Abstract
Pancreas units represent new organizational models of care that are now at the center of the European debate. The PUECOF study, endorsed by the European–African Hepato-Pancreato-Biliary Association (E-AHPBA), aims to reach an expert consensus by enquiring surgical leaders about the Pancreas Units’ most relevant organizational factors, with 30 surgical leaders from 14 countries participating in the Delphi survey. Results underline that surgeons believe in the need to organize multidisciplinary meetings, nurture team leadership, and create metrics. Clinical professionals and patients are considered the most relevant stakeholders, while the debate is open when considering different subjects like industry leaders and patient associations. Non-technical skills such as ethics, teamwork, professionalism, and leadership are highly considered, with mentoring, clinical cases, and training as the most appreciated facilitating factors. Surgeons show trust in functional leaders, key performance indicators, and the facilitating role played by nurse navigators and case managers. Pancreas units have a high potential to improve patients' outcomes. While the pancreas unit model of care will not change the technical content of pancreatic surgery, it may bring surgeons several benefits, including more cases, professional development, easier coordination, less stress, and opportunities to create fruitful connections with research institutions and industry leaders.
Similar content being viewed by others
Introduction
Pancreatic cancer (PC) has the worst prognosis among solid malignancies and carries the most remarkable mortality rate. Although clinical research and practice have increased the likelihood of prolonged survival in recent years, the diagnostic and therapeutic path remains extremely demanding. When feasible, radical surgery combined with systemic chemotherapy offers the highest chances for long-term survival, with highly specialized centers in pancreatic surgery leading to better clinical outcomes when compared to low-volume ones [1,2,3,4,5]. The majority of patients diagnosed with PC will need palliative and end-of-life care [6,7,8].
Each phase of the clinical pathway, from first diagnosis to therapeutic decisions and follow-up, requires specialized knowledge and skills. Among these, surgery represents a crucial step, together with histopathology, medical oncology, radiotherapy, and palliative care. Nonetheless, each patient must be treated for their unique nutritional [9, 10] and psychological [11, 12] needs. Integrating simultaneous and palliative treatment, from the earliest phases to end-of-life care, requires a multidisciplinary approach to a care continuum.
As translational research is often slow, improvement can be found in organizational innovation, namely, designing a different, most efficient, and effective patient’s journey. The so-called disease units represent new organizational, patient-centric models of care, where various medical professionals and stakeholders share their contributions and knowledge, and actions are tailored according to the disease and the single patient’s needs [13]. In general terms, a disease unit differs from a simple multidisciplinary board in several aspects, including:
-
A more comprehensive number and variety of stakeholders involved in the process beyond medical professionals.
-
The presence of professional figures aiming at bridging the knowledge and organizational gaps between the patient and the medical staff, fostering, whenever possible, co-production and shared decision-making dynamics [14,15,16,17].
-
The creation, collection, and sharing of medical information about the patient, but also in an aggregate way for clinical and research purposes.
-
The definition and monitoring of each step of care by balancing those medical activities that may be more complex or require higher specialization or instruments than those that may be easily present in less specialized centers.
The European debate on disease units is now lively when it comes to PC. Pancreas units, depending on national or regional regulation, are requested to have specified characteristics and minimal requirements, leaving to hub centers defined activities (i.e., surgery) and to spokes some others (i.e., endoscopy, medical treatment, biopsies). Still, there is an open debate and lack of literature on how these pancreas units should be designed, which organizational model they should follow, and how knowledge should be created, captured, and shared in a multistakeholders’ approach.
Starting from these premises, the PUECOF (Pancreas Unit Expert Consensus on the Organizational Factors) study aims to test a possible organizational model through a Delphi panel, seeking an expert consensus among surgical leaders involved in the European pancreatic surgery scenario. In their role as hybrid managers with some managerial responsibilities [18, 19], surgical leaders represent key figures in setting up the “rules of the games” in establishing such new organizational structures. The study was endorsed by the European–African Hepato-Pancreato-Biliary Association (E-AHPBA).
Methods
Design and setting
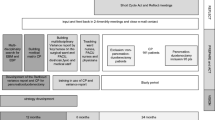
A Delphi survey [20, 21] was designed starting from the recent literature on healthcare organization science [13], stakeholders’ engagement [14], knowledge translation [22], and non-technical skills [23,24,25]. The survey was conceived by a multidisciplinary panel encompassing scholars in general surgery, healthcare management, organization science, social statistics, and healthcare policies. The final version of the survey was revised by the steering committee (LC, FDM, GM, GBu, and IF) and audited by E-AHPBA to grant the endorsement, which was given in October 2022.
The experts included in the panel were gathered from the members’ list of E-AHPBA. The criteria for selecting the participants were: renowned leadership in pancreatic surgery practice and research within the E-AHPBA community, affiliation to high-volume centers, and diversity in gender and countries to cover most of the E-AHPBA area of interest.
