Abstract
One of the most common neurodegenerative illnesses is Parkinson’s disease (PD). Rotigotine (RTG) is a dopamine agonist that exerts anti-Parkinsonian effects through dopamine receptor agonism to improve motor symptoms and overall performance in PD patients. In this study, an in situ liquid crystal gel called rotigotine-gel (RTG-gel) was developed using soya phosphatidyl choline (SPC) and glycerol dioleate (GDO) to provide long-acting slow-release benefits of rotigotine while minimizing side effects. This study prepared the RTG-gel precursor solution using SPC, GDO, and ethanol (in the ratio of 54:36:10, w/w/w). The internal structures of the gel were confirmed by crossed-polarized light microscopy (PLM), small-angle X-ray scattering (SAXS), and differential scanning calorimetry (DSC). The rheological properties of the RTG-gel precursor solution indicate a favorable combination of low viscosity and excellent flowability. The gel that produced during water absorption was also highly viscous and structurally stable, which helped to maintain the drug delayed release at the injection site. In vitro release assays showed that the in vitro release of RTG-gel followed Ritger-Peppas. The RTG-gel precursor solution was administered by subcutaneous injection, and the results of in vivo pharmacokinetic tests in SD rats showed that the plasma elimination half-life (t1/2) was 59.28 ± 16.08 h; the time to peak blood concentration (Tmax) was 12.00 ± 10.32 h, and the peak concentration (Cmax) was 29.9 ± 10.10 ng/mL. The blood concentration remained above 0.1 ng/mL for 20 days after administration and was still detectable after 31 days of administration, and the bioavailability of RTG can reach 72.59%. The results of in vitro solvent exchange tests showed that the RTG-gel precursor solution undergoes rapid exchange upon contact with PBS, and the diffusion of ethanol can reach 48.1% within 60 min and 80% within 8 h. The results of cytotoxicity test showed 89.27 ± 4.32% cell survival after administration of the drug using RTG-gel. The results of tissue extraction at the administration site showed that healing of the injection site without redness and hemorrhage could be observed after 14 days of injection. The results of tissue section of the administered site showed that the inflammatory cells decreased and granulation tissue appeared after 14 days of administration, and there was basically no inflammatory cell infiltration after 35 days of administration, and the inflammatory reaction was basically eliminated. It shows that RTG-gel has some irritation to the injection site, but it can be recovered by itself in the later stage, and it has good biocompatibility. In summary, RTG-gel might be a potential RTG extended-release formulation for treating PD.
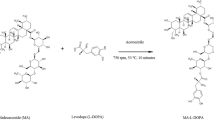
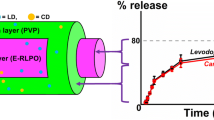
Graphical Abstract














Similar content being viewed by others
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Materials availability
N/A
References
Ko T, Brenner AM, Monteiro NP, Debastiani MS, et al. Abnormal eye movements in parkinsonism: a historical view. Arq Neuropsiquiatr. 2021;79(5):457–9.
Costa HN, Esteves AR, Empadinhas N, Cardoso SM. Parkinson’s disease: a multisystem disorder. Neurosci Bull. 2023;39(1):113–24. https://doi.org/10.1007/s12264-022-00934-6.
Johnson M, Stecher B, Labrie V, Brundin L, et al. Triggers, facilitators, and aggravators: redefining Parkinson’s disease pathogenesis. 2019;42:4–13.
Choi JH, Kim JM, Yang HK, Lee HJ, et al. Clinical perspectives of Parkinson’s disease for ophthalmologists, otorhinolaryngologists, cardiologists, dentists, gastroenterologists, urologists, physiatrists, and psychiatrists. J Korean Med Sci. 2020;35(28): e230. https://doi.org/10.3346/jkms.2020.35.e230.
Bang Y, Lim J, Choi HJ. Recent advances in the pathology of prodromal non-motor symptoms olfactory deficit and depression in Parkinson’s disease: clues to early diagnosis and effective treatment. Arch Pharm Res. 2021;44(6):588–604. https://doi.org/10.1007/s12272-021-01337-3.
Bloem BR, Okun MS, Klein C. Parkinson’s disease. Lancet. 2021;397(10291):2284–303. https://doi.org/10.1016/s0140-6736(21)00218-x.
Church FC. Treatment options for motor and non-motor symptoms of Parkinson’s disease. Biomolecules. 2021;11(4). https://doi.org/10.3390/biom11040612.
Prasad EM, Hung SY. Current therapies in clinical trials of Parkinson’s disease: a 2021 update. Pharmaceuticals (Basel). 2021;14(8). https://doi.org/10.3390/ph14080717.
Kalinderi K, Papaliagkas V, Fidani L. Pharmacogenetics and levodopa induced motor complications. Int J Neurosci. 2019;129(4):384–92. https://doi.org/10.1080/00207454.2018.1538993.
Chagraoui A, Boulain M, Juvin L, Anouar Y, et al. L-DOPA in Parkinson’s disease: looking at the “false” neurotransmitters and their meaning. Int J Mol Sci. 2019;21(1). https://doi.org/10.3390/ijms21010294.
Fu J, Zhao X, Tian F, Yu X. Continuous dopaminergic stimulation counteracts L-DOPA-induced overactivity of Ca(2+) in 6-OHDA-lesioned rats. Exp Brain Res. 2022;240(7–8):1933–41. https://doi.org/10.1007/s00221-022-06390-y.
Olanow CW, Calabresi P, Obeso JA. Continuous dopaminergic stimulation as a treatment for Parkinson’s disease: current status and future opportunities. Mov Disord. 2020;35(10):1731–44. https://doi.org/10.1002/mds.28215.
Lv H, Yu F, Sha C, Huang Y, et al. Effects of rotigotine and rotigotine extended-release microsphere therapy on myocardial ischemic injury in mice. Eur J Pharm Sci. 2019;134:1–6. https://doi.org/10.1016/j.ejps.2019.04.009.
Raeder V, Boura I, Leta V, Jenner P, et al. Rotigotine Transdermal patch for motor and non-motor Parkinson’s disease: a review of 12 years’ clinical experience. CNS Drugs. 2021;35(2):215–31. https://doi.org/10.1007/s40263-020-00788-4.
Swart PJ, de Zeeuw RA. Pharmacokinetics of the dopamine D2 agonist S(-)-2-(N-propyl-N-2-thienylethylamino)-5-hydroxytetralin in freely moving rats. J Pharm Sci. 1993;82(2):200–3. https://doi.org/10.1002/jps.2600820217.
Fox SH, Katzenschlager R, Lim SY, Barton B, et al. International Parkinson and movement disorder society evidence-based medicine review: update on treatments for the motor symptoms of Parkinson’s disease. Mov Disord. 2018;33(8):1248–66. https://doi.org/10.1002/mds.27372.
Frampton JE. Rotigotine transdermal patch: a review in Parkinson’s disease. CNS Drugs. 2019;33(7):707–18. https://doi.org/10.1007/s40263-019-00646-y.
Elshoff JP, Cawello W, Andreas JO, Mathy FX, et al. An update on pharmacological, pharmacokinetic properties and drug-drug interactions of rotigotine transdermal system in Parkinson’s disease and restless legs syndrome. Drugs. 2015;75(5):487–501. https://doi.org/10.1007/s40265-015-0377-y.
Elshoff JP, Braun M, Andreas JO, Middle M, et al. Steady-state plasma concentration profile of transdermal rotigotine: an integrated analysis of three, open-label, randomized, phase I multiple dose studies. Clin Ther. 2012;34(4):966–78. https://doi.org/10.1016/j.clinthera.2012.02.008.
Kolawole OM, Cook MT. In situ gelling drug delivery systems for topical drug delivery. Eur J Pharm Biopharm. 2023;184:36–49. https://doi.org/10.1016/j.ejpb.2023.01.007.
Supper S, Anton N, Seidel N, Riemenschnitter M, et al. Thermosensitive chitosan/glycerophosphate-based hydrogel and its derivatives in pharmaceutical and biomedical applications. Expert Opin Drug Delivery. 2014;11(2):249–67. https://doi.org/10.1517/17425247.2014.867326.
