Abstract
Obesity and overweight status is growing rapidly worldwide. Although there have been enormous advances in explaining the genetic basis of obesity in recent years, the pathways that lead to a high body weight are still not fully understood. Interactions between genetic and environmental factors, including nutrient exposures and dietary behaviors, can influence the development of obesity. Specifically, genes play a decisive role under the permissive circumstances of an obesogenic environment (increase in energy intake with a decrease in physical activity). Given the many factors that influence obesity, as well as the dynamic nature of this health problem (weight gain, weight loss, weight maintenance, variability in body composition), genomic tools have been used to evaluate all possible contributions of genes to the obesity problem. In this report, we present recently discovered gene–diet interaction studies in human obesity. Although existing literature in this specific area is fairly limited, various investigations utilizing large cohorts corroborate the potential for personalized interventions that take into account genetic patterns.
Similar content being viewed by others
Introduction
Obesity has reached epidemic proportions in the industrialized world and in developing countries during the past three decades, and our genetic pool did not change in the same period. Instead, major changes have taken place in lifestyle that facilitate weight gain. One is an energy-dense diet and the other is reduced physical activity throughout the life cycle. This is why obesity is prevalent in adults and in children with documented risk factors for diabetes and cardiovascular disease early on [1]. Genes, though, are also involved in the development of obesity. Heritability of body weight is estimated at 40% to 70 % [2], with a typical estimate at 50 %, meaning that about one half of the variation in body weight within a population is attributed to genes. In recent years, our knowledge of obesity genes has increased impressively due to new technologies such as gene and genome-wide linkage studies [3••]. Still, the established obesogenic genes explain less than 2 % of interindividual variation in body mass index (BMI) [4••], which means that many more obesogenic loci remain to be identified.
The obesity epidemic is primarily an environmental problem. However, given the current environment, genes influence decisively the response to the environment. It is becoming more obvious that an environment that facilitates the expression of weight-gaining genes is part of the reason why in the same obesity-promoting environment, some people become overweight and others do not. A genetically mediated susceptibility to environmental exposure is known as a gene–environment interaction. Although more than 120 genes have been associated with weight gain or obesity, few have definitively been shown to interact with diet to modulate obesity outcomes in humans [5]. Even fewer are the examples of replicated evidence that is necessary to definitively demonstrate the scientific merit of these observations. Some research has revealed that genes may affect weight loss success [6]. The idea that in the future, clinicians will be able to assign the best diet for optimal weight loss after taking into consideration genotype pattern constitutes a very useful approach toward personalized nutrition.
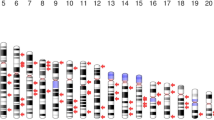
The purpose of this review is to present recently reported genotype–diet interactions that impact indices of obesity and to highlight evidence from studies that document the contribution of a genetic component in weight loss due to energy restriction. The majority of information comes from available epidemiologic and candidate gene studies. Genes that have been shown to participate in diet-related interaction studies of obesity include primarily MC4R, FTO, PPARG, APOA2, APOA5, and PLIN.
MC4R
There are obesogenic genes that are involved in neurohormonal pathways that often act on regulation of energy intake and expenditure [7]. Their primary influence seems to be on controlling appetite and satiety. The melanocortin-4-receptor (MC4R) gene is one such gene in which loss of function of the MC4R contributes to weight gain and obesity [8]. This receptor is widely expressed in the brain and is a protein made of 332 amino acids encoded by an exon on chromosome 18q22 [9]. More than 100 mutations in the human MC4R gene have been identified to date. Overall, associated features of mutations include hyperphagia, hyperinsulinemia, and increased fat mass [10]. Some defects in MC4R have been associated with monogenic obesity in which prevalence rates are fairly low (1 %–4 %) [11], but other mutations have been associated with common forms of polygenic obesity [12]. Mutations of the MC4R gene in combination with common variants of the FTO gene—another strong candidate gene for obesity—account for less than 2 % of the variance in the BMI of adults [13, 14]. Also, not all subjects carrying an MC4R weight-gaining mutation are overweight/obese. Taken together, this suggests that the interplay between other unknown genes and/or environmental factors could be important for the development of obesity.
Specific information on MC4R gene–diet interactions is available from animal studies. The first gene–diet interaction involving an MC4R mutation and weight gain showed that the homozygous mutated mice were hyperphagic only when fed a high-fat diet, and not when fed a low-fat diet when compared with the homozygous wild-type mice [15]. A recent study supported that subjects carrying MC4R mutations not only consume higher amounts of energy but also engage in a significantly higher consumption of specific nutrients, namely fat and saturated fat [16]. At this time, the specific mechanisms by which MC4R mutations lead to weight gain remain unknown. Nevertheless, the documented preference of subjects carrying an MC4R mutation for energy-dense food choices—including foods high in fat—should be explored further.
FTO
To date, the fat mass and obesity associated (FTO) gene is the first and most robust gene contributing to common forms of human obesity [14]. Recent studies support that the FTO locus increases obesity risk through increasing energy intake and fat intake [17–19] as well as reducing satiety [20] in various ages.
The FTO gene is situated on chromosome 16 and is made up of nine exons taking up at least 400 kb. Several FTO single nucleotide polymorphisms (SNPs) have been identified, all located on the first intron of the gene, a region on which the sequence is heavily maintained across species [14, 21, 22]. The FTO gene encodes the enzyme 2-oxoglutarate-dependent nucleic acid demethylase, which is found in the nucleus. The function of this enzyme remains to be determined, yet accumulating evidence supports its involvement in eating behavior, satiety, and dietary intake [23]. The most researched SNP is the rs9939609 T > A, which has been related to a higher body weight and higher risk of obesity in several populations across the world [23].
