Abstract
The development of technologies with rapid and sensitive detection capabilities and increased throughput have become crucial for responding to greater number of threats posed by emerging and re-emerging viruses in the recent past. The conventional identification methods require time-consuming culturing, and/or detection of antibodies, which are not very sensitive and specific. The recent advances in molecular biology techniques in the field of genomics and proteomics greatly facilitate the rapid identification with more accuracy. The real-time assays viz; SYBR green I based real time RT-PCR and RT-LAMP have been developed for rapid detection as well as typing of some of the emerging arboviruses of biomedical importance viz; Dengue, Japanese Encephalitis, Chikungunya, West Nile, SARS and Swine Flu etc. Both these techniques are capable of detection and differentiation as well as quantifying viral load with higher sensitivity, rapidity and specificity. One of the most important advantages of RT-LAMP is its field applicability, without requirement of any sophisticated equipments. The establishment of these real time molecular assays will certainly facilitate the rapid detection of viruses with high degree of precision and accuracy in future.
Similar content being viewed by others
Introduction
The last decade has witnessed emergence and re-emergence of several microbial diseases with pronounced virulence thereby causing severe large scale epidemics every year on regular basis. Majority of such diseases belong to the group of vector-borne infections due to various factors such as massive urbanization and change in ecosystem leading to evolutionary pressure etc. By far the most important vector borne infections include arthropod borne viral diseases which constitute 90% of the re-emerging diseases. Despite decades of efforts, no approved vaccine is currently available for many viral diseases. The accurate and rapid detection of viral infection is also essential for successful antiviral treatment as the irreversible damages to cellular functions occurs very early in most virus infections [1]. The rapid diagnosis of virus diseases has assumed greater significance owing to the direct benefit of patient management in the absence of suitable therapeutic and prophylactic measures.
An increasing diversity of methods are available which make it possible to detect and analyze any virus, including those, which cannot be cultured. The laboratory diagnosis of virus infection can be made by the detection of specific virus, viral antigen, genomic sequences and/or antibodies [2]. The presence of virus can be detected by isolation in cell culture or more directly by electron microscopy. Virus isolation is rarely used for diagnosis because it is time consuming and technically difficult. Alternatively, the presence of either viral antigen or nucleic acid can be demonstrated by employing immunological and molecular techniques. In addition, viruses are good immunogen and thus elicit strong and highly specific antibodies that are maintained in the blood system for a prolonged period and are relatively easy to detect. Therefore, most virus diagnostic assays are based on the detection of anti-viral antibodies. The demonstration of such antibodies provides indirect evidence of infection with that virus. The routinely used immunological techniques for laboratory diagnosis of virus infections are—Enzyme linked Immunosorbent assay (ELISA), Immunofluorescence Test (IFT), Immuno Chromoatographic Test (ICT). ICT is now gaining more popularity and widely used test system as a rapid screening system for large number of clinical samples especially during epidemics. However, the limitation associated with detection of antibody responses in putative “patients” is the presence of antibodies which do not necessarily indicate current virus infection—they may reflect events, which occurred many years earlier.
The rapid diagnosis of virus diseases has assumed greater significance owing to the direct benefit of patient management in absence of suitable therapeutic and prophylactic measures [3]. With the advancement of technologies, increasingly diverse methods are available which make it possible to detect and analyze any virus, including those, which cannot be cultured. The laboratory diagnosis of virus infection can be made by the detection of specific virus, viral antigen, genomic sequences and/or antibodies. Nucleic acid amplification is one of the most valuable tools in virtually all life science fields, including application-oriented fields such as clinical medicine in which diagnosis of infectious diseases, genetic disorders and genetic traits are particularly benefited by this new technique [4]. Although several amplification methods have been developed, PCR is the most widely used because of its apparent high simplicity and reliability. Routine use of PCR as a standard approach in biotechnology and medical diagnostic laboratories has been usually practiced. During the past decade, various forms of PCRs such as Reverse transcription polymerase chain reaction (RT-PCR), Nested PCR and Multiplex PCR have been developed to address the need for rapid identification of viruses to serotype level with more accuracy. Despite the obtainable magnitude of amplification, these PCR based methods require either high precision instruments for the amplification or elaborate methods for detection of the amplified products. In addition, the PCR method has several intrinsic disadvantages, such as the requirement of thermal cycling, insufficient specificity and rather low amplification efficiency. More sensitive and real time based assays are therefore needed to complement the existing PCR based assay systems.