Kolawole OM, Lau WM, Khutoryanskiy VV. Chitosan/β-glycerophosphate in situ gelling mucoadhesive systems for intravesical delivery of mitomycin-C Int J Pharm X. 2019;1:100007. https://doi.org/10.1016/j.ijpx.2019.100007.
Okur NU, Yagcilar AP, Siafaka PI. Promising polymeric drug carriers for local delivery: the case of in situ gels. Curr Drug Delivery. 2020;17(8):675–93. https://doi.org/10.2174/1567201817666200608145748.
Silvestrini AVP, Caron AL, Viegas J, Praça FG, et al. Advances in lyotropic liquid crystal systems for skin drug delivery. Expert Opin Drug Deliv. 2020;17(12):1781–805. https://doi.org/10.1080/17425247.2020.1819979.
Zhai J, Fong C, Tran N, Drummond CJ. Non-lamellar lyotropic liquid crystalline Lipid nanoparticles for the next generation of nanomedicine. ACS Nano. 2019;13(6):6178–206. https://doi.org/10.1021/acsnano.8b07961.
Guo C, Wang J, Cao F, Lee RJ, et al. Lyotropic liquid crystal systems in drug delivery. Drug Discovery Today. 2010;15(23):1032–40. https://doi.org/10.1016/j.drudis.2010.09.006.
Chavda VP, Dawre S, Pandya A, Vora LK, et al. Lyotropic liquid crystals for parenteral drug delivery. J Control Release. 2022;349:533–49. https://doi.org/10.1016/j.jconrel.2022.06.062.
Li Y, Angelova A, Liu J, Garamus VM, et al. In situ phase transition of microemulsions for parenteral injection yielding lyotropic liquid crystalline carriers of the antitumor drug bufalin. Colloids Surf B Biointerfaces. 2019;173:217–25. https://doi.org/10.1016/j.colsurfb.2018.09.023.
Xia M-Q, Liu L, Tian C-L, Li Q, et al. Pharmacokinetics of sinomenine hydrochloride cubic liquid crystal injection based on microdialysis technology. J Drug Delivery Sci Technol. 2019;52:553–558. https://doi-org-s.ytu.yitlink.com:443/10.1016/j.jddst.2019.05.021.
Salata GC, Malagó ID, Lopes LB. A lipid-based in situ-forming hexagonal phase for prolonged retention and drug release in the breast tissue. AAPS PharmSciTech. 2022;23(7):260. https://doi.org/10.1208/s12249-022-02411-9.
Fang X, Shen A. Preparation and evaluation of phytantriol liquid crystal as a liquid embolic agent. Pharm Dev Technol. 2020;25(5):610–6. https://doi.org/10.1080/10837450.2020.1725046.
Le NTT, Cao VD, Nguyen TNQ, Le TTH, et al. Soy lecithin-derived liposomal delivery systems: surface modification and current applications. Int J Mol Sci. 2019;20(19). https://doi.org/10.3390/ijms20194706.
Sriwidodo A, Umar K, Wathoni N, Zothantluanga JH, et al. Liposome-polymer complex for drug delivery system and vaccine stabilization. Heliyon. 2022;8(2):e08934. https://doi.org/10.1016/j.heliyon.2022.e08934.
Zhang P, Chen D, Tian Y, Li H, et al. Comparison of three in-situ gels composed of different oil types. Int J Pharm. 2020;587: 119707. https://doi.org/10.1016/j.ijpharm.2020.119707.
Wadsäter M, Barauskas J, Tiberg F, Nylander T. The lipolytic degradation of highly structured cubic micellar nanoparticles of soy phosphatidylcholine and glycerol dioleate by phospholipase A(2) and triacylglycerol lipase. Chem Phys Lipids. 2018;211:86–92. https://doi.org/10.1016/j.chemphyslip.2017.11.011.
Wang X, Huang L, Zhang Y, Meng F, et al. Tunable two-compartment on-demand sustained drug release based on lipid gels. J Pharm Sci. 2020;109(2):1059–67. https://doi.org/10.1016/j.xphs.2019.10.021.