It has been hypothesized that the FTO gene might interact with diet to boost obesity. In this context, variations of the FTO gene have been the focus of recent studies on gene–diet interactions (Table 1). The rs9939609 SNP is again the most studied in relation to lifestyle factors. In a cross-sectional study, Sonestedt and colleagues [24] reported that fat and carbohydrate intake modifies the association between the rs9939609 variant of the FTO and obesity. Also, an intervention study was carried out in a sample of high cardiovascular risk adults aged 55 to 80 years [25]. After 3 years of intervention with the Mediterranean diet, subjects carrying the A allele of the mutation gained significantly less weight compared with wild-type subjects (TT). Recently, Moleres et al. [26] reported that in children, risk allele carriers who consume saturated fat that exceeds 12.6 % of energy had an increased obesity risk compared with all others. Similarly, Corella and colleagues [27] discovered in two large US adult cohorts that homozygous participants of the risk allele had a higher BMI compared with the other genotypes only when they consumed a high amount of saturated fat. Interestingly, in two Greek cohorts of 3,512 children [28•], breastfeeding exerted a protective effect on the relationship between risk allele carriers of FTO and indices of obesity. In the same investigation, these findings were not replicated in the British cohort (n = 4,325). In light of accumulating evidence [25–27], it is possible that a Mediterranean-type diet, inherently lower in saturated fat, consumed by the Greek nursing mothers blunted the obesogenic effect of FTO in comparison to the British counterparts, who presumably consumed a more Western-type diet. In contrast, the Finnish Diabetes Prevention study [29] failed to detect any FTO gene–diet interaction on obesity. Taken together, available results suggest that the BMI-increasing effect of FTO may be enhanced by a Westernized diet characterized by high energy density and abundant intakes of total and saturated fat. The mechanism explaining this suggested gene–environment interaction remains to be fully described as new information becomes available.
PPARG
The human peroxisome proliferator–activated receptor gamma (PPARG) plays a key role in the regulation of lipid and glucose homeostasis, differentiation of adipocytes, lipid storage, and insulin sensitization [30]. Due to its central role in macronutrient metabolism, this gene has been studied extensively for its possible involvement in obesity [31, 32], with a number of studies focused on the discovery of significant gene–environment interactions (Table 1). The coding region of the PPARG gene includes one common polymorphism (Pro12Ala) in addition to 16 rare missense and nonsense mutations [33]. The common polymorphism (Pro12Ala) has been studied the most for a variety of chronic diseases, including obesity, and related metabolic disorders such as type 2 diabetes mellitus and hyperlipidemias. It has been shown that the receptor expressing the risk allele has a reduced DNA-binding affinity, reduced transcriptional activity, and impaired activity in target genes, including a reduced release of free fatty acids [34]. Interestingly, both activation of PPRG by thiazolidinediones and reduced transcriptional activity of PPRG due to the common polymorphism (Pro12Ala) have been associated with improved insulin sensitivity [35]. Overall, the biological importance of the mutation is not fully understood, and the risk allele (12Ala) has not consistently been shown to increase obesity risk. Indeed, several studies report positive, negative, and null associations [31]. This variation suggests a heterogeneity of the effect. It is possible then that the common SNP (Pro12Ala) interacts with other factors to influence obesity outcomes; one such factor could be diet.
In humans, several studies have investigated the interaction between PPARG Pro12Ala polymorphism and diet with respect to obesity. Some studies suggest that Ala allele carriers may be more sensitive to the composition of the diet than Pro/Pro homozygotes, while other studies indicate the reverse. One study has reported on the relationship between the Pro12Ala variant and carbohydrate intake [36]: specifically, Ala12 carriers had an increased risk of obesity when consuming an excess of 49 % of energy as carbohydrates. Apart from this one study on carbohydrate consumption, the majority of Pro12Ala variant–diet interaction studies have focused on fat intake. According to structural research [37], free fatty acids bind and activate the PPARG transcription factor, suggesting a rather direct impact of fat intake on the gene’s activity. This plausible mechanism has led to several relevant studies. Luan et al. [38] reported that a low dietary polyunsaturated fatty acid (PUFA) to saturated fatty acid (SFA) ratio is associated with higher BMI in Ala carriers compared with Pro homozygotes, with the opposite effect for a high PUFA/SFA ratio. Also, Franks et al. [39] found that carriers of the mutant Ala12 allele who had a high PUFA/SFA ratio and were physically active had a lower fasting insulin concentration. In a case-control study, Nieters et al. [40] showed that Ala12 carriers who consumed higher quantities of arachidonic acid were at higher risk of obesity. In a French-Canadian population, Robitaille and colleagues [41] reported a Pro12Ala–fat interaction on waist circumference. Specifically, the homozygotes for the Pro allele had a significantly higher waist circumference if they consumed higher amounts of total fat or saturated fat, but this was not evident in Ala12 carriers. In the same population [41], an interaction between the Ala12 variant and total fat intake was identified as leading to a higher BMI. Also, in a subsample of the Health Nurses’ Study [42], investigators revealed a significant interaction between total fat intake, the Pro12Ala, and BMI. In this case, among homozygous Pro subjects, those who were categorized in the highest quintile of total fat intake were found to have a significantly higher BMI compared with their counterparts in the lowest quintile. In the same study [42], intake of monounsaturated fat was inversely associated with BMI among 12Ala allele carriers. This gene–diet interaction between the PPARG genotype and monounsaturated fatty acid (MUFA) intake on obesity was replicated in a weight loss study [43]. In this intervention that used the Mediterranean diet as its dietary treatment, it was found that obesity was attenuated in carriers of the Ala12 allele only in subjects with a high MUFA consumption (≥56 % of total fat intake). Also, a study of a healthy population showed that a low intake of monounsaturated fats by obese 12Ala carriers was associated with significantly higher insulin resistance [44]. The results of a another intervention trial showed that adherence to the Mediterranean diet for 2 years was inversely associated with waist circumference in carriers of the mutant 12Ala allele, especially in type 2 diabetics [45]. Furthermore, for the 12Ala carriers randomly assigned to the low-fat diet control group of the same intervention study [45], waist circumference was significantly higher when compared with wild-type participants in the control group.