Thirty-eight surgical leaders from 17 countries were personally invited via email to join the initiative. The project was advertised on the E-AHPBA website, although participation was by invitation only. Thirty experts accepted the invitation and participated in the first round. Twenty-six experts participated in the second round, with a response rate of 87%. Data collection was carried out between November 2022 and March 2023 through Google Forms.
Survey and statistical analysis
The Delphi survey included some descriptive statistics and four sections, namely the organizational factors (14 items), the stakeholders (18 items), the non-technical skills (1 + 16 items), and the processes and knowledge translation facilitators (31 items). All items needed to be voted on by the expert panel on a Likert scale from 1 (not important) to 9 (very important). A positive consensus (inclusion) was gathered for those items voted with a mean of over 7. A negative consensus (exclusion) was defined for those items voted with a mean of 3 or below.
Another round of discussion had to be made for those items voted from 3.1 to 6.9 as the average. The Delphi round 2 survey was designed to revote the factors that did not reach a consensus by expressing the same macro-concepts in a different way than round 1 to avoid bias. Fifteen items were brought forward in round 2.
The Delphi questionnaires for both round 1 and 2, and the definition of the macro-topics brought forth in round 2 are reported in Appendix 1.
Statistical analysis was conducted using R (RStudio version 2023.06.1.524) [26].
Results
Descriptive statistics
Thirty surgical leaders responded to round 1. The sample included practitioners from 14 countries, with Italy as the most represented one (12 participants, equal to 40%). Surgeons were mostly males, with only one female. The vast majority of them declared more than 20 years of experience in pancreatic surgery (21, 70% of the sample), and most of them were from academic institutions (26, 87%). 60% of them hold leadership roles as department chiefs, 73% of them were over 50 years old, more than half of the sample was from high-volume centers, with more than 81 surgical resections performed per year.
Table 1 reports some of the descriptive statistics about the sample.
Section 1 : organizational factors
The first section was about the organizational factors that were most important when establishing a pancreas unit. Among the initial 14 factors, half of them reached a consensus in round 1, while the others had to be brought forward in round 2.
The best-rated factor was the need to organize frequent meetings about multidisciplinary clinical professionals, which is an already common task in the multidisciplinary board. Other highly rated factors included the definition of team leaders for each clinical and organizational function, the presence of metrics and key performance indicators to assess the quality of the healthcare service, and the need to introduce case managers to support and guide the patient throughout the journey.
The items to be brought forth included the use of technology (e.g., telemedicine tools) to support the relationships with both staff and patients and knowledge dissemination through the press and media.
Table 2 reports the results of round 1 concerning the section about the organizational factors.
In round 2, all the remaining items got full consensus. However, the sample was not equally distributed, especially about the potential contribution of press and media, which recorded a standard deviation of 1.94, dividing the participants between those more open to the new tools and those skeptical.
Table 3 reports the results of round 2 concerning the section about the organizational factors.
Section 2 : stakeholders
The second section was about the stakeholders to be engaged in a pancreas unit. Notably, among the initial 18 subjects, only 3 of them (17%) reached a consensus in round 1, while the remaining 15 had to be brought forward in round 2.
The only actors that were recognized as necessary were those traditional medical professionals (like surgeons, oncologists, radiation therapists, and palliative care specialists) who are part of the already-established care path. These actors received an overall rating of 8.4 out of 9 and a low standard deviation of 0.61. The other two stakeholders who received a consensus (still with lower degrees) were non-traditional clinical professionals (like physiotherapists and psychologists) and the patient.
Table 4 reports the results of round 1 concerning the section about stakeholders.
Most of the stakeholders received a consensus while reconnected to those macro-themes brought forth to round 2, except for private firms and industry leaders (mean 5.99, standard deviation 2.12). Again, a high standard deviation denotes that the sample is widely distributed.
Table 5 reports the results of round 2 concerning the section about stakeholders.
Section 3 : non-technical skills
All the items about non-technical skills receive full consensus in round 1, without discussing and evaluating the topic further. Interestingly, the worst-rated factor was the importance of non-technical or soft skills in general terms. The best-rated skills were ethics, teamwork, professionalism, and leadership.
Table 6 reports the results of the section about non-technical skills.
Section 4: facilitators
The last section concerned the tools (technical, non-technical, technological, and creative) that could facilitate the knowledge-sharing dynamics within a pancreas unit. Notably, all the items received full consensus in round 1, without the need to continue the dialog in round 2. Still, not all the factors received the same level of agreement and importance.
The best-rated facilitators included mentoring and leadership, clinical cases, participation in national and international meetings, training, and clinical guidelines. The worst-rated items were co-production, leaflets and brochures, design elements, and testimonials.