Real-Time PCR
The Real-time PCR assay has many advantages over conventional PCR methods, including rapidity, quantitative measurement, lower contamination rate, higher sensitivity, higher specificity, and easy standardization. Thus, nucleic acid-based assays or real-time quantitative assay might eventually replace virus isolation and conventional RT-PCR as the new gold standard for the rapid diagnosis of virus infection in the acute-phase samples. The majority of diagnostic PCR assays reported to date have been used in a qualitative, or ‘yes/no’ format. The development of real-time PCR has brought true quantitation of target nucleic acids out of the pure research laboratory and into the diagnostic laboratory [1].
Real-time Reporters (SYBR® Green, TaqMan®, and Molecular Beacons)
All real-time PCR systems rely upon the detection and quantitation of a fluorescent reporter, the signal of which increases in direct proportion to the amount of PCR product in a reaction. In the simplest and most economical format, that reporter is the double-strand DNA-specific dye SYBR® Green (Molecular Probes) [9]. SYBR Green binds to double-stranded DNA, and upon excitation emits light. Thus, as a PCR product accumulates, the fluorescence increases. The advantages of SYBR Green are that it is inexpensive, easy to use, and sensitive. The disadvantage is that SYBR Green will bind to any double-stranded DNA in the reaction, including primer-dimers and other non-specific reaction products, which results in an overestimation of the target concentration. For single PCR product reactions with well-designed primers, SYBR Green can work extremely well, with spurious non-specific background only showing up in very late cycles [10]. The two most popular alternatives to SYBR Green are TaqMan® and molecular beacons, both of which are hybridization probes relying on fluorescence resonance energy transfer (FRET) for quantitation (Fig. 1a).
TaqMan Probes are oligonucleotides that contain a fluorescent dye, typically on the 5′ base, and a quenching dye, typically located on the 3′ base. When irradiated, the excited fluorescent dye transfers energy to the nearby quenching dye molecule rather than fluorescing, resulting in a nonfluorescent substrate (Fig. 1b). TaqMan probes are designed to hybridize to an internal region of a PCR product. During PCR, when the polymerase replicates a template on which a TaqMan probe is bound, the 5′ exonuclease activity of the polymerase cleaves the probe. This separates the fluorescent and quenching dyes and FRET no longer occurs. Fluorescence increases in each cycle in proportion to the rate of probe cleavage (Fig. 2).
Molecular beacons also contain fluorescent and quenching dyes, but FRET only occurs when the quenching dye is directly adjacent to the fluorescent dye. Molecular beacons are designed to adopt a hairpin structure while free in solution, bringing the fluorescent dye and quencher in close proximity. When a molecular beacon hybridizes to a target, the fluorescent dye and quenchers are separated, FRET does not occur, and the fluorescent dye emits light upon irradiation. Unlike TaqMan probes, molecular beacons are designed to remain intact during the amplification reaction, and must rebind to target in every cycle for signal measurement [11].
TaqMan probes and molecular beacons allow multiple DNA species to be measured in the same sample (multiplex PCR), since fluorescent dyes with different emission spectra may be attached to the different probes. Multiplex PCR allows internal controls to be co-amplified and permits allele discrimination in single-tube, homogeneous assays. These hybridization probes afford a level of discrimination impossible to obtain with SYBR Green, since they will only hybridize to true targets in a PCR and not to primer-dimers [12].