Recently, Anderson et al. [46] discovered an interaction between dietary patterns and the PPARG Pro12Ala genotype on body composition. Pro/Pro homozygous males and females consuming a healthy food pattern did not differ in body composition from their counterparts consuming other food patterns. On the other hand, male carriers of the Ala allele consuming a healthy food pattern had significantly lower levels of adiposity than those consuming the rest of identified food patterns. Women with the Ala allele who consumed the healthy food pattern differed only in thigh intermuscular fat compared with women eating the rest of the food patterns. Similarly, a pediatric study reported on a diet-modified effect of the PPARG polymorphism influenced by age and gender [47]. The researchers showed that in Pro/Pro homozygous young girls, saturated fat and total fat intake were positively associated with higher BMI, waist circumference, and skinfold thickness measurements. For Pro/Pro homozygotes, unsaturated fat intake was inversely associated with BMI in young girls and positively with BMI, waist circumference, and triceps skinfold in periadolescent boys. Taken together, these results in adults [47] and children [47] suggest that adiposity is influenced by the Pro12Ala polymorphism in a sex-specific and age-dependent manner. The evidence of these gene–diet interactions also suggests that diet and type of fat intake modify the effect of the Pro12 allele on obesity-related measures, yet their specific impact is not clear from studies to date.
Previous studies have found interactions between diet and PPARG Pro12Ala genotype in relation to weight change, but results have been inconsistent. A study by Lindi et al. [48], reported on the importance of the Pro12Ala polymorphism and diet on weight loss. This was a 3-year longitudinal trial of subjects with impaired glucose tolerance who were randomly assigned to an intensive exercise and diet intervention aimed at lowering total fat consumption, or a control group. The main outcome was that homozygous Ala/Ala individuals in the intervention arm lost significantly more weight than all others in the intervention. These results suggest that the negative impact of Ala may be circumvented to an extent due to sustained improvements in diet and physical activity. Also, Ala allele carriers in the weight loss lifestyle intervention group of the Diabetes Prevention Program lost more weight compared with the wild-type Pro homozygotes [39]. On the other hand, another weight loss study by Adamo and colleagues [49] showed that the Ala allele was related to significant weight loss resistance in obese women who were placed on a 900-kcal diet. This was supported by the findings of Garaulet et al. [43], who reported that when total fat intake was high, Ala12 carriers lost a significantly lower percentage of body weight than Pro carriers. Finally, in a hypocaloric study of overweight women [50], although weight loss did not differ by genotype, weight regain during follow-up was greater in Ala carriers.
APOA2
The apolipoprotein A-2 (APOA2) gene codes for the second major high-density lipoprotein apolipoprotein and is a member of the apolipoprotein multigene family (APO1, APOA2, and APOA4). The APOA2 gene is located on chromosome 1 within the cytogenetic band q23.3 [51]. The functions of the APOA2 protein appear to be fairly complex, with evidence that it plays a central role in regulating fatty acid and triglyceride metabolism [52]. Still, the complete range of its functions is largely undetermined. Animal models show that overexpression of APOA2 results in high concentrations of triglycerides, increased adiposity, weight gain, and insulin resistance [53–56], but the physiologic role of APOA2 in humans is less clear due to conflicting results [57–59].
Recently, studies of the APOA2 gene have shown that the APOA2 –265 T > C polymorphism interacts with a high saturated fat diet to enhance weight gain and obesity (Table 1). The first study to show a role for APOA2 in regulating food intake and satiety was the Genetics of Lipid Lowering Drugs and Diet Network (GOLDN), which included 1,078 subjects [60]. In this investigation, CC individuals were found to consume increased amounts of fat and protein and to present with a significantly higher body weight, BMI, and waist circumference compared with T carriers. In a subsequent report [61], 3,462 individuals were investigated from 3 different populations (Framingham Offspring Study (n = 1,454), GOLDN (n = 1,078), and Boston-Puerto Rican Centers on Population Health and Health Disparities Study (n = 903). In these three independent samples, it was shown that CC individuals consuming a high saturated fat diet (≥22 g/d) had a 6.2 % higher BMI compared with all other genotypes. There were no differences in BMI among genotypes for all individuals who consumed a low saturated fat diet. The same finding was replicated by a study of 4,602 participants [62] using two other samples, one from the Mediterranean (907 adults) and one from various Asian backgrounds (2,506 Chinese, 605 Malaysian, and 494 Asian-Indian adults). In both these populations, the results showed that homozygous CC subjects had a statistically significant higher BMI (by 6.8 %) only if they consumed an excess of saturated fat (≥22 g/d) when compared with CT and TT subjects. Also, Smith et al. [63•] showed in 1,225 overweight and obese adults that CC subjects consuming a high saturated fat diet (≥20.7 g/d) had a significantly higher waist circumference than all other genotypes in the high saturated fat stratum. At the same time, in the lower saturated fat stratum, there were no differences in waist circumference among any genotype. These repeated findings from unrelated large populations constitute the first consistent replication evidence of a gene–diet interaction (between the APOA2 –265 T > C polymorphism and high saturated fat consumption) that promotes weight gain and a higher body weight. Although the mechanism leading to a higher weight is unknown, the APOA2 –265 T > C SNP has been associated with specific weight-gaining eating behaviors (eg, meal skipping and lack of meal planning) and dietary modulation of plasma ghrelin mediated by consumption of saturated fat [63•]. Smith et al. [63•] showed that ghrelin concentration of CC subjects consuming a low saturated fat diet was significantly lower compared with CC subjects consuming a high saturated fat diet, with TT and TC subjects consuming a low saturated fat diet, and with TT and TC subjects consuming a high saturated fat diet. Understanding these types of intermediate processes that are driven by gene–diet interactions could be crucial in planning effective personalized behavioral changes for obesity prevention and management (Fig. 1).
APOA5
Apolipoprotein A5 is a molecule that influences plasma triglyceride (TG) concentration in humans. It received its name due to its homology with APOA4 and from binding to HDL and other lipoproteins The gene encoding for APOA5 is located on chromosome 11q23 and is present in the APOA1-C3-A4 gene cluster. Several SNPs in the APOA5 gene are associated with increased TG levels in humans, and some nonsense mutations affecting protein structure predispose for familial hypertriglyceridemia and late-onset chylomicronemia [64]. The specific mechanism by which APOA5 acts is essentially unknown. However, the activation of lipoprotein lipase (LPL) is one possible scenario that is thought to lead to hypotriglyceridemia [65]. LPL may be involved in increased weight gain [66]. Also, some of the known regulators of the APOA5 gene may be obesogenic, including perixosome proliferator-activated receptors PPARs, as well as insulin and thyroid hormones [67, 68].
In this sense, there has been interest in discovering possible gene–diet interactions that involve APOA5 common variants. In a fat-restriction weight loss study of 606 overweight men with hyperlipidemia [69], it was demonstrated that BMI reduction was significantly higher in C allele carriers of the -1131 T > C variant of the APOA5 gene. In that study, it was concluded that because the polymorphism increases risk of coronary artery disease, a restriction diet is an important therapeutic modality for C carriers. The Framingham study has been used several times to investigate interactions of the APOA5 gene. Elosua and colleagues [70] showed in the Framingham study a gene–diet interaction between the -1131 T > C variant of the APOA5 gene and PUFAs on plasma lipid concentrations and particle size. It was also shown in the Framingham cohort [71] that obesity influences the effect of the APOA5 variant on carotid intimal medial thickness, which is a reliable proxy measure of atherosclerosis. This association was significant despite adjustment for TG concentration [71]. Again in the same cohort [72], a dose-dependent gene–diet interaction was detected involving the APOA5 variant -1131 T > C, fat intake, and obesity risk. Based on the results of this study, carriers of the mutant C allele, independent of high TG concentrations, had a lower likelihood of being obese when consuming a high monounsaturated fat diet when compared with individuals who were homozygous for the wild-type T allele. The same group tested the interaction in a Mediterranean population [73]. In this case, consistent with the previous gene–diet interaction identified in the Framingham cohort [72], the authors reported that participants homozygous for the T major allele had a positive association between fat intake and obesity, and in those who were carriers of the minor C allele, a higher fat intake was not associated with a higher BMI. Taken together, these data support the hypothesis that the C allele may protect those consuming a high-fat diet from obesity [72, 73].
PLIN
A growing body of evidence is in support of PLN1 as an important gene candidate for obesity and insulin resistance [74]. It has been suggested that in addition to its potential use in identifying high-risk individuals, this locus may be a key “switch” to reducing obesity through behavioral interventions such as diet [74]. Research on perilipin expression in humans has reported elevated concentrations of perilipin in obese people [75]. The gene encoding for human perilipin resides on chromosome 15q26 in the region of a linkage locus for obesity, diabetes, and hypertriglyceridemia [76–78]. Perilipins are a group of phosphorylated proteins found at the surface of fat cells. Studies have shown that these proteins are necessary in regulating triglyceride storage and mobilization from fat cells [79, 80]. These protein functions have prompted research involving PLIN polymorphisms on obesity indices.
In a 1-year randomized weight loss trial, Corella et al. [81] showed that A carriers of the 11482 G > A mutation at the perilipin locus were the least successful in losing weight. It was concluded that taking into account this polymorphism may predict body weight reduction success in low-energy interventions. Similarly, in another weight loss study that lasted 12 weeks, the subjects were placed on a calorie restriction study (~300 kcal/d) [82]. The results indicated that variation at the PLIN locus was associated with reduction in abdominal fat following weight loss. In a recent 12-week energy restriction intervention study of 78 obese women [83], the impact of PLIN1 polymorphisms (PLIN1 11482 G > A and PLIN1 13041 A > G) on body composition, energy and substrate metabolism, and metabolic response was assessed. In this study, consistent with the earlier findings of Corella et al. [81], women carriers of the A allele experienced a lesser reduction in waist circumference when compared with non–A allele carriers. The PLIN1 13041 A > G polymorphism did not show any effect of interaction. A significant gene–diet interaction between the PLIN11482G > A polymorphism and complex carbohydrate intake was identified in a cohort of 920 adults [84]. Results showed that among those subjects who consumed a high amount of complex carbohydrates (≥144 g/d), carriers of the minor allele had a smaller waist and hip circumferences compared with the homozygotes of the major allele. On the other hand, for those consuming complex carbohydrates less than 144 g/d, minor allele carriers had a larger waist circumferences compared with the rest. This type of interaction could be important in the dietary management of high body weight.
