, Bonet J, et al. Effects of nebivolol and atenolol on central aortic pressure in hypertensive patients: a multicenter, randomized, double-blind study. Blood Press. 2014;23(3):181–8.
Kamp O, Sieswerda GT, Visser CA. Comparison of effects on systolic and diastolic left ventricular function of nebivolol versus atenolol in patients with uncomplicated essential hypertension. The American Journal of Cardiology. 2003;92(3):344–8.
Bystolic® (nebivolol tablets). US prescribing information. Cincinnati: Forest Pharmaceuticals, Inc. 2016.
Van Bortel LM, Fici F, Mascagni F. Efficacy and tolerability of nebivolol compared with other antihypertensive drugs: a meta-analysis. Am J Cardiovasc Drugs. 2008;8(1):35–44.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2010;31(15):1865–71.
Kampus P, Serg M, Kals J, Zagura M, Muda P, Karu K, et al. Differential effects of nebivolol and metoprolol on central aortic pressure and left ventricular wall thickness. Hypertension. 2011;57(6):1122–8.
Studinger P, Tabak AG, Chen CH, Salvi P, Othmane TE, Torzsa P, et al. The effect of low-dose carvedilol, nebivolol, and metoprolol on central arterial pressure and its determinants: a randomized clinical trial. J Clin Hypertens (Greenwich, Conn). 2013;15(12):910–7.
Tenormin® (atenolol tablets). US prescribing information. Wilmington: AstraZeneca Pharmaceuticals LP. 2011.
Lopressor® (metoprolol tartrate tablets). US prescribing information. East Hanover: Novartis Pharmaceuticals Corporation. 2008.
Brewster LM, Seedat YK. Why do hypertensive patients of African ancestry respond better to calcium blockers and diuretics than to ACE inhibitors and beta-adrenergic blockers? A systematic review. BMC Med. 2013;11:141.
Paz MA, de-La-Sierra A, Saez M, Barcelo MA, Rodriguez JJ, Castro S, et al. Treatment efficacy of anti-hypertensive drugs in monotherapy or combination: ATOM systematic review and meta-analysis of randomized clinical trials according to PRISMA statement. Medicine (Baltimore). 2016;95(30):e4071.
Materson BJ. Variability in response to antihypertensive drugs. Am J Med. 2007;120(4 Suppl 1):S10–20.
Mende CW, Giles TD, Bharucha DB, Ferguson WG, Mallick M, Patel MD. Efficacy of nebivolol-valsartan single-pill combination in obese and nonobese patients with hypertension. J Clin Hypertens (Greenwich, Conn). 2017;19:632–9.
Punzi H, Lewin A, Lukic T, Goodin T, Wei C. Efficacy and safety of nebivolol in Hispanics with stage I-II hypertension: a randomized placebo-controlled trial. Ther Adv Cardiovasc Dis. 2010;4(6):349–57.
Giles TD, Khan BV, Lato J, Brener L, Ma Y, Lukic T. Nebivolol monotherapy in younger adults (younger than 55 years) with hypertension: a randomized, placebo-controlled trial. J Clin Hypertens (Greenwich, Conn). 2013;15(9):687–93.
Saunders E, Smith WB, DeSalvo KB, Sullivan WA. The efficacy and tolerability of nebivolol in hypertensive African American patients. J Clin Hypertens (Greenwich, Conn). 2007;9(11):866–75.
Gradman AH, Basile JN, Carter BL, Bakris GL. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(1):42–50.
Acknowledgements
The authors thank the participants of the study.
Funding
All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. All processing charges were funded by Allergan plc, Madison, NJ, US (study sponsor).
Medical Writing and Editorial Assistance
The authors wish to also acknowledge the editorial and writing contributions of Lynn M. Anderson, PhD and Kristen A. Andersen, PhD of Prescott Medical Communications Group, Chicago, IL, funded by Allergan plc, Madison, NJ, US.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Prior Presentation
These data were previously presented at The American Heart Association Annual Meeting, held November 12–16, 2017; the American College of Cardiology Annual Meeting, held March 17–19, 2017; and the American Academy of Nurse Practitioners Annual Meeting, held June 20–25, 2017.
Disclosures
Jan Basile has received speaker/honorarium and consultant fees from Arbor Pharmaceuticals; all fees are “modest”. Brent Egan has received royalties from UpToDate, research support from Medtronic and Quintiles, honoraria as a consultant from AstraZeneca, Medtronic, and Valencia and as a lecturer from Merck-Sorono. Henry Punzi has received “significant” speaker and consultant fees from Astra Zeneca and “significant” research grants from Ferrer Internacional S.A., Boehringer Ingelheim, Actelion, Astra Zeneca, and the National Institutes of Health; he has received “modest” research grants, speaker and consultant fees from Allergan. Sanjida Ali was affiliated at Allergan plc, Madison, New Jersey, USA at the time of the study, and is currently affiliated with Progenics Pharmaceuticals, Inc, not affiliated with this study. Mehul Patel is an employee of Allergan plc. Qian Li is an employee of Evidera (a division of PPD), a consulting firm that received funding from Allergan to plan and conduct the analyses reported here. Joel Neutel functioned as a PI in this study.
Compliance with Ethics Guidelines
This study is based on de-identified data collected from a health care claims database and does not contain any studies with human participants or animals performed by any of the authors, therefore informed consent was not obtained.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.6965000.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Basile, J., Egan, B., Punzi, H. et al. Risk of Hospitalization for Cardiovascular Events with β-Blockers in Hypertensive Patients: A Retrospective Cohort Study. Cardiol Ther 7, 173–183 (2018). https://doi.org/10.1007/s40119-018-0117-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-018-0117-y