Application of Real-Time PCR in Virus Diagnosis
Real-time PCR has become the benchmark for the detection and quantification of viruses and is being utilized increasingly in novel clinical diagnostic assays. Quantitative results obtained by this technology are not only more informative than qualitative data, but simplify assay standardization and quality management. Quantitative PCR (QPCR) assays are most established for the detection of viral load and therapy monitoring. Further, nucleotide sequence analysis of the amplification products has facilitated epidemiological studies of infectious disease outbreaks, and the monitoring of treatment outcomes for infections, in particular with viruses which mutate at high frequency [10].
Several investigators have reported fully automatic real-time PCR assays for the detection of viruses in acute-phase serum samples. With improved and automated nucleic acid sample isolation techniques, as well as real-time detection methods, a new generation of assays for most clinically important viruses is being developed [13, 14]. QPCR assays based on SYBR Green and TaqMan chemistries have been developed and validated and are beginning to reveal the virus’s epidemiology and pathogenesis. The QPCR assay also provides critical prognostic information for clinical management. The real-time PCR assays have been increasingly used for early and accurate detection as well as quantification of all most all human viruses including Measles, Mumps, HSV (Herpes Simplex virus), Rota virus, Noro virus, Influenza virus types A and B, Respiratory syncytial virus (RSV) and Para influenza virus (PIV) types 1–4, Severe Acute Respiratory Syndrome Virus (SARS) Dengue, Japanese Encephalitis (JE), West Nile, Chikungunya, Hepatitis B Virus (HBV), Hepatitis C Virus (HCV), Human Immunodeficiency Virus (HIV), Avian Flu (H5 N1) etc [15–19].
More recently, real-time PCR assays have provided additional major contributions, with the inclusion of an additional fluorescent probe detection system resulting in an increase in sensitivity over conventional PCR, the ability to confirm the amplification product and to quantitate the target concentration and detection of multiple targets in a single tube. Multiplex real-time quantitative RT-PCR assays have been developed for simultaneous detection, identification and quantification of HBV (hepatitis B virus), HCV (hepatitis C virus) and HIV-1 in plasma or serum samples [20–22].
However, the lack of commercially available validated reagent kits for most viruses remains a major problem, as does the absence of standardization of the existing tests. Besides, all these nucleic acid amplification methods have several intrinsic disadvantages of requiring either a high precision instrument for amplification or an elaborate complicated method for detection of amplified products. The high cost of instruments required for performing the real time assays restricted its use to laboratories with good financial resources [23–25, 28, 31].
Loop-Mediated Isothermal Amplification (LAMP)
“LAMP” which stands for Loop-mediated Isothermal Amplification is a simple, rapid, specific and cost-effective nucleic acid amplification method and is characterized by the use of six different primers specifically designed to recognize eight distinct regions on the target gene [5, 35]. The amplification proceeds at a constant temperature using strand displacement reaction. Amplification and detection of gene can be completed in a single step, by incubating the mixture of samples, primers, DNA polymerase with strand displacement activity and substrates at a constant temperature of 63°C. Compared to PCR and real-time PCR, the LAMP has the advantages of reaction simplicity and detection sensitivity. The higher sensitivity and specificity of the LAMP reaction is attributed to continuous amplification under isothermal condition employing six primers recognizing eight distinct regions of the target (Fig. 3). Besides, the higher amplification efficiency of LAMP reaction yields large amount of by-product, pyrophosphate ion, leading to white precipitate of magnesium pyrophosphate in the reaction mixture. Since the increase in turbidity of the reaction mixture according to the production of precipitate correlates with the amount of DNA synthesized, real-time monitoring of the LAMP reaction can be achieved by real-time measurement of turbidity [6].
Being an isothermal amplification, LAMP does not require any thermal cycler and thus can be performed even with heating block and/or water bath. Thus, LAMP method has the characteristics of not requiring special reagents and sophisticated temperature control device. Since it only requires simple equipments, cost effective point of care gene test can be achieved. Both simple detection and real-time detection of the reaction are possible. In addition, in case of LAMP, both amplification and detection occur simultaneously during the exponential phase without going through the plateau phase where the non spurious amplification leads to lower sensitivity and false positivity [7].