PLN4 is also a member of the lipid storage proteins. A meta-analysis of two populations of European ancestry was combined to reveal a significant interaction between the minor allele of the rs8887 PLN4 polymorphism and high intakes of PUFA n-3 fatty acids in reducing obesity-related phenotypes, including BMI and waist circumference [85••]. This was not evident in non-carriers of the minor allele. Although most of the work in perilipin proteins has focused on PLIN1, it is reassuring that both loci PLIN1 and PLIN4 appear to be regulated by polyunsaturated fats similarly. Replication studies in this area are necessary to help clarify the role of perilipin genes interacting with dietary fats on various obesity-related traits.
Conclusions and Future Directions
The present review highlights recent findings that increase our understanding of the relationship between genes and diet that can impact obesity. Data from gene–diet interactions are difficult to interpret. Unknown confounding factors may be the reason gene–diet interaction studies are not easily replicated in different populations. Thus, questions regarding validity are not fully addressed. Larger collaborations that increase the ethnic and geographic diversity, the size of samples, and the number of variables assessed will improve the probability of identifying important obesogenic relationships.
Even though the existing literature is not large, it seems to support that gene–diet interactions have a role in obesity outcomes. Genes that have been implicated thus far are related to appetite control (MC4R, FTO) and lipid metabolism (PPARG, APOA2, APOA5, PLIN1, PLIN). As more susceptibility genes are identified, it is likely that our knowledge of gene–diet interactions on obesity will be enriched. Of great interest is that eating behaviors may be the end result of gene–diet interactions, as has been discovered in the APOA2 gene (Fig. 1). Despite these exciting new areas of research, available data are not yet adequate to justify public genetic screening. The most effective way to prevent and manage a high body weight is through efficacious behavioral changes to achieve realistic energy deficits. Until the complete puzzle is solved, it is important to be cognizant that in any overweight group, there will be individuals who will respond less well or not at all to the dietary treatment of obesity due to genetic variability.
Incorporating genetic information into dietary trials may help reduce intraindividual variability in weight loss. Identifying subsets that would benefit from boosting or limiting the intake of a specific nutrient could aid in giving nutritional advice specific to individuals according to their genetic profile.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Papoutsakis C, Vidra NV, Hatzopoulou I, et al. The Gene-Diet Attica Investigation on childhood obesity (GENDAI): overview of the study design. Clin Chem Lab Med. 2007;45(3):309–15.
Allison DB, Kaprio J, Korkeila M, Koskenvuo M, Neale MC, Hayakawa K. The heritability of body mass index among an international sample of monozygotic twins reared apart. Int J Obes Relat Metab Disord. 1996;20(6):501–6.
•• Speliotes EK, Willer CJ, Berndt SI, et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat Genet. 2010;42(11):937–48. This is one of the largest association studies that identified obesogenic genes in more than 100,000 individuals.
•• Loos RJ. Recent progress in the genetics of common obesity. Br J Clin Pharmacol. 2009;68(6):811–29. This is a thorough review of obesity genetics.
Papoutsakis C, Dedoussis GV. Gene diet interactions in childhood obesity: paucity of evidence as the epidemic of childhood obesity continues to rise. Personalized Medicine. 2007;4(2):133–46.
Martinez JA, Parra MD, Santos JL, Moreno-Aliaga MJ, Marti A, Martinez-Gonzalez MA. Genotype-dependent response to energy-restricted diets in obese subjects: towards personalized nutrition. Asia Pac J Clin Nutr. 2008;17 Suppl 1:119–22.
Schwartz MW, Woods SC, Porte Jr D, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404(6778):661–71.
Young EH, Wareham NJ, Farooqi S, et al. The V103I polymorphism of the MC4R gene and obesity: population based studies and meta-analysis of 29 563 individuals. Int J Obes (Lond). 2007;31(9):1437–41.
Tao YX, Segaloff DL. Functional characterization of melanocortin-4 receptor mutations associated with childhood obesity. Endocrinology. 2003;144(10):4544–51.
Farooqi IS. Monogenic human obesity syndromes. In: A. Kalsbeek EF, M.A. Hofman, D.F. Swaab, E.J.W. van Someren and R.M. Buijs, ed. Hypothalamic Integration of Energy Metabolism, Proceedings of the 24th International Summer School of Brain Research, held at the Royal Netherlands Academy of Arts and Sciences. Volume 153 ed: Elsevier; 2006:119–125.
Vaisse C, Clement K, Durand E, Hercberg S, Guy-Grand B, Froguel P. Melanocortin-4 receptor mutations are a frequent and heterogeneous cause of morbid obesity. J Clin Invest. 2000;106(2):253–62.
Willer CJ, Speliotes EK, Loos RJ, et al. Six new loci associated with body mass index highlight a neuronal influence on body weight regulation. Nat Genet. 2009;41(1):25–34.
Loos RJ, Lindgren CM, Li S, et al. Common variants near MC4R are associated with fat mass, weight and risk of obesity. Nat Genet. 2008;40(6):768–75.
Frayling TM, Timpson NJ, Weedon MN, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007;316(5826):889–94.
Butler AA, Cone RD. Knockout studies defining different roles for melanocortin receptors in energy homeostasis. Ann N Y Acad Sci. 2003;994:240–5.