Table 7 reports the results of the section about facilitators.
Discussion
The new pancreas units represent a unique and immense opportunity for pancreatic cancer care, including raising the quality of care for patients and the quality of work for clinical professionals. The new organizational model may bring several benefits to pancreatic surgeons, for instance, in the number of treated cases, professional development through networking, easier coordination with colleagues and patients thanks to the formal establishment of professional figures such as case managers, and more opportunities to connect with research institutions and industry leaders for joint projects and trials. Moreover, one more potential benefit of creating pancreas units may be reducing pancreatic surgeon burnout. Indeed, pancreatic surgery has elevated morbidity and mortality when compared to essentially every other intracavitary procedure. The development of pancreas units may enhance camaraderie among pancreatic surgeons, and the added support of non-surgical pancreatic experts such as round-the-clock interventional radiologists and endoscopists could help mitigate the difficulties of providing pancreatic surgical care [27, 28].
The debate about the most meaningful organizational factors, stakeholders, and procedures to be established in this new care concept is still open, and so is the design of an “ideal” pancreas unit. The results of the PUECOF study are intriguing and can contribute to the current debate on organizational innovation in surgery.
Regarding the organizational factors and the meaningful stakeholders, the enquired surgical leaders still seem stuck to a traditional model of care. Indeed, the best-rated item was about the need to carry on multidisciplinary meetings to discuss the patient’s case, a routine task that represents the primary paradigm in surgical oncology today. In line with this result, surgeons feel more comfortable enquiring those medical professionals who are part of the tumor board, such as surgeons, oncologists, radiation therapists, and palliative care specialists. They are also open to connecting and discussing with less traditional medical professionals, for instance, in the fields of nutrition and psychology, as recommended by the latest literature on pancreatic cancer care [9,10,11,12].
Interestingly enough, surgeons consider patients as relevant parties, while other stakeholders are not, neither the patient’s family nor the caregivers. These results are in contrast with the recognized pillars of the modern healthcare system, which is based on patient-centric concepts like co-production and shared decision-making. Modern oncology requires clinicians to engage the patient as much as possible, considering the circumstances [29,30,31], to co-design, co-plan, co-decide, and co-execute the oncological care [14, 32]. The concept of co-production has recently been also applied to surgery [14], and one first experience has been planned also in pancreatic cancer care [33]. Patients who are fully engaged in their own care record higher levels of satisfaction and adherence to the care plan [29, 30]. Therefore, it is important even for surgeons to second these elements when they are feasible.
Surgeons are also less likely to engage with other stakeholders, such as other clinicians from partner institutions or other pancreas units, universities, scientific societies, patients’ associations, NGOs, and industry firms. Surgical leaders seem less willing to go far beyond their operating room, as the meaningful partners they need are just outside it. Also these findings are in contrast with the most recent trends describing the healthcare ecosystem as an open one [34, 35], and the need for a multistakeholder approach [14], in which each actor has a role and can contribute to the ultimate goal, namely, the patient’s satisfaction and quality of care.
However, the role of professional figures such as nurse navigators, case managers [36], or advanced nurse practitioners [37] emerges. These professionals aim to connect the patients and the clinical staff, offering technical and non-technical support throughout the entire care journey. Surgeons are also sensitive to the organizational dimension through the definition of functional leaders and chiefs and the establishment of metrics and key performance indicators. In contrast, there is less trust in the use of telemedicine to support the relationships between medical professionals and the patient.
About the non-technical skills, in line with the current surgical literature [23, 25], surgical leaders recognized their importance. The best-rated items are represented by ethics, teamwork, professionalism, leadership, decision-making, and communication, which stress the importance of team dynamics within the operating room [38]. Interestingly, less importance is devoted to managing stress, ideas creation ability, agility, coping with fatigue, and coordination, even if pancreatic surgery is known to be technically complex with long operating times [39, 40].
Last but not least, concerning the facilitators, again, surgeons seem more comfortable when employing traditional instruments, like mentoring, clinical reports and critical review of complicated cases, participation in national and international meetings, training, clinical guidelines, and evidence-based methods. They have less trust in modern concepts like the above-mentioned co-production or marketing-oriented tools like leaflets and brochures, design and visual elements, and testimonials, who may share their personal experience with others.
Although the establishment of pancreas units will not change the technical content of pancreatic surgery, it can foster the progress of research and innovation thanks to the multistakeholder perspective in terms of new pharmaceutical treatments to improve resection rates, surgical techniques, or new frontiers in the use of telemedicine and e-health tools in pancreatic care and follow-up. It is an exciting scenario where everyone must contribute and offer an effort to change the paradigm to fight one of the worst oncological diseases.