Designing of LAMP Primers
Designing of a highly sensitive and specific primer set is crucial for performing LAMP amplification. The target selection for primer designing can be accomplished by using the Primer Explore [LAMP primer designing support software program, Net laboratory, Japan (http://venus.netlaboratory.com)] after considering the base composition, GC contents and the formation of secondary structures. The primer set for LAMP amplification include a set of six primers comprising two outer, two inner and two loop primers that recognize eight distinct regions on the target sequence. The two outer primers were described as forward outer primer (F3) and backward outer primer (B3) and have a role in strand displacement during non-cyclic step only. The inner primers were described as forward inner primer (FIP) and backward inner primer (BIP) having both sense and antisense sequence in such a way that it helps in the formation of loop. Further, two loop primers viz; forward loop primer (FLP) and backward loop primer (BLP) were designed to accelerate the amplification reaction by binding to additional sites that are not accessed by internal primers (Fig. 4). LAMP amplification can also be accomplished with the two outer (F3 & B3) and two internal primers (FIP & BIP) but by using the two loop primers (FLP & BLP), the amplification is accelerated and thereby shortens amplification time by one third to one half [8].
Assay Protocol for RT-LAMP Amplification
The LAMP reaction is usually carried out in a total 25 μl reaction volume containing 50 pmol each of the primers FIP and BIP, 5 pmol each of the outer primers F3 and B3, 25 pmol each of loop primers FLP and BLP in a 2× reaction mixture having 20 mM Tris–HCl pH8.8, 10 mM (NH4)2SO4, 8 mM MgSO4, 10 mM KCl, 1.4 mM dNTPs, 0.8 M Betaine, 0.1% Tween20, 8 units of the Bst DNA polymerase (New England Biolabs), and 2 μl of DNA template. Positive and negative controls should be included in each run, and all precautions to prevent cross-contamination should be observed. The studies temperature optima required for efficient amplification by LAMP assay indicated that the optimum temperature for the LAMP reaction was 63°C, which is optimum for the activity of Bst DNA polymerase. The amplification of RNA template was accomplished through Reverse Transcription-Loop-mediated Isothermal Amplification (RT-LAMP) assay by employing reverse transcriptase for reverse transcription step in addition to the Bst DNA polymerase. RT-LAMP method can synthesize cDNA from template RNA and apply LAMP technology to amplify and detect them [26].
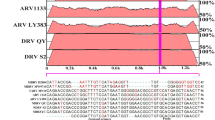
Monitoring of RT-LAMP Amplification
The real-time monitoring of-LAMP amplification can be accomplished through spectrophotometric analysis with the help of loop amp real-time turbidimeter (LA-200, Teramecs, Japan) that records the turbidity in the form of O.D. at 400 nm at every 6 s (Figs. 5, 6a). On agarose gel analysis, the LAMP amplicons revealed ladder like pattern in contrast to a single band as observed in PCR (Fig. 6b). This is due to the cauliflower-like structures with multiple loops formed by annealing between alternately inverted repeats of the target in the same strand [26].
Monitoring of LAMP Amplification. a The turbidity of magnesium pyrophosphate, a byproduct of the reaction, can be real-time detected by a real-time turbidimeter. b Agarose gel analysis revealing the typical electrophoresis pattern of LAMP amplified product, which is not a single band but a ladder pattern because LAMP method can form amplified products of various sizes consisting of alternately inverted repeats of the target sequence on the same strand. d The tube containing the amplified products in the presence of fluorescent intercalating dye is illuminated with a UV lamp, the fluorescence intensity increases
In order to facilitate the field application of LAMP assay, the monitoring of amplification can also be accomplished with naked eye inspection either in the form of visual turbidity or visual fluorescence. Following amplification, the tubes can be inspected for white turbidity through naked eye after a pulse spin to deposit the precipitate in the bottom of the tube. Hence, the presence of turbidity can indicate the presence of target gene (Fig. 6c). The tube containing the amplified products can also be better visualized in the presence of fluorescent intercalating dye viz; ethidium bromide, SYBR Green I and Calcein etc. by illuminating with a UV lamp, the fluorescence intensity increases. In practice, usually the visual inspection for amplification is performed through observation of color change following addition of 1 μl of SYBR Green I (a fluorescent dsDNA intercalating dye) to the tube. In case of positive amplification, the original orange color of the dye will change into green that can be judged under natural light as well as under UV light (302 nm) with the help of a hand held UV torch lamp. In case there is no amplification, the original orange color of the dye will be retained. This change of color is permanent and thus can be kept for record purpose (Fig. 6d) [27].