Bauer F, Elbers CC, Adan RA, et al. Obesity genes identified in genome-wide association studies are associated with adiposity measures and potentially with nutrient-specific food preference. Am J Clin Nutr. 2009;90(4):951–9.
Cecil JE, Watt P, Palmer CN, Hetherington M. Energy balance and food intake: the role of PPARgamma gene polymorphisms. Physiol Behav. 2006;88(3):227–33.
Timpson NJ, Emmett PM, Frayling TM, et al. The fat mass- and obesity-associated locus and dietary intake in children. Am J Clin Nutr. 2008;88(4):971–8.
Wardle J, Llewellyn C, Sanderson S, Plomin R. The FTO gene and measured food intake in children. Int J Obes (Lond). 2009;33(1):42–5.
Wardle J, Carnell S, Haworth CM, Farooqi IS, O’Rahilly S, Plomin R. Obesity associated genetic variation in FTO is associated with diminished satiety. J Clin Endocrinol Metab. 2008;93(9):3640–3.
Dina C, Meyre D, Gallina S, et al. Variation in FTO contributes to childhood obesity and severe adult obesity. Nat Genet. 2007;39(6):724–6.
Scuteri A, Sanna S, Chen WM, et al. Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS Genet. 2007;3(7):e115.
Loos RJ, Bouchard C. FTO: the first gene contributing to common forms of human obesity. Obes Rev. 2008;9(3):246–50.
Sonestedt E, Roos C, Gullberg B, Ericson U, Wirfalt E, Orho-Melander M. Fat and carbohydrate intake modify the association between genetic variation in the FTO genotype and obesity. Am J Clin Nutr. 2009;90(5):1418–25.
Razquin C, Martinez JA, Martinez-Gonzalez MA, Bes-Rastrollo M, Fernandez-Crehuet J, Marti A. A 3-year intervention with a Mediterranean diet modified the association between the rs9939609 gene variant in FTO and body weight changes. Int J Obes (Lond). 2010;34(2):266–72.
Moleres A, Ochoa MC, Rendo-Urteaga T, et al. Dietary fatty acid distribution modifies obesity risk linked to the rs9939609 polymorphism of the fat mass and obesity-associated gene in a Spanish case-control study of children. Br J Nutr. 2012;107(4):533–8.
Corella D, Arnett DK, Tucker KL, et al. A high intake of saturated fatty acids strengthens the association between the fat mass and obesity-associated gene and BMI. J Nutr. 2011;141(12):2219–25.
• Dedoussis GV, Yannakoulia M, Timpson NJ, et al. Does a short breastfeeding period protect from FTO-induced adiposity in children? Int J Pediatr Obes. 2011;6(2-2):e326–335. This study is one of the few that has shown a role for breastfeeding in a gene–diet interaction context.
Lappalainen T, Lindstrom J, Paananen J, et al. Association of the fat mass and obesity-associated (FTO) gene variant (rs9939609) with dietary intake in the Finnish Diabetes Prevention Study. Br J Nutr. 2012;1–7.
Spiegelman BM. Peroxisome proliferator-activated receptor gamma: a key regulator of adipogenesis and systemic insulin sensitivity. Eur J Med Res. 1997;2(11):457–64.
Masud S, Ye S. Effect of the peroxisome proliferator activated receptor-gamma gene Pro12Ala variant on body mass index: a meta-analysis. J Med Genet. 2003;40(10):773–80.
Tonjes A, Scholz M, Loeffler M, Stumvoll M. Association of Pro12Ala polymorphism in peroxisome proliferator-activated receptor gamma with Pre-diabetic phenotypes: meta-analysis of 57 studies on nondiabetic individuals. Diabetes Care. 2006;29(11):2489–97.
Jeninga EH, Gurnell M, Kalkhoven E. Functional implications of genetic variation in human PPARgamma. Trends Endocrinol Metab. 2009;20(8):380–7.
Deeb SS, Fajas L, Nemoto M, et al. A Pro12Ala substitution in PPARgamma2 associated with decreased receptor activity, lower body mass index and improved insulin sensitivity. Nat Genet. 1998;20(3):284–7.
Yamauchi T, Kamon J, Waki H, et al. The mechanisms by which both heterozygous peroxisome proliferator-activated receptor gamma (PPARgamma) deficiency and PPARgamma agonist improve insulin resistance. J Biol Chem. 2001;276(44):41245–54.
Marti A, Corbalan MS, Martinez-Gonzalez MA, Forga L, Martinez JA. CHO intake alters obesity risk associated with Pro12Ala polymorphism of PPARgamma gene. J Physiol Biochem. 2002;58(4):219–20.
Xu HE, Lambert MH, Montana VG, et al. Molecular recognition of fatty acids by peroxisome proliferator-activated receptors. Mol Cell. 1999;3(3):397–403.
Luan J, Browne PO, Harding AH, et al. Evidence for gene-nutrient interaction at the PPARgamma locus. Diabetes. 2001;50(3):686–9.
Franks PW, Jablonski KA, Delahanty L, et al. The Pro12Ala variant at the peroxisome proliferator-activated receptor gamma gene and change in obesity-related traits in the Diabetes Prevention Program. Diabetologia. 2007;50(12):2451–60.
Nieters A, Becker N, Linseisen J. Polymorphisms in candidate obesity genes and their interaction with dietary intake of n-6 polyunsaturated fatty acids affect obesity risk in a sub-sample of the EPIC-Heidelberg cohort. Eur J Nutr. 2002;41(5):210–21.