Conclusions
The debate on the new pancreas units has just started. Our exciting results depict a picture that sees surgical leaders still comfortable in their traditional role. Indeed, those organizational factors that reached full consensus are those closer to the actual situation and procedures, while surgeons are still reluctant to recognize more modern concepts like multistakeholder engagement and co-production dynamics.
The above-described scenario has a substantial impact on new essential needs in surgical education for the next generation of surgical oncologists. Both academic institutions and scientific societies will have the strategic role of promoting such a paradigm shift, sharing knowledge and best practices about what is and will go on in pancreatic cancer care.
Limitations
As with all pieces of research, ours has limitations. First of all, our Delphi panel members are not equally distributed, with many coming from Italy, where the debate on pancreas units is particularly lively because of the recent regulation of the Lombardy Region [13, 41] and the creation of a dedicated focus group by the Ministery of Health [42]. Despite our efforts, gender diversity is not met, with only 1 woman out of 30 total participants, reflecting the scenario of a (still) male-dominated domain. Moreover, the literature and the topic of pancreas units are still in their infancy. As the theme progresses, we may expect more intriguing inputs and experiences to be included in the debate. Inquiring different clinical professionals other than surgeons, such as oncologists, gastroenterologists, and also nurses, about their perception of the meaningful organizational factors may create valuable synergies with the thoughts of surgical leaders. Our limitations can, therefore, represent new exciting research avenues for researchers in surgery and healthcare management to design, disseminate, and assess the “ideal” pancreas unit model of care.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Vonlanthen R, Lodge P, Barkun JS, Farges O, Rogiers X, Soreide K et al (2018) Toward a consensus on centralization in surgery. Ann Surg 268(5):712–724
Balzano G, Guarneri G, Pecorelli N, Paiella S, Rancoita PMV, Bassi C et al (2020) Modelling centralization of pancreatic surgery in a nationwide analysis. Br J Surg 107(11):1510–1519
Balzano G, Guarneri G, Pecorelli N, Reni M, Capurso G, Falconi M (2021) A four-step method to centralize pancreatic surgery, accounting for volume, performance and access to care. HPB Off J Int Hepato Pancreato Biliary Assoc 23(7):1095–1104
Ahola R, Sand J, Laukkarinen J (2020) Centralization of pancreatic surgery improves results: review. Scand J Surg. 109(1):4–10
Nymo LS, Søreide K, Kleive D, Olsen F, Lassen K (2019) The effect of centralization on short term outcomes of pancreatoduodenectomy in a universal health care system. HPB 21(3):319–327
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin. 72(1):7–33. https://doi.org/10.3322/caac.21708
Frassini S, Calabretto F, Granieri S, Fugazzola P, Viganò J, Fazzini N et al (2022) Intraperitoneal chemotherapy in the management of pancreatic adenocarcinoma: a systematic review and meta-analysis. Eur J Surg Oncol. https://doi.org/10.1016/j.ejso.2022.05.030
Barcellini A, Peloso A, Pugliese L, Vitolo V, Cobianchi L (2020) Locally advanced pancreatic ductal adenocarcinoma: challenges and progress. Onco Targets Ther 13:12705–12720
Vashi P, Popiel B, Lammersfeld C, Gupta D (2015) Outcomes of systematic nutritional assessment and medical nutrition therapy in pancreatic cancer. Pancreas 44(5):750–755
Carrato A, Cerezo L, Feliu J, Macarulla T, Martín-Pérez E, Vera R et al (2022) Clinical nutrition as part of the treatment pathway of pancreatic cancer patients: an expert consensus. Clin Transl Oncol. 24(1):112–126
Bauer MR, Bright EE, Macdonald JJ, Cleary EH, Hines OJ, Stanton AL (2018) Quality of life in patients with pancreatic cancer and their caregivers: a systematic review. Pancreas 47(4):368–375
Shakin EJ, Holland J (1988) Depression and pancreatic cancer. J Pain Symptom Manage 3(4):194–198
Dal Mas F, Previtali P, Denicolai S, Venturi A, Campostrini S, Cogliati PG et al (2023) A multidisciplinary approach to care. A Delphi consensus on the case of Pancreas Units. In: Martellucci J, Dal Mas F (eds) Towards the future of surgery. Springer, Cham, pp 147–171. https://doi.org/10.1007/978-3-031-47623-5_13
Cobianchi L, Dal Mas F, Massaro M, Bednarova R, Biancuzzi H, Filisetti C et al (2022) Hand in hand: a multistakeholder approach for Co-production of surgical care. Am J Surg 223(1):214–215
Griffioen IPM, Rietjens JAC, Melles M, Snelders D, Homs MYV, Van ECH et al (2021) The bigger picture of shared decision making: a service design perspective using the care path of locally advanced pancreatic cancer as a case. