Abstract
Introduction
Alopecia areata (AA) is an autoimmune disease characterized by nonscarring hair loss involving the scalp, face, and/or body. Literature on the prevalence, patient characteristics, management approaches, and challenges faced by patients with AA across the Middle East is limited. Therefore, a greater understanding of the current AA landscape within the region is needed. This cross-sectional study surveyed dermatologists from four countries to assess dermatologists’ perspectives on the prevalence of AA within the Middle East, as well as patient characteristics, unmet needs, and management strategies.
Methods
This blinded, quantitative, observational study surveyed practicing dermatologists in Egypt, Lebanon, Saudi Arabia, and the United Arab Emirates. The survey was conducted between September 2021 and January 2022 and comprised 47 closed-ended, multiple-choice questions as well as Likert scale responses. These questions assessed the characteristics of physicians and the patients in their practices, physicians’ familiarity with treatment, and physicians’ treatment approaches.
Results
The estimated prevalence of AA varied across the region. Across all age groups treated for AA, the majority of patients had AA of mild severity (pediatric: 63%; adolescent: 60%; adult: 54%) and the scalp was reported as the most affected area (65%). Potent topical corticosteroids were the most frequently used treatment for mild to moderate and severe AA (92% and 78%, respectively). There was a lack of awareness of investigative treatments, with only 33% of dermatologists aware of these options. The greatest unmet needs in treating AA included long-term disease control, improved efficacy, faster onset of action, and better safety profiles (62%, 53%, 52%, and 51%, respectively).
Conclusions
This study provided insight into the diagnosis and management of AA in the Middle East. Treatment strategies were similar regardless of the severity of AA. Long-term disease control and improved efficacy and safety profiles were identified as key unmet needs in the treatment of AA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Published literature on the overall prevalence, patient characteristics, and treatment landscape for alopecia areata (AA) across the Middle East is limited. |
This blinded, quantitative, observational study surveyed practicing dermatologists across four countries in the Middle East to obtain a comprehensive understanding of the current AA landscape in the region. |
What was learned from this study? |
Treatment strategies for patients with AA were similar regardless of the severity of the disease; potent topical corticosteroids were the most frequently prescribed treatment for both mild to moderate and severe AA. |
Overall, there was a lack of familiarity among dermatologists on the use of investigative treatments, particularly Janus kinase (JAK) inhibitors. Key unmet needs for AA treatment included long-term disease control, faster onset, and improved efficacy and safety profiles. |
As the AA treatment landscape continues to evolve, further education on novel treatments is warranted to inform clinical decision-making and ensure optimal treatment for patients with AA across the Middle East. |
Introduction
Alopecia areata (AA) is an autoimmune disease that has underlying immuno-inflammatory pathogenesis and is characterized by nonscarring hair loss ranging from small bald patches to complete loss of scalp, face, and/or body hair [1]. Approximately 10% to 35% of patients with AA will progress to more extensive forms of AA, including alopecia totalis (AT [complete loss of scalp hair]) or alopecia universalis (AU [complete loss of scalp, face, and body hair]) [2, 3]. Hair loss with AA is unpredictable, and patients may experience relapse and remission or persistence of the condition [4, 5].
The global prevalence of AA has been estimated at approximately 2% [6], with both male and female adults and children affected and with no significant differences across ethnicities [7, 8]. Patients with AA may experience psychological and psychosocial symptoms that may have a negative impact on their quality of life (QOL) [9,10,11,12,13,14,15,16], including feelings of low self-esteem, depression, and other mental health issues. Additionally, AA can have a functional impact on a patient’s career, relationships, and education. Patients with AA are more likely to present with other autoimmune comorbidities, such as atopic dermatitis (AD), vitiligo, psoriasis, and thyroid disease [17].
Current treatment options for AA include topical, intralesional, and systemic corticosteroids; topical calcineurin inhibitors, prostaglandin analogues, and minoxidil; systemic cyclosporine, methotrexate, and azathioprine; and phototherapy. However, response to current therapies varies, and disease relapse in patients is frequent, so there is a need for new effective treatments. The underlying pathogenesis of AA involves multiple cytokines, including interferon-gamma (IFN-γ) and interleukin (IL)-15, boh of which signal through Janus kinases (JAKs) [18]; this discovery has led to the investigation of JAK inhibitors for the treatment of AA. Several JAK inhibitors are currently under investigation, and recent data from clinical trials support their use in the treatment of AA [19,20,21,22,23]. Baricitinib demonstrated significant hair regrowth in two phase 3 trials and has since been approved for the treatment of adults with severe AA by the US Food and Drug Administration (FDA) and European Medicines Agency (EMA) [24,25,26,27]. Ritlecitinib, an oral JAK3/TEC family kinase inhibitor, has also demonstrated efficacy and safety in patients aged ≥ 12 years with AA. [20, 21].