Robitaille J, Despres JP, Perusse L, Vohl MC. The PPAR-gamma P12A polymorphism modulates the relationship between dietary fat intake and components of the metabolic syndrome: results from the Quebec Family Study. Clin Genet. 2003;63(2):109–16.
Memisoglu A, Hu FB, Hankinson SE, et al. Interaction between a peroxisome proliferator-activated receptor gamma gene polymorphism and dietary fat intake in relation to body mass. Hum Mol Genet. 2003;12(22):2923–9.
Garaulet M, Smith CE, Hernandez-Gonzalez T, Lee YC, Ordovas JM. PPARgamma Pro12Ala interacts with fat intake for obesity and weight loss in a behavioural treatment based on the Mediterranean diet. Mol Nutr Food Res. 2011;55(12):1771–9.
Soriguer F, Morcillo S, Cardona F, et al. Pro12Ala polymorphism of the PPARG2 gene is associated with type 2 diabetes mellitus and peripheral insulin sensitivity in a population with a high intake of oleic acid. J Nutr. 2006;136(9):2325–30.
Razquin C, Alfredo Martinez J, Martinez-Gonzalez MA, Corella D, Santos JM, Marti A. The Mediterranean diet protects against waist circumference enlargement in 12Ala carriers for the PPARgamma gene: 2 years’ follow-up of 774 subjects at high cardiovascular risk. Br J Nutr. 2009;102(5):672–9.
Anderson AL, Harris TB, Houston DK, et al. Relationships of dietary patterns with body composition in older adults differ by gender and PPAR-gamma Pro12Ala genotype. Eur J Nutr. 2010;49(7):385–94.
Dedoussis GV, Manios Y, Kourlaba G, et al. An age-dependent diet-modified effect of the PPARgamma Pro12Ala polymorphism in children. Metabolism. 2011;60(4):467–73.
Lindi VI, Uusitupa MI, Lindstrom J, et al. Association of the Pro12Ala polymorphism in the PPAR-gamma2 gene with 3-year incidence of type 2 diabetes and body weight change in the Finnish Diabetes Prevention Study. Diabetes. 2002;51(8):2581–6.
Adamo KB, Dent R, Langefeld CD, et al. Peroxisome proliferator-activated receptor gamma 2 and acyl-CoA synthetase 5 polymorphisms influence diet response. Obesity (Silver Spring). 2007;15(5):1068–75.
Nicklas BJ, van Rossum EF, Berman DM, Ryan AS, Dennis KE, Shuldiner AR. Genetic variation in the peroxisome proliferator-activated receptor-gamma2 gene (Pro12Ala) affects metabolic responses to weight loss and subsequent weight regain. Diabetes. 2001;50(9):2172–6.
Eisenberg S. High density lipoprotein metabolism. J Lipid Res. 1984;25(10):1017–58.
Kalopissis AD, Pastier D, Chambaz J. Apolipoprotein A-II: beyond genetic associations with lipid disorders and insulin resistance. Curr Opin Lipidol. 2003;14(2):165–72.
Castellani LW, Goto AM, Lusis AJ. Studies with apolipoprotein A-II transgenic mice indicate a role for HDLs in adiposity and insulin resistance. Diabetes. 2001;50(3):643–51.
Castellani LW, Nguyen CN, Charugundla S, et al. Apolipoprotein AII is a regulator of very low density lipoprotein metabolism and insulin resistance. J Biol Chem. 2008;283(17):11633–44.
Weng W, Breslow JL. Dramatically decreased high density lipoprotein cholesterol, increased remnant clearance, and insulin hypersensitivity in apolipoprotein A-II knockout mice suggest a complex role for apolipoprotein A-II in atherosclerosis susceptibility. Proc Natl Acad Sci U S A. 1996;93(25):14788–94.
Wuschke S, Dahm S, Schmidt C, Joost HG, Al-Hasani H. A meta-analysis of quantitative trait loci associated with body weight and adiposity in mice. Int J Obes (Lond). 2007;31(5):829–41.
van Hooft FM, Ruotolo G, Boquist S, de Faire U, Eggertsen G, Hamsten A. Human evidence that the apolipoprotein a-II gene is implicated in visceral fat accumulation and metabolism of triglyceride-rich lipoproteins. Circulation. 2001;104(11):1223–8.
Lara-Castro C, Hunter GR, Lovejoy JC, Gower BA, Fernandez JR. Apolipoprotein A-II polymorphism and visceral adiposity in African-American and white women. Obes Res. 2005;13(3):507–12.
Delgado-Lista J, Perez-Jimenez F, Tanaka T, et al. An apolipoprotein A-II polymorphism (-265T/C, rs5082) regulates postprandial response to a saturated fat overload in healthy men. J Nutr. 2007;137(9):2024–8.
Corella D, Arnett DK, Tsai MY, et al. The -256 T > C polymorphism in the apolipoprotein A-II gene promoter is associated with body mass index and food intake in the genetics of lipid lowering drugs and diet network study. Clin Chem. 2007;53(6):1144–52.
Corella D, Peloso G, Arnett DK, et al. APOA2, dietary fat, and body mass index: replication of a gene-diet interaction in 3 independent populations. Arch Intern Med. 2009;169(20):1897–906.
Corella D, Tai ES, Sorli JV, et al. Association between the APOA2 promoter polymorphism and body weight in Mediterranean and Asian populations: replication of a gene-saturated fat interaction. Int J Obes (Lond). 2011;35(5):666–75.