Rosenbaum E, Tavelin S, Johansson LBÅ. A characterisation study on the application of inverted lyotropic phases for subcutaneous drug release. Int J Pharm. 2010;388(1):52–57. https://doi-org-s.ytu.yitlink.com:443/10.1016/j.ijpharm.2009.12.032.
Zeng N, Hu Q, Liu Z, Gao X, et al. Preparation and characterization of paclitaxel-loaded DSPE-PEG-liquid crystalline nanoparticles (LCNPs) for improved bioavailability. Int J Pharm. 2012;424(1):58–66. https://doi.org/10.1016/j.ijpharm.2011.12.058.
Wu W, Cao W, Chen J, Cai Y, et al. In situ liquid crystal gel as a promising strategy for improving ocular administration of dexamethasone: preparation, characterization, and evaluation. AAPS PharmSciTech. 2021;23(1):36. https://doi.org/10.1208/s12249-021-02193-6.
Chen Y, Liang X, Ma P, Tao Y, et al. Phytantriol-based in situ liquid crystals with long-term release for intra-articular administration. AAPS PharmSciTech. 2015;16(4):846–54. https://doi.org/10.1208/s12249-014-0277-6.
Yang Z, Liang X, Jiang X, Guo J, et al. Development and evaluation of minocycline hydrochloride-loaded in situ cubic liquid crystal for intra-periodontal pocket administration. Molecules. 2018;23(9). https://doi.org/10.3390/molecules23092275.
Vyazovkin S, Burnham AK, Criado JM, Pérez-Maqueda LA, et al. ICTAC Kinetics Committee recommendations for performing kinetic computations on thermal analysis data. Thermochim Acta. 2011;520(1):1–19. https://doi.org/10.1016/j.tca.2011.03.034.
Srichan T, Phaechamud T. Designing solvent exchange-induced in situ forming gel from aqueous insoluble polymers as matrix base for periodontitis treatment. AAPS PharmSciTech. 2017;18(1):194–201. https://doi.org/10.1208/s12249-016-0507-1.
Wang A, Liang R, Liu W, Sha C, et al. Effect of palmitic acid on the characteristics and release profiles of rotigotine-loaded microspheres. Pharm Dev Technol. 2016;21(1):3–7. https://doi.org/10.3109/10837450.2015.1011662.
Zhang P, Chen D, Tian Y, Li H, et al. Comparison of three in-situ gels composed of different oil types. Int J Pharm (Amsterdam, Neth.). 2020;587:119707. https://doi.org/10.1016/j.ijpharm.2020.119707.
Kamali H, Khodaverdi E, Hadizadeh F, Mohajeri SA. In-vitro, ex-vivo, and in-vivo evaluation of buprenorphine HCl release from an in situ forming gel of PLGA-PEG-PLGA using N-methyl-2-pyrrolidone as solvent. Mater Sci Eng C. 2019;96:561–575. https://doi.org/10.1016/j.msec.2018.11.058.
Chen J, Long W, Dong B, Cao W, et al. Hexagonal liquid crystalline system containing cinnamaldehyde for enhancement of skin permeation of sinomenine hydrochloride. Pharm Dev Technol. 2022;27(6):684–94. https://doi.org/10.1080/10837450.2022.2107011.
Calixto GMF, Victorelli FD, Franz-Montan M, Baltazar F, et al. Innovative mucoadhesive precursor of liquid crystalline system loading anti-gellatinolytic peptide for topical treatment of oral cancer. J Biomed Nanotechnol. 2021;17(2):253–62. https://doi.org/10.1166/jbn.2021.3025.
Xingqi W, Yong Z, Xing L, Yang W, et al. Cubic and hexagonal liquid crystal gels for ocular delivery with enhanced effect of pilocarpine nitrate on anti-glaucoma treatment. Drug Delivery. 2019;26(1):952–64. https://doi.org/10.1080/10717544.2019.1667451.
Zhang P, Chen D, Tian Y, Li H, et al. Comparison of three in-situ gels composed of different oil types. Int J Pharm. 2020;587(1): 119707. https://doi.org/10.1016/j.ijpharm.2020.119707.
Ribeiro IR, Immich MF, Lundberg D, Poletto F, et al. Physiological neutral pH drives a gradual lamellar-to-reverse cubic-to-reverse hexagonal phase transition in phytantriol-based nanoparticles. Biointerfaces. 2019;177(1):204–10. https://doi.org/10.1016/j.colsurfb.2019.01.055.
Soliman KA, Ullah K, Shah A, Jones DS, et al. Poloxamer-based in situ gelling thermoresponsive systems for ocular drug delivery applications. Drug Discov Today. 2019;24(8):1575–86. https://doi.org/10.1016/j.drudis.2019.05.036.
Zad Bagher Seighalani F, Joyner H, Ross C. Relationships among rheological, sensory, and wear behaviors of cheeses. J Texture Stud. 2020;51(5):702–721. https://doi.org/10.1111/jtxs.12547.
Jie H, Liu L, Shuangying G, Xingqi W, et al. A novel phytantriol-based in situ liquid crystal gel for vaginal delivery. AAPS PharmSciTech. 2019;20(5):185. https://doi.org/10.1208/s12249-019-1393-0.
Wang H, Peng T, Wu H, Chen J, et al. In situ biomimetic lyotropic liquid crystal gel for full-thickness cartilage defect regeneration. J Control Release. 2021;338:623–32. https://doi.org/10.1016/j.jconrel.2021.08.062.
Mei L, Xie Y, Huang Y, Wang B, et al. Injectable in situ forming gel based on lyotropic liquid crystal for persistent postoperative analgesia. Acta Biomater. 2018;67:99–110. https://doi.org/10.1016/j.actbio.2017.11.057.
Kamali H, Khodaverdi E, Hadizadeh F, Mohajeri SA. In-vitro, ex-vivo, and in-vivo evaluation of buprenorphine HCl release from an in situ forming gel of PLGA-PEG-PLGA using N-methyl-2-pyrrolidone as solvent. Mater Sci Eng C Mater Biol Appl. 2019;96:561–75. https://doi.org/10.1016/j.msec.2018.11.058.
Rahimi M, Mobedi H, Behnamghader A. In situ forming poly(lactic acid-co-glycolic acid) implants containing leuprolide acetate/β-cyclodextrin complexes: preparation, characterization, and in vitro drug release. Int J Polym Mater Polym Biomater. 2016;65(2):75–84. https://doi.org/10.1080/00914037.2015.1055633.
Kamali H, Khodaverdi E, Mohammadpour F, Kakavand A, et al. The impacts of PLGA/PEG triblock copolymers with variable molecular weights on the sustained release of buprenorphine. Curr Drug Deliv. 2022;19(3):357–68. https://doi.org/10.2174/1567201818666210708115841.
Kim MS, Ho MJ, Joung MY, Choi YS, et al. Effect of dispersion medium on pharmacokinetic profile of rotigotine crystalline suspension following subcutaneous injection. Pharmaceutics. 2022;14(2630). https://doi.org/10.3390/pharmaceutics14122630.
Acknowledgements
Thanks to Yantai Institute of Materia Medica for providing experimental equipment and space.
Funding
The authors would like to thank the Yantai Institute of Materia Medica and the Shandong Laboratory of Yantai Drug Discovery for funding this work.
Author information
Authors and Affiliations
Contributions
Xiaxia Wu: conceptualization, writing—original draft, writing—review and editing. Dongfang Cheng: conceptualization, writing—review and editing, supervision. Yue Lu: writing—original draft, writing—review and editing. Rong Rong: writing—review and editing. Ying Kong: writing—review and editing. Xiuzhi Wang: writing—review and editing. Baohua Niu: writing—review and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the animal experiments reported in this paper were approved by the Committee on the Ethics of Animal Experiments of the Yantai Institute of Materia Medica and were performed in strict accordance with the guidelines of the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Consent for publication
All the authors provided consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, X., Cheng, D., Lu, Y. et al. A liquid crystal in situ gel based on rotigotine for the treatment of Parkinson’s disease. Drug Deliv. and Transl. Res. 14, 1048–1062 (2024). https://doi.org/10.1007/s13346-023-01449-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-023-01449-x