A wide diversity of ethnicities and socioeconomic conditions can be found across the countries of the Middle East. However, although a few studies have been conducted to understand the distribution of AA in Saudi Arabia [28, 29], the literature is limited regarding the overall prevalence, patient characteristics, and treatment patterns in AA across the Middle East. As the treatment landscape for AA continues to evolve, a current and more detailed understanding of the population of patients with AA, management approaches, and challenges faced by dermatologists in these countries is warranted. This study aimed to investigate dermatologists’ perspectives of the prevalence and clinical characteristics of patients with AA, as well as current treatment plans and management strategies used, across four selected countries in the Middle East.
Methods
Study Design
This was a blinded, quantitative, observational, cross-sectional study of dermatologists practicing in Egypt, Lebanon, Saudi Arabia, and the United Arab Emirates (UAE), who were identified through the use of multiple databases. The survey, developed in collaboration with a consultant dermatologist in Lebanon, was conducted between September 2021 and January 2022, and comprised 47 questions, including closed-ended multiple-choice questions, multi-select, and Likert scale measurement responses using a 7-point scale (Electronic Supplementary Material Text [ESM] S1). Questions assessed physician characteristics (e.g., diagnostic methods, referral patterns, and prescribing information), patient profiles (e.g., prevalence and severity of AA), and treatment approaches. A total of 200 dermatologists were surveyed (50 from each geographic region). Data collection was carried out through non-response emails to dermatologists, and results were provided as percentage ranges. Programming functionality was checked to ensure that routing, ranges, summations, and question functionality were as indicated in the questionnaire, while quality checks were performed on each individual respondent’s data. This allowed for exclusion of flat-liners (respondents providing the same rating scores to all or the majority of statements), length of interview outliers (extraordinary high/low values), inconsistent answers, poor/invalid open-ended answers, random/pattern answers, and duplicates.
This article reports data from the survey of dermatologists. The study did not involve intervention in human participants or animals and was conducted in accordance with the Declaration of Helsinki and its later amendments. This study was considered to be exempt from institutional review board approval according to national legislations.
Results
Participants
A total of 200 dermatologists were surveyed from four countries across the Middle East: Egypt (n = 50), Lebanon (n = 50), Saudi Arabia (n = 50), and UAE (n = 50). Most participating dermatologists had been practicing for > 10 years (68%) and worked predominantly in small independent private clinics (33%) or academic hospitals (32%). Over one-third of dermatologists surveyed (35%) indicated that, in any given month, they managed > 200 medical dermatology patients for whom they would be the primary treatment decision-maker.
The dermatologists surveyed treated a variety of dermatological conditions. Across the four countries, the dermatologists surveyed indicated that AA was the area of greatest specialist interest (88%), followed by AD (85%), psoriasis (83%), and vitiligo (74%).
Prevalence and Patient Characteristics
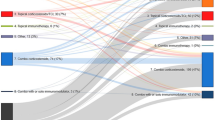
Estimates of AA prevalence in the general population were varied, without a consensus among the surveyed dermatologists. Overall, responses were evenly distributed between the four prevalence categories of 1–3%, 4–6%, 7–10%, and > 10%. Over one-third of dermatologists in Egypt estimated the prevalence of AA to be > 10% in the general population, while 42% of dermatologists surveyed in Saudi Arabia estimated a prevalence of 7–10% (Fig. 1a). The participating dermatologists predominately treated adult patients with AA (58%), although adolescent (24%) and pediatric (18%) patients were also managed (Fig. 1b). Overall, 61% of patients across all age groups were male, and the sex distribution was similar across all four countries (Fig. 1c).
Dermatologists’ perception of prevalence, patient characteristics, and disease severity of patients with AA. a Dermatologists’ perspective of AA prevalence across countries, b patient age distribution, c patient gender distribution, d AA severity by age group. AA alopecia areata, AD atopic dermatitis, UAE United Arab Emirates
Criteria of the Alopecia Areata Scale, an assessment tool designed to evaluate the severity of AA in clinical practice, were used to classify the severity of AA into three groups at the following thresholds: mild AA: ≤ 20% scalp hair loss; moderate AA: 21–49% scalp hair loss; and severe AA: 50–100% scalp hair loss. Across all age groups, most patients treated had mild forms (mild severity) of AA: 63%, 60%, and 54% of pediatric, adolescent, and adult patients, respectively (Fig. 1d). Almost 95% of dermatologists indicated that they treated or managed patients with moderate to severe AA instead of referring them to a different physician (7%) (ESM Fig. S1).
The most frequently affected area was the scalp, with 65% of patients diagnosed with AA experiencing hair loss at this site. Other affected sites included beard (28%), eyebrows (12%), eyelashes (9%), and extremities (8%) (Fig. 2a). Most patients received a diagnosis of patchy AA (55%), with other diagnoses including diffuse AA (14%), AT (10%), ophiasis alopecia (9%), and AU (7%) (Fig. 2b). The proportion of patients with AT or AU was similar across all four countries.
The dermatologists surveyed reported psychological factors to be the greatest contributing risk factor to AA (81%), closely followed by genetic risk factors (75%), environmental factors (52%), and innate and adaptive immunity (50%) (Fig. 3a). Most dermatologists (83%) indicated that comorbidities were common in patients with AA; the most frequently reported comorbidities in patients with mild to moderate AA included thyroid disease (65%), AD (54%), vitiligo (49%), and mental health problems, including anxiety and depression (38%) (Fig. 3b). Over one-half of all patients with AA seen by the surveyed dermatologists (55%) reported bullying behavior from within their community (ESM Fig. S2A). Across all countries, most patients (> 80%) were receiving treatment for psychological disorders (ESM Fig. S2C), and more than two-thirds of the dermatologists surveyed (71%) reported referring patients for further psychological support (ESM Fig. S2B).
Diagnosis
For the diagnosis of AA, nearly one-half of all dermatologists (47%) performed in-house dermoscopies versus referring the patient to other clinics for the procedure. However, over one-quarter of dermatologists in Saudi Arabia (28%) reported neither performing dermoscopies nor referring patients for dermoscopies (ESM Fig. S3A). Overall, 60% of dermatologists performed scalp biopsies at their primary work center when required for diagnosis. However, this was much less common in Egypt, where only 30% of those surveyed reported performing this procedure (ESM Fig. S3B).
The provision of laboratory facilities in dermatologists’ primary work center varied between countries. Most dermatologists in Saudi Arabia (90%) reported access to laboratories at their primary center of work compared with only 24% in Lebanon and 54% in Egypt (ESM Fig. S3C). Only two-fifths of dermatologists (39%) reported conducting therapeutic drug monitoring for biological treatments in their primary work center (ESM Fig. S3D).
The surveyed dermatologists reported using either physical examination alone (43%) or in combination with trichoscopy (46%) to ensure an accurate diagnosis of AA (ESM Fig. S4B). The hair pull test was the most common additional workup procedure used in the diagnosis of AA (62%); others included complete blood count (CBC) tests (61%), hormonal tests (45%), scalp biopsies (31%), and the venereal disease research laboratory test (16%) (ESM Fig. S4A). Differential diagnosis included the exclusion of other similar conditions, including trichotillomania (76%), tinea capitis (71%), telogen and anagen effluvium (47%), and loose anagen hair (29%) (ESM Fig. S4C).
Current Treatments
Overall, most dermatologists (68%) reported following treatment guidelines when managing patients with AA. This was less frequent in the UAE, where over a one-third of those surveyed (38%) reported that there is limited evidence and guidance available for AA management (ESM Fig. S5A). Less than one-third of dermatologists reported personally prescribing advanced treatments to their patients with AA (32%), with the remaining dermatologists referring patients to other physicians (37%) or neither prescribing advanced treatments nor referring them for these treatments (32%) (ESM Fig. S5B). Referrals were substantially higher in Egypt and Saudi Arabia (62% and 56%, respectively) than in the UAE and Lebanon (18% and 10%, respectively), where most dermatologists prescribed advanced treatments (ESM Fig. S5B).
For the management of mild to moderate AA, dermatologists reported using potent topical corticosteroids (92%), topical minoxidil (73%), intralesional corticosteroids (72%), oral corticosteroids (48%), and topical calcineurin inhibitors (48%). Treatments were similar irrespective of severity; moderate to severe AA was also treated with topical corticosteroids (78%), topical minoxidil (70%), oral corticosteroids (67%), intralesional corticosteroids (65%), and topical calcineurin inhibitors (35%). Off-label use of JAK inhibitors was low in patients with mild to moderate AA (9%), and slightly higher in patients with moderate to severe AA (15%) (Table 1).
Overall, potent topical corticosteroids were the preferred first-line treatment for AA, regardless of disease severity (Table 1). The most frequently used proactive treatment option for mild to moderate AA was topical minoxidil (41%), while topical calcineurin inhibitors were the least commonly used (1%) (ESM Fig. S6). Other proactive treatment options used were platelet-rich plasma injections (26%) and topical corticosteroids (24%). Of the dermatologists surveyed, 23% stated they do not use any proactive treatments. When questioned on the hesitance of patients to use steroid treatments, > 90% of dermatologists reported steroid phobia from patients and/or caregivers (ESM Fig. S7A). However, 72% of dermatologists indicated that they would share information regarding treatment options with their patients (ESM Fig. S7B).
Across the region, there was a lack of awareness of investigational drugs for the treatment of AA, with only one-third of dermatologists surveyed (33%) aware of investigative treatment options (Fig. 4a). Overall, 58% and 24% of dermatologists indicated prior knowledge and awareness of ritlecitinib or brepocitinib, respectively (Fig. 4b). Dermatologists from the UAE were found to be the most likely dermmatologists to use systemic JAK inhibitors once approved for the treatment of AA, while dermatologists in Egypt indicated that they were least likely to prescribe JAK inhibitors (Fig. 4c).
Awareness of new and investigative treatments for AA. a, b Percentages of dermatologists aware of investigative treatments for AA (a) and of JAK inhibitors for the treatment of AA (b). c The likelihood of the dermatologists surveyed to prescribe JAK inhibitors (on a scale of 1 [least likely] to 7 [extremely likely]; (average likelihood to prescribe JAK inhibitors is shown at end of bars). AA alopecia areata, JAK Janus kinase, UAE United Arab Emirates.
Assessment of the severity of hair shedding was the most common (47%) method used by the dermatologists surveyed, followed by repeated photography (36%), QOL scores (10%), and Severity of Alopecia Tool (SALT) score (5%). Approximately one-third of dermatologists (33%) reported using all of the measures listed (ESM Fig. S8A), and the majority reported that it was more difficult to determine treatment response than disease severity (ESM Fig. S8B, C).
The dermatologists indicated that the greatest unmet needs in the treatment of moderate to severe AA were long-term disease control (62%), improved efficacy profiles (53%), faster onset of action (52%), and better safety profiles (51%); systemic monotherapies, novel mechanisms of action, and favorable dosing schedules had the lowest priority. Similar unmet needs were identified for the treatment of mild to moderate AA: faster onset (51%), long-term control (44%), and improved efficacy profiles (42%) were highlighted as the areas of greatest unmet need (Fig. 5a, b). Prior to prescribing any new treatments to their patients with AA, dermatologists indicated the main factors they would evaluate were improvements in patient QOL, a tolerable safety profile, and both short- and long-term efficacy (Table 2).
Across the region, only 34% and 18% of dermatologists were aware that patient education initiatives and active support groups, respectively, were available to patients within their institution (ESM Fig. S9A, B). However, dermatologists expressed high levels of interest in informing their patients of these resources going forward (ESM Fig S9C).
Overall, the proportions of prescriptions that were reimbursed were similar across all four countries. Although 26% and 23% of dermatologists reported that their patients were not reimbursed for systemic therapies and topical therapies, respectively, approximately one-third of dermatologists (20%–30%) reported that all prescriptions for systemic or topical therapies received reimbursement (ESM Fig. S10A, B).
Discussion
In this study, 200 dermatologists from across the Middle East were surveyed to assess their perception of the overall prevalence of AA, identify patient characteristics, and evaluate management strategies employed in the region, with the overall aim of identifying any unmet needs in AA. Prevalence estimates varied across the dermatologists surveyed, with no clear consensus. Over one-third of dermatologists in Egypt estimated the prevalence of AA to exceed 10%, while nearly one-half of the dermatologists surveyed in Saudi Arabia reported a slightly lower prevalence of 7–10%. The scarcity of published data on the prevalence of AA in the Middle East makes it challenging to assess the accuracy of these estimates. However, prevalence estimates from the dermatologists surveyed in this study are notably higher than either global prevalence estimates (2%) [6] or estimates from a retrospective, cross-sectional study conducted at the King Abdulaziz Medical City in Riyadh, Saudi Arabia (2.3%) [28]. Studies from the USA have previously reported that physicians often overestimate the diagnosis or probability of disease in their patients [30], so it is likely that physicians also may overestimate the prevalence in the general population.
The dermatologists surveyed treated a range of patients with AA, most of whom presented with mild to moderate AA, although those with more severe forms of AA, including AT and AU, were also treated. The scalp was the most affected area of patients with AA, and patchy AA was the most common form presented by patients; a small proportion of patients with AA (< 20%) also had AT or AU. These data are consistent with those from published reports from other regions [5, 6].
In this study, comorbidities, including thyroid disease, AD, and vitiligo, were common among patients with AA treated by the dermatologists. It has also previously been reported that patients with AA have presented with several systemic comorbidities, such as metabolic syndrome and hypertension, which may play a role in the pathogenesis of AA [31, 32]. In addition, mental health disorders, including depression and anxiety, were frequently identified in patients, further highlighting that the impact of AA extends beyond that of hair loss. It is well established that patients with AA experience psychological and psychosocial symptoms, such as depression, anxiety, anger, social withdrawal, embarrassment, and low self-esteem due to their hair loss, and that these symptoms can have a substantial negative impact on their quality of life [10, 12, 14, 16, 33]. Low self-esteem and higher levels of dissatisfaction with their appearance can impact personal, social, and work-related activities and engagement [34]. Patients with AA often report functional impairment related to decreased work productivity (presenteeism) and increased absenteeism [12, 35]. This increases the financial burden of AA and further contributes to the overall patient burden [12].
The use of treatment guidelines in clinical practice was inconsistent across the region. Specifically, over one- third of dermatologists in the UAE indicated that guidance for the management of AA was limited. Although treatment guidelines are available in certain countries outside the Middle East [4, 36, 37], limited guidance exists in the region for the treatment and management of AA. While over one-half of dermatologists reported consulting treatment guidelines when treating their patients, due to the survey design and binary response selection, no additional information was provided on which treatment guidelines were frequently used. However, dermatologists indicated that they prescribed topical corticosteroids, topical minoxidil, or intralesional corticosteroids as first-line treatments, consistent with established treatment algorithms outlined in published AA treatment guidelines [4, 36, 37]. Given that prescribed treatments were similar irrespective of AA severity, this highlights the unmet need for effective treatments for more severe forms of AA. Additionally, approximately one-third of dermatologists reported prescribing advanced treatments. Although guidelines and consensus statements support the use of advanced systemic treatments for AA, the present study found a low rate of utilization; across the region, off-label use of JAK inhibitors was low, ranging from 9% to 15%. This may reflect physicians’ reluctance to prescribe such treatments, given that at the time this study was conducted, there were no approved JAK inhibitors for AA and off-label treatments are not reimbursed by third-party payers. Together, these factors may limit patient access to new and advanced treatments for AA.
The results of our study suggest that there is limited knowledge among dermatologists in the Middle East of the JAK1/TYK inhibitor brepocitinib or the JAK3/TEC family kinase inhibitor ritlecitinib. However, dermatologists were not asked about their knowledge or awareness of other JAK inhibitors, including baricitinib, which was in late-stage development for the treatment of AA when this study was conducted. Therefore, these results may not accurately reflect physician knowledge of JAK inhibitors for treating AA. Given the recent FDA and EMA approval of baricitinib for the treatment of adults with severe AA [25, 26] and positive results from the ALLEGRO phase 2b/3 study [20], awareness and clinical use of JAK inhibitors is likely to increase throughout the region. However, the results of the present study highlight the need for additional physician education on novel and investigative treatment strategies for AA, including JAK inhibitors, to inform their use in clinical practice.
Patients with AA frequently report high levels of dissatisfaction with commonly used treatment options due to ineffectiveness and adverse effects [12, 16, 38]. Therefore, a substantial unmet need exists for safe and effective treatments for patients with AA. In this study, long-term disease control, improved efficacy and safety profiles, and faster onset of action were identified as the greatest unmet needs in the treatment of AA. The ongoing development of JAK inhibitors, including baricitinib and ritlecitinib, may address the unmet need for new treatments in AA. Both baricitinib and ritlecitinib have demonstrated efficacy up to 36 and 48 weeks, respectively, and both have a tolerable safety profile [20, 24]. The ongoing ALLEGRO-LT study (ClinicalTrials.gov identifier: NCT04006457) will further investigate the long-term efficacy and safety of ritlecitinib in adult and adolescent patients with AA and ≥ 25% hair loss [39].
Although mental health disorders were identified as one of the most common comorbidities in patients with AA, the provision of psychological support appeared to be limited across the region. Most dermatologists were unaware if patient education initiatives or active support groups were available within their institution. Together, these results suggest there is an unmet need for the management of the psychosocial implications in patients with AA and that the provision of psychological support, group support, and education initiatives is warranted.