• Smith CE, Ordovas JM, Sanchez-Moreno C, Lee YC, Garaulet M. Apolipoprotein A-II polymorphism: relationships to behavioural and hormonal mediators of obesity. Int J Obes (Lond). 2012;36(1):130–6. This study is one of the few in which eating behavior is shown to be the result of gene–diet interaction.
Pennacchio LA, Olivier M, Hubacek JA, et al. An apolipoprotein influencing triglycerides in humans and mice revealed by comparative sequencing. Science. 2001;294(5540):169–73.
Merkel M, Loeffler B, Kluger M, et al. Apolipoprotein AV accelerates plasma hydrolysis of triglyceride-rich lipoproteins by interaction with proteoglycan-bound lipoprotein lipase. J Biol Chem. 2005;280(22):21553–60.
Mead JR, Irvine SA, Ramji DP. Lipoprotein lipase: structure, function, regulation, and role in disease. J Mol Med (Berl). 2002;80(12):753–69.
Prieur X, Coste H, Rodriguez JC. The human apolipoprotein AV gene is regulated by peroxisome proliferator-activated receptor-alpha and contains a novel farnesoid X-activated receptor response element. J Biol Chem. 2003;278(28):25468–80.
Prieur X, Huby T, Coste H, Schaap FG, Chapman MJ, Rodriguez JC. Thyroid hormone regulates the hypotriglyceridemic gene APOA5. J Biol Chem. 2005;280(30):27533–43.
Aberle J, Evans D, Beil FU, Seedorf U. A polymorphism in the apolipoprotein A5 gene is associated with weight loss after short-term diet. Clin Genet. 2005;68(2):152–4.
Elosua R, Ordovas JM, Cupples LA, et al. Variants at the APOA5 locus, association with carotid atherosclerosis, and modification by obesity: the Framingham Study. J Lipid Res. 2006;47(5):990–6.
Lai CQ, Corella D, Demissie S, et al. Dietary intake of n-6 fatty acids modulates effect of apolipoprotein A5 gene on plasma fasting triglycerides, remnant lipoprotein concentrations, and lipoprotein particle size: the Framingham Heart Study. Circulation. 2006;113(17):2062–70.
Corella D, Lai CQ, Demissie S, et al. APOA5 gene variation modulates the effects of dietary fat intake on body mass index and obesity risk in the Framingham Heart Study. J Mol Med. 2007;85(2):119–28.
Sanchez-Moreno C, Ordovas JM, Smith CE, Baraza JC, Lee YC, Garaulet M. APOA5 gene variation interacts with dietary fat intake to modulate obesity and circulating triglycerides in a Mediterranean population. J Nutr. 2011;141(3):380–5.
Tai ES, Ordovas JM. The role of perilipin in human obesity and insulin resistance. Curr Opin Lipidol. 2007;18(2):152–6.
Kern PA, Di Gregorio G, Lu T, Rassouli N, Ranganathan G. Perilipin expression in human adipose tissue is elevated with obesity. J Clin Endocrinol Metab. 2004;89(3):1352–8.
Chagnon YC, Borecki IB, Perusse L, et al. Genome-wide search for genes related to the fat-free body mass in the Quebec family study. Metabolism. 2000;49(2):203–7.
Duggirala R, Blangero J, Almasy L, et al. A major susceptibility locus influencing plasma triglyceride concentrations is located on chromosome 15q in Mexican Americans. Am J Hum Genet. 2000;66(4):1237–45.
Mori Y, Otabe S, Dina C, et al. Genome-wide search for type 2 diabetes in Japanese affected sib-pairs confirms susceptibility genes on 3q, 15q, and 20q and identifies two new candidate Loci on 7p and 11p. Diabetes. 2002;51(4):1247–55.
Brasaemle DL, Rubin B, Harten IA, Gruia-Gray J, Kimmel AR, Londos C. Perilipin A increases triacylglycerol storage by decreasing the rate of triacylglycerol hydrolysis. J Biol Chem. 2000;275(49):38486–93.
Mottagui-Tabar S, Ryden M, Lofgren P, et al. Evidence for an important role of perilipin in the regulation of human adipocyte lipolysis. Diabetologia. 2003;46(6):789–97.
Corella D, Qi L, Sorli JV, et al. Obese subjects carrying the 11482 G > A polymorphism at the perilipin locus are resistant to weight loss after dietary energy restriction. J Clin Endocrinol Metab. 2005;90(9):5121–6.
Jang Y, Kim OY, Lee JH, et al. Genetic variation at the perilipin locus is associated with changes in serum free fatty acids and abdominal fat following mild weight loss. Int J Obes (Lond). 2006;30(11):1601–8.
Ruiz JR, Larrarte E, Margareto J, Ares R, Alkorta P, Labayen I. Preliminary findings on the role of PLIN1 polymorphisms on body composition and energy metabolism response to energy restriction in obese women. Br J Nutr. 2011;106(4):486–90.
Smith CE, Tucker KL, Yiannakouris N, et al. Perilipin polymorphism interacts with dietary carbohydrates to modulate anthropometric traits in hispanics of Caribbean origin. J Nutr. 2008;138(10):1852–8.
•• Richardson K, Louie-Gao Q, Arnett DK, et al. The PLIN4 variant rs8887 modulates obesity related phenotypes in humans through creation of a novel miR-522 seed site. PLoS One. 2011;6(4):e17944. This is an outstanding meta-analysis showing that microRNA mediates the gene–diet interaction related to obesity.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Papoutsakis, C. Gene–Diet Interactions and Obesity Indices. Curr Nutr Rep 1, 142–152 (2012). https://doi.org/10.1007/s13668-012-0019-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-012-0019-x