Abstract
Purpose
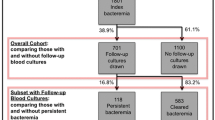
Data on the systemic dissemination in Staphylococcus aureus bloodstream infection (SAB) remain sparse. We investigated the timing and the sequence of clinical symptoms, diagnostic confirmation, and occurrence of multiple infective foci in relation to three major infective foci.
Methods
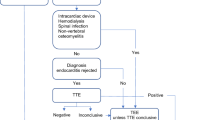
From 2006 to 2011, all adult patients with first-time SAB in Cologne and Freiburg, Germany were followed prospectively. The study was restricted to patients with short-term central venous catheter (CVC)-related SAB, vertebral osteomyelitis (VO), and infective endocarditis (IE). The collection date of the first positive blood culture was used as reference point for determining time to onset of clinical symptoms, microbiological findings, imaging results compatible with focal infection, and occurrence of additional infective foci.
Results
We included 266 patients with first-time SAB. Among patients with CVC-related SAB, clinical onset, collection of the first positive blood culture, and microbiological confirmation almost coincided. In contrast, among patients with VO or IE, the onset of clinical symptoms most often preceded the collection of the first positive blood culture, and imaging and microbiological confirmation were most frequently obtained subsequent to the SAB diagnosis. CVC-related SAB was infrequently associated with further foci (n = 15/15.5%). Conversely, more than one infective focus was observed in 44 (56.4%) patient with VO and 68 (64.8%) patients with IE.
Conclusions
The sequence of clinical symptoms, diagnostic confirmation, and occurrence of multiple infective foci varied considerably with different infective foci in SAB. Based on these results, we propose a pragmatic and evidence-based terminology for the clinical course of SAB and suggest the terms “portal of entry”, “infective focus”, “multiple infective foci”, and “dominant infective focus”.

Similar content being viewed by others
References
Kaasch A, Barlow G, Edgeworth JD, Fowler VG Jr, Hellmich M, Hopkins S, et al. Staphylococcus aureus bloodstream infection: a pooled analysis of five prospective, observational studies. J Infect. 2014;68:242–51.
van Hal SJ, Jensen SO, Vaska VL, Espedido BA, Paterson DL, Gosbell IB. Predictors or mortality in Staphylococcus aureus bacteremia. Clin Microbiol Rev. 2012;25:362 – 86.
Gudiol F, Aguado JM, Almirante B, Bouza E, Cercenado E, Domínguez M, et al. Diagnosis and treatment of bacteremia and endocarditis due to Staphylococcus aureus. A clinical guideline from the Spanish Society of Clinical Microbiology and Infectious Diseases (SEIMC). Enferm Infecc Microbiol Clin. 2015;33:625.e1–625.e23
Holland TL, Arnold C, Fowler VG Jr. Clinical management of Staphylococcus aureus bacteremia. JAMA. 2014;312:1330–41.
Tong SYC, Davis JS, Eichenberger E, Holland TL, Fowler VG Jr. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev. 2015;28:603–61.
Soriano A, Martinez JA, Mensa J, Marco F, Almela M, Moreno-Martínez A, et al. Pathogenic significance of methicillin resistance for patients with Staphylococcus aureus bacteremia. Clin Infect Dis. 2000;30:368–73.
Nolan CM, Beaty HN. Staphylococcus aureus bacteremia. Current clinical patterns. Am J Med. 1976;60:495–500.
Lautenschlager S, Herzog C, Zimmerli W. Course and outcome of bacteremia due to Staphylococcus aureus: Evaluation of different clinical case definitions. Clin Infect Dis. 1993;16:567–73.
Mylotte JM, Tayara A. Staphylococcus aureus bacteremia: predictors of 30-day mortality in a large cohort. Clin Infect Dis. 2000;31:1170–4.
Cuijpers ML, Vos FJ, Bleeker-Rovers CP, Krabbe PF, Pickkers P, van Dijk AP, et al. Complicating infectious foci in patients with Staphylococcus aureus or Streptococcus species bacteraemia. Eur J Clin Microbiol Infect Dis. 2007;26:105–13.
Saginur R, Suh KN. Staphylococcus aureus bacteraemia of unknown primary source: Where do we stand? Int J Antimicrob Agents. 2008;32:S21-25.
del Rio A, Cervera C. Moreno A, Moreillon P, Miró JM. Patients at risk of complications of Staphylococcus aureus bloodstream infection. Clin Infect Dis. 2009;48:S246-253.
Price J, Baker G, Heath I, Walker-Bone K, Cubbon M, Curtis S, et al. Clinical and microbiological determinants of outcome in Staphylococcus aureus bacteraemia. Int J Microbiol 2010;2010:654858.
Asgeirsson H, Kristjansson M, Kristinsson KG, Gudlaugsson O. Clinical significance of Staphylococcus aureus bacteriuria in a nationwide study of adults with S. aureus bacteremia. J Infect. 2012;64:41–6.
Paulsen J, Mehl A, Askim Å, Solligård E, Åsvold BO, Damås JK. Epidemiology and outcome of Staphylococcus aureus bloodstream infection and sepsis in a Norwegian county 1996–2011: an observational study. BMC Infect Dis. 2015;15:116. https://doi.org/10.1186/s12879-015-0849-4.
https://www.cdc.gov/nhsn/pdfs/pscmanual/4psc_clabscurrent.pdf. 2018. Accessed 22 Feb 2018
Seifert H, Wisplinghoff H, Kaasch A, Achilles K, Langhorst A, Peyerl-Hoffmann G, et al. Epidemiology, course and prognosis of Staphylococcus aureus bacteremia - Preliminary results from the INSTINCT (INvasive STaphylococcus aureus INfection CohorT) cohort. Dtsch Med Wochenschr. 2008;133:340–5.
Kaasch AJ, Fowler VG Jr, Rieg S, Peyerl-Hoffmann G, Birkholz H, Hellmich M, et al. Use of a simple criteria set for guiding echocardiography in nosocomial Staphylococcus aureus bacteremia. Clin Infect Dis. 2011;53:1–9.
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Healthcare-associated infections in adults: a reason to the change the accepted definition if community-acquired infections. Ann Intern Med. 2002;137:791–7.
Charlson M, Pompei P, Ales KL. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chron Dis. 1987;40:373 – 83.
Horino T, Sato F, Hosaka Y, Hoshina T, Tamura K, Nakahrai K, et al. Predictive factors for metastatic infection in patients with bacteremia caused by methicillin-sensitive Staphylococcus aureus. Am J Med Sci. 2015;349:24–8.
Kim SH, Park WB, Lee KD, Kang CI, Kim HB, Oh MD, et al. Outcome of Staphylococcus aureus bacteremia in patients with eradicable foci versus noneradicable foci. Clin Infect Dis. 2003;37:794–9.
Vos FJ, Kullberg BJ, Sturm PD, Krabbe PF, van Dijk AP, Wanten GJ, et al. Metastatic infectious disease and clinical outcome in Staphylococcus aureus and Streptococcus species bacteremia. Medicine (Baltimore). 2012;91:86–94.
Ringberg H, Thorén A, Lilja B. Metastatic complications of Staphylococcus aureus septicemia. To seek is to find. Infection. 2000;28:132–6.
Fowler VG Jr, Olsen MK, Corey GR, Woods CW, Cabell CH, Reller LB, et al. Clinical identifiers of complicated Staphylococcus aureus bacteremia. Arch Intern Med. 2003;163:2066–72.
Acknowledgements
The authors thank Christian Bernasch (Institute for Medical Microbiology, Immunology and Hygiene, University of Cologne, Germany), Hanna Birkholz (Clinical Trials Center, University of Cologne, Germany), and Gabriele Peyerl-Hoffmann (Department of Medicine II, University Medical Center Freiburg, Germany) for providing administrative support and collecting patient data.
Funding
This work was supported by the Deutsche Forschungsgemeinschaft (DFG; grant number KA 3104/1–1 to A.J.K.), the Paul-Ehrlich Gesellschaft für Chemotherapie (to HS and WVK), and the Bundesministerium für Bildung und Forschung (BMBF 01KI1017 to AJK/01KN1106 to the Clinical Trial Center Cologne). The funding organizations had no role in the design of the study, data collection, and data analysis.
Author information
Authors and Affiliations
Contributions
JS: study design, data management, analysis and interpretation, and manuscript preparation. AJK: data collection, study concept and design, data management, analysis and interpretation, and manuscript review. SRR, WVK, HS, AFW: data collection, study design, interpretation of the data, manuscript review. HCS: study design, interpretation of the data, manuscript review. All the authors have read and approved the final draft submitted.
Corresponding author
Ethics declarations
Ethical approval
The study and data collection were approved by the institutional review boards of the University Medical Centers Freiburg and Cologne. We followed the ethical standards set by the Helsinki Declaration of 1975, as revised in 2004, and the research guidelines of the Universities of Freiburg and Cologne. Written informed consent was obtained from the patients at the University Medical Center Cologne. The institutional review board of the University Medical Center Freiburg considered the investigation as evaluation of service within a quality assurance program and waived the need for written informed consent. The study is registered in the German Clinical Trials Registry (DRKS00005045).
Conflict of interest
A.J.K. has received payments for lectures from BD Biosciences, bioMérieux, MSD Sharp & Dohme, Limbach Gruppe SE, and ViiV Healthcare and travel support from Janssen-Cilag. H.S. has received grants or research support from the Bundesministerium für Bildung und Forschung (BMBF), Germany, the German Centre for Infection Research (DZIF), Basilea, Novartis and Pfizer, has been a consultant for Astellas, AstraZeneca, Basilea, Cubist, Novartis, Pfizer, Tetraphase, and The Medicines Company, and has received payments for lectures from MSD, Novartis and Pfizer. S.R. has received payments for lectures from Pfizer and MSD Sharp & Dohme, as well as travel support from Astellas and MSD Sharp & Dohme. W.V.K., A.F.W., J.S and H.C.S report no conflicts.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Smit, J., Rieg, S.R., Wendel, A.F. et al. Onset of symptoms, diagnostic confirmation, and occurrence of multiple infective foci in patients with Staphylococcus aureus bloodstream infection: a look into the order of events and potential clinical implications. Infection 46, 651–658 (2018). https://doi.org/10.1007/s15010-018-1165-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1165-x