This study had a number of limitations, including its subjective nature and possible selection bias, both typical for surveys of physicians. Although a moderate response rate was obtained, the data are based on the individual responses of dermatologists and may incorporate some elements of bias. The survey results presented here are also regionally limited due to the inclusion of dermatologists from only four Middle Eastern countries. Additionally, the sample size of dermatologists surveyed was relatively small, which may not give an accurate representation of the overall perceived AA treatment and management landscape within the region; as with any local study, this may impact the generalizability of these results because physicians’ views, knowledge, and clinical practices may differ according to their educational background and training. Finally, the survey design which included closed-ended, multiple-choice questions, multi-select, and Likert scale measurement responses may limit the interpretation of these results as no additional context was provided for specific responses.
Conclusion
In conclusion, this cross-sectional study surveyed dermatologists across the Middle East to provide insights into the overall perceived prevalence, treatment, and management of AA in this region. Although dermatologists followed established treatment guidance for prescribing topical or intralesional corticosteroids or topical minoxidil, there was limited knowledge of investigative treatments for AA, specifically JAK inhibitors, despite these showing promise in clinical development. Long-term disease control and improved efficacy and safety profiles were identified as key areas of unmet need in the treatment of AA. As the treatment landscape for AA continues to evolve, further education regarding novel treatments is warranted to inform clinical decision-making and ensure optimal treatment for patients with AA across the Middle East.
References
Islam N, Leung PS, Huntley AC, Gershwin ME. The autoimmune basis of alopecia areata: a comprehensive review. Autoimmun Rev. 2015;14(2):81–9. https://doi.org/10.1016/j.autrev.2014.10.014.
Safavi KH, Muller SA, Suman VJ, Moshell AN, Melton LJ. Incidence of alopecia Areata in Olmsted county, Minnesota, 1975 through 1989. Mayo Clin Proc. 1995;70(7):628–33. https://doi.org/10.4065/70.7.628.
Tosti A, Bellavista S, Iorizzo M. Alopecia areata: a long term follow-up study of 191 patients. J Am Acad Dermatol. 2006;55(3):438–41. https://doi.org/10.1016/j.jaad.2006.05.008.
Cranwell WC, Lai VW, Photiou L, et al. Treatment of alopecia areata: an Australian expert consensus statement. Australas J Dermatol. 2019;60(2):163–70. https://doi.org/10.1111/ajd.12941.
Pratt CH, King LE Jr, Messenger AG, Christiano AM, Sundberg JP. Alopecia areata. Nat Rev Dis Primers. 2017;3:17011. https://doi.org/10.1038/nrdp.2017.11.
Lee HH, Gwillim E, Patel KR, et al. Epidemiology of alopecia areata, ophiasis, totalis, and universalis: a systematic review and meta-analysis. J Am Acad Dermatol. 2020;82(3):675–82. https://doi.org/10.1016/j.jaad.2019.08.032.
Gilhar A, Etzioni A, Paus R. Alopecia areata. N Engl J Med. 2012;366(16):1515–25. https://doi.org/10.1056/NEJMra1103442.
Goh C, Finkel M, Christos PJ, Sinha AA. Profile of 513 patients with alopecia areata: associations of disease subtypes with atopy, autoimmune disease and positive family history. J Eur Acad Dermatol Venereol. 2006;20(9):1055–60. https://doi.org/10.1111/j.1468-3083.2006.01676.x.
Aldhouse NVJ, Kitchen H, Knight S, et al. “You lose your hair, what’s the big deal?’ I was so embarrassed, I was so self-conscious, I was so depressed:” a qualitative interview study to understand the psychosocial burden of alopecia areata. J Patient Rep Outcomes. 2020;4(1):76. https://doi.org/10.1186/s41687-020-00240-7.
Liu LY, King BA, Craiglow BG. Alopecia areata is associated with impaired health-related quality of life: A survey of affected adults and children and their families. J Am Acad Dermatol. 2018;79(3):556-558.e1. https://doi.org/10.1016/j.jaad.2018.01.048.
Marahatta S, Agrawal S, Adhikari BR. Psychological impact of alopecia areata. Dermatol Res Pract. 2020;2020:8879343. https://doi.org/10.1155/2020/8879343.
Mesinkovska N, King B, Mirmirani P, Ko J, Cassella J. Burden of illness in alopecia areata: a cross-sectional online survey study. J Investig Dermatol Symp Proc. 2020;20(1):S62-s68. https://doi.org/10.1016/j.jisp.2020.05.007.
Mostaghimi A, Napatalung L, Sikirica V, et al. Patient perspectives of the social, emotional and functional impact of alopecia areata: a systematic literature review. Dermatol Ther (Heidelb). 2021;11(3):867–83. https://doi.org/10.1007/s13555-021-00512-0.