Quantitation of Gene Copy Numbers by LAMP Assay
Capitalizing on its exquisite sensitivity, LAMP has been designed to quantify the amount of gene copies in a person’s blood (load) thereby allowing physicians to monitor their patients’ disease progression and response to therapy. Assessment of the load of the organisms/pathogens before, during and after therapy has tremendous potential for improving the clinical management of diseases. The quantification of gene copy number and/or concentration of the organisms can be accomplished through generation of a standard curve by plotting a graph between known concentration of gene copy number or infectious unit of organisms and time of positivity to get the amplification signal for that particular concentration. A linear relationship between various concentrations Vs time of positivity is usually obtained through the real-time monitoring of the amplification (Fig. 7). The quantification of gene copies in the clinical samples can be extrapolated from the standard curve on the basis of their time of positivity [27].
LAMP in Clinical Diagnosis of Virus Infections
LAMP technology facilitates the detection of DNA or RNA of pathogenic organisms and, as such, is the basis for a broad range of clinical diagnostic tests for various infectious agents, including viruses and bacteria. These gene based tests have several advantages over traditional antibody-based diagnostic methods that measure the body’s immune response to a pathogen. In particular, LAMP is capable of detecting the presence of pathogenic agents earlier than PCR even on day one of fever where the amount of gene copy number is expected to be very low due to higher sensitivity with a detection limit of about 1–2 copies. Earlier detection of infection can mean earlier treatment and an earlier return to good health.
The loop mediated isothermal amplification (LAMP) assay is emerging as a simple, rapid and powerful gene amplification technique for early detection of microbial diseases. Although the inception of LAMP refers back to 1998 but the popularity of LAMP starts only after 2003 following emergence of West Nile and SARS viruses. Since then, LAMP assay is increasingly being adapted by researchers mostly from Japan in clinical diagnosis of emerging diseases including bacteria, viruses and parasitic diseases. LAMP has been successfully applied for rapid and real-time detection of both DNA and RNA viruses. However, most of the published researches have been directed for RNA viruses may be due to the increased incidence of RNA viruses in recent past in the form of major epidemic having significant public health importance. A one-step single tube real-time accelerated reverse transcription loop mediated isothermal amplification (RT-LAMP) assays have been developed for rapid detection of some of the recently emerged human viral pathogens viz; West Nile, SARS, Dengue, Japanese Encephalitis, Chikungunya, Norwalk, H5N1 highly pathogenic avian influenza (HPAI) viruses [29, 30]. On comparison to conventional RT-PCR, RT-LAMP assay demonstrated 10–100 fold more sensitivity with a detection limit of 0.01–10 PFU of virus in all these cases. The usefulness of LAMP for amplification of DNA viruses was also reported for HBV, HPV (Human papillomavirus) type—6,11, 16 & 18, HSV, VZV(Varivella Zooster Virus), CMV (Cytomegalo Virus) and found to be superior in terms of sensitivity, specificity, rapidity, and simplicity, and can potentially be a valuable tool for the detection of HPV DNA compared to PCR and real-time PCR [32–34].
Conclusion
The combination of excellent sensitivity and specificity, low contamination risk, and speed has made real-time PCR technology an appealing alternative to culture or immunoassay-based testing methods for diagnosing many infectious diseases. The recent advances in the development of fluorophores, nucleotide labeling chemistries, and the novel applications of oligoprobe hybridization have provided real-time PCR technologies with a broad enough base to ensure their acceptance. The LAMP is emerging as a new generation of cost effective and rapid gene amplification tool having all the characteristics of rapidity and high sensitivity of real-time assays as well as easy adaptability under field conditions due to its simple operation, rapid reaction, and easy detection. The rapidity and sensitivity of these real-time assays will assist in precise diagnosis, which is extremely useful to undertake suitable control measures and patient management at the earliest. The combination of the LAMP technology and the new detection method described here can overcome several factors that have been preventing true practical application of super-simple gene point of care testing (g-POCT). The integration of isothermal amplification and electrophoresis onto microchips can lead to LAMP on Chips for quick and accurate identification of disease producing genes at patient’s bed side.
References
Espy MJ, Uhl JR (2006) Real-Time PCR in clinical microbiology: applications for routine laboratory testing. Clin Micobiol Rev 19(1):165–256
Chan AB, Fox JD (1999) NASBA and other transcription-based amplification methods for research and diagnostic microbiology. Rev Med Microbiol 10:185–196
Parida MM (2008) Rapid and Real-time detection technologies for emerging viruses of biomedical importance. J Biol Sci 33(4):617–628
Ratcliff RM, Chang G (2007) Molecular diagnosis of medical viruses. Curr Issues Mol Biol 9(2):87–102
Notomi T, Okayama H (2000) Loop-mediated isothermal amplification of DNA. Nucleic Acids Res 28(12):e63
Mori Y, Hirano T (2006) Sequence specific visual detection of LAMP reactions by addition of cationic polymers. BMC Biotechnol 6:1–10
Ushikubo H (2004) Principle of LAMP method—a simple and rapid gene amplification method. Virus 54(1):107–112
Nagamine K, Hase T (2002) Accelerated reaction by loop mediated isothermal amplification using loop primers. Mol Cell Prob 16:223–229
Mackay IM, Arden KE (2002) Real-time PCR in virology. Nucleic Acids Res 30:1292–1305
Niesters HG (2002) Clinical virology in real time. J Clin Virol 25(Suppl 3):S3–S12
Gunson RN, Collins TC (2006) Practical experience of high throughput real time PCR in the routine diagnostic virology setting. J Clin Virol 35(4):355–367
Watzinger F, Ebner K (2006) Detection and monitoring of virus infections by real-time PCR. Mol Aspects Med 27(2–3):254–298
Dong-Kun Y, Kweon CH (2004) TaqMan reverse transcription polymerase chain reaction for the detection of Japanese encephalitis virus. J Vet Sci 5:345–351
Jiang SS, Chen TC (2004) Sensitive and quantitative detection of severe acute respiratory syndrome coronavirus infection by real-time nested polymerase chain reaction. Clin Infect Dis 38:293–296
Enders KO, Peter NG (2005) Influenza A H5N1 Detection. Emerg Infect Dis 11(8):1303–1305
Chien LJ, Liao TL (2006) Development of real-time reverse transcriptase PCR assay to detect and serotype dengue viruses. J Clin Microbiol 44(4):1295–1304
Poon LL, Chan KH, Wong OK (2003) Early diagnosis of SARS coronavirus infection by real time RT-PCR. J Clin Virol 28:233–238
Ruelle J, Mukadi BK, Schutten M, Goubau P (2004) Quantitative real-time PCR on Lightcycler for the detection of human immunodeficiency virus type 2 (HIV-2). J Virol Methods 117:67–74
Santhosh SR, Parida MM, Dash PK (2007) Development and evaluation of SYBR Green I based one step real time RT-PCR assay for detection and quantification of Japanese encephalitis virus. J Virol Methods 143(1):73–80