Okhovat JP, Marks DH, Manatis-Lornell A, Hagigeorges D, Locascio JJ, Senna MM. Association between alopecia areata, anxiety, and depression: a systematic review and meta-analysis. J Am Acad Dermatol. 2023;88(5):1040-50. https://doi.org/10.1016/j.jaad.2019.05.086.
Toussi A, Barton VR, Le ST, Agbai ON, Kiuru M. Psychosocial and psychiatric comorbidities and health-related quality of life in alopecia areata: a systematic review. J Am Acad Dermatol. 2021;85(1):162–75. https://doi.org/10.1016/j.jaad.2020.06.047.
United States Food and Drug Administration. Patient-focused drug development public meeting for alopecia areata. 2017. https://www.fda.gov/ForIndustry/UserFees/PrescriptionDrugUserFee/ucm554443.htm. Accessed 21 June 2023
Huang KP, Mullangi S, Guo Y, Qureshi AA. Autoimmune, atopic, and mental health comorbid conditions associated with alopecia areata in the United States. JAMA Dermatol. 2013;149(7):789–94. https://doi.org/10.1001/jamadermatol.2013.3049.
Triyangkulsri K, Suchonwanit P. Role of janus kinase inhibitors in the treatment of alopecia areata. Drug Des Devel Ther. 2018;12:2323–35. https://doi.org/10.2147/dddt.s172638.
Gupta AK, Carviel JL, Foley KA, et al. Monotherapy for alopecia areata: a systematic review and network meta-analysis. Skin Appendage Disord. 2019;5(6):331–7. https://doi.org/10.1159/000501940.
King B, Zhang X, Gubelin Harcha W, et al. Efficacy and safety of ritlecitinib in adults and adolescents with alopecia areata: a randomised, double-blind, multicentre phase 2b/3 trial. Lancet. 2023;401(10387):1518–29.
King B, Guttman-Yassky E, Peeva E, et al. A phase 2a randomized, placebo-controlled study to evaluate the efficacy and safety of the oral Janus kinase inhibitors ritlecitinib and brepocitinib in alopecia areata: 24-week results. J Am Acad Dermatol. 2021;85(2):379–87. https://doi.org/10.1016/j.jaad.2021.03.050.
Ramírez-Marín HA, Tosti A. Evaluating the therapeutic potential of ritlecitinib for the treatment of alopecia areata. Drug Des Devel Ther. 2022;16:363–74. https://doi.org/10.2147/DDDT.S334727.
Dillon KL. A Comprehensive literature review of JAK inhibitors in treatment of alopecia areata. Clin Cosmet Investig Dermatol. 2021;14:691–714. https://doi.org/10.2147/CCID.S309215.
King B, Ohyama M, Kwon O, et al. Two phase 3 trials of baricitinib for alopecia areata. N Engl J Med. 2022;386(18):1687–99. https://doi.org/10.1056/NEJMoa2110343.
United States Food and Drug Administration. FDA approves first systemic treatment for alopecia areata. 2022. https://www.fda.gov/news-events/press-announcements/fda-approves-first-systemic-treatment-alopecia-areata. Accessed 21 June 2023.
European Medicines Agency. Olumiant (baricitinib). https://www.ema.europa.eu/en/medicines/human/EPAR/olumiant. Accessed 21 June 2023.
Oluminant (baricitinib). Prescribing Information. 2022. https://pi.lilly.com/us/olumiant-uspi.pdf. Accessed 21 June 2023.
Alomaish AR, Gosadi IM, Dallak FH, et al. Prevalence of alopecia and its contributing factors among primary healthcare attendees in the Jazan region, Saudi Arabia. J Family Med Prim Care. 2021;10(10):3851–6. https://doi.org/10.4103/jfmpc.jfmpc_1070_21.
Alshahrani AA, Al-Tuwaijri R, Abuoliat ZA, Alyabsi M, AlJasser MI, Alkhodair R. Prevalence and clinical characteristics of alopecia Areata at a tertiary care center in Saudi Arabia. Dermatol Res Pract. 2020;2020:7194270. https://doi.org/10.1155/2020/7194270.
Morgan DJ, Pineles L, Owczarzak J, et al. Accuracy of practitioner estimates of probability of diagnosis before and after testing. JAMA Intern Med. 2021;181(6):747–55. https://doi.org/10.1001/jamainternmed.2021.0269.
Gopinath H, Upadya GM. Metabolic syndrome in androgenic alopecia. Indian J Dermatol Venereol Leprol. 2016;82(4):404–8. https://doi.org/10.4103/0378-6323.174421.
Stefanadi EC, Dimitrakakis G, Antoniou CK, et al. Metabolic syndrome and the skin: a more than superficial association. Reviewing the association between skin diseases and metabolic syndrome and a clinical decision algorithm for high risk patients. Diabetol Metab Syndr. 2018;10:9. https://doi.org/10.1186/s13098-018-0311-z
Kim AB, Cheng BT, Hassan S. Association of mental health outcomes and lower patient satisfaction among adults with alopecia: a cross-sectional population-based study. JAAD Int. 2022;8:82–8. https://doi.org/10.1016/j.jdin.2022.05.011.
Hunt N, McHale S. The psychological impact of alopecia. BMJ. 2005;331(7522):951–3. https://doi.org/10.1136/bmj.331.7522.951.
Senna M, Ko J, Glashofer M, Edison-Heredia E, Zhu B, Shapiro J. Predictors of QOL in patients with alopecia areata. J Investig Dermatol. 2022;142(10):2646–50. https://doi.org/10.1016/j.jid.2022.02.019.
Meah N, Wall D, York K, et al. The Alopecia Areata Consensus of Experts (ACE) study: results of an international expert opinion on treatments for alopecia areata. J Am Acad Dermatol. 2020;83(1):123–30. https://doi.org/10.1016/j.jaad.2020.03.004.
Rossi A, Muscianese M, Piraccini BM, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154(6):609–23. https://doi.org/10.23736/S0392-0488.19.06458-7.
Hussain ST, Mostaghimi A, Barr PJ, Brown JR, Joyce C, Huang KP. Utilization of mental health resources and complementary and alternative therapies for alopecia areata: A U.S. survey. Int J Trichology. 2017;9(4):160–4. https://doi.org/10.4103/ijt.ijt_53_17.
ClinicalTrials.gov. Long-Term PF-06651600 for the Treatment of Alopecia Areata (ALLEGRO-LT). https://clinicaltrials.gov/ct2/show/NCT04006457. Accessed 21 June 2023.
Acknowledgements
The authors thank the dermatologists who undertook the survey and participated in this study. The authors also thank the team at Sermo (New York, NY, USA) for their support with the creation and distribution of the survey used in this study.
Funding
This study and the journal’s Rapid Service Fee was funded by Pfizer Gulf FZ LLC.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Medical Writing and Editorial Assistance
Third-party medical writing assistance provided by James Glen, MRes, of Health Interactions, Inc, was funded by Pfizer LLC.
Author Contributions
Conceptualization: Marcelle Ghoubar, Alfred Ammoury. Methodology: Marcelle Ghoubar, Alfred Ammoury. Formal analysis and investigation: Marcelle Ghoubar, Nehal Hassan. Writing—original draft preparation: Alfred Ammoury, Rehab Hegazy, Saad Al Talhab, Ahmed Ameen, Nehal Hassan, Marcelle Ghoubar. Writing—review and editing: Alfred Ammoury, Rehab Hegazy, Saad Al Talhab, Ahmed Ameen, Nehal Hassan, Marcelle Ghoubar. Funding acquisition: Marcelle Ghoubar, Nehal Hassan. Resources: Marcelle Ghoubar, Nehal Hassan. Supervision: Marcelle Ghoubar, Nehal Hassan.
Disclosures
Alfred Ammoury has received consultancies and/or honoraria from AbbVie, Biologix, Janssen, Lilly, LEO, Novartis, and Pfizer. Rehab Hegazy has nothing to disclose. Saad Al Talhab has nothing to disclose. Ahmed Ameen has been a speaker, advisor, and/or investigator for AbbVie, Bayer, Biologix, Ego, Ferrer, Galderma, Hikma, Jamjoom, Janssen, LEO Pharma, Lilly, Novartis, Pfizer, and Sanofi. Marcelle Ghoubar and Nehal Hassan are employees of Pfizer Gulf FZ LLC and Pfizer Egypt LLC, respectively.
Compliance with Ethics Guidelines
This article is based on a previously conducted survey and does not contain any new studies or intervention with human participants or animals performed by any of the authors. The study was in accordance with the Declaration of Helsinki and its later amendments and is considered exempt from institutional review board approval according to national legislations.
Data Availability
The datasets generated during and/or analyzed during the current study are published alongside this paper as supplementary material and are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ammoury, A., Hegazy, R., Al Talhab, S. et al. Treatment Patterns and Unmet Needs in the Management of Alopecia Areata: Results of a Physician’s Survey in the Middle East. Dermatol Ther (Heidelb) 13, 1801–1815 (2023). https://doi.org/10.1007/s13555-023-00963-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-00963-7