Shu PY, Chang SF (2003) Development of group- and serotypespecific one-step SYBR green I-based real-time reverse transcription-PCR assay for dengue virus. J Clin Microbiol 41:2408–2416
Sugiyama H, Yoshikawa T, Ihira M, Enomoto Y, Kawana T, Asano Y (2005) Comparison of loop-mediated isothermal amplification, real-time PCR, and virus isolation for the detection of herpes simplex virus in genital lesions. J Med Virol 75(4):583–587
Templeton KE, Scheltinga SA (2004) Rapid and sensitive method using multiplex real-time PCR for diagnosis of infections by influenza a and influenza B viruses, respiratory syncytial virus, and parainfluenza viruses 1, 2, 3, and 4. J Clin Microbiol 42:1564–1569
Verstrepen WA, Kuhn S, Kockx MM (2001) Rapid detection of enterovirus RNA in cerebrospinal fluid specimens with a novel single-tube real-time reverse transcription-PCR assay. J Clin Microbiol 39:4093–4096
Beuret C (2004) Simultaneous detection of enteric viruses by multiplex real-time RT-PCR. J Virol Methods 115:1–8
Parida MM, Horioke K, Ishida H (2005) Rapid detection and differentiation of dengue virus serotypes by a real-time reverse transcription-loop-mediated isothermal amplification assay. J Clin Microbiol 43:2895–2903
Parida MM, Santhosh SR, Dash PK (2006) Development and evaluation of reverse transcription loop mediated isothermal amplification assay for rapid and Real-time detection of Japanese encephalitis virus. J Clin Microbiol 44(11):4172–4178
Parida MM, Santhosh SR, Dash PK (2007) Rapid and real-time detection of Chikungunya virus by reverse transcription loop mediated isothermal amplification assay. J Clin Microbiol 45(2):351–357
Parida MM, Santhosh SR, Dash PK, Lakshmana Rao PV, Morita K (2008) Rapid and real-time assays for detection and quantification of Chikungunya virus. Future Virol 3(2):179–192
Hong TC, Mai QL, Cuong DV (2004) Development and evaluation of a novel loop-mediated isothermal amplification method for rapid detection of severe acute respiratory syndrome coronavirus. J Clin Microbiol 42(5):1956–1961
Imai M, Ninomiya A, Minekawa H (2006) Rapid diagnosis of H5N1 avian influenza virus infection by newly developed influenza H5 hemagglutinin gene-specific loop-mediated isothermal amplification method. Vaccine 24(44–46):6679–6682
Toriniwa H, Komiya T (2006) Rapid detection and quantification of Japanese encephalitis virus by real-time reverse transcription loop-mediated isothermal amplification. Microbiol Immunol 50(5):379–387
Enomoto Y, Yoshikawa T, Ihira M (2005) Rapid diagnosis of herpes simplex virus infection by a loop-mediated isothermal amplification method. J Clin Microbiol 43(2):951–955
Hagiwara M, Sasaki H, Matsuo K, Honda M, Kawase M, Nakagawa H (2007) Loop-mediated isothermal amplification method for detection of human papillomavirus type 6, 11, 16, and 18. J Med Virol 79(5):605–615
Kubo T, Agoh M, Mai LQ, Fukushima K, Nishimura H, Yamaguchi A, Hirano M, Yoshikawa A, Hasebe F, Kohno S, Morita K (2010) Development of a reverse transcription loop mediated isothermal amplification assay for detection of pandemic (H1N1) 2009 virus as a novel molecular method for diagnosis of pandemic influenza in resource limited settings. J Clin Microbiol 48(3):728–735
Yasuyoshi M, Notomi T (2009) Loop mediated isothermal amplification (LAMP): a rapid, accurate, and cost effective diagnostic method for infectious diseases. J Infect Chemother 15:62–69
Acknowledgments
The authors are thankful to Dr. R. Vijayaraghavan, Director, Defence Research and Development Establishment, Gwalior for his keen interest and constant inspiration.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parida, M., Shukla, J., Sharma, S. et al. Rapid and Real-time Detection of Human Viral Infections: Current Trends and Future Perspectives. Proc. Natl. Acad. Sci. Sect B. Biol. Sci. 82, 199–207 (2012). https://doi.org/10.1007/s40011-011-0015-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40011-011-0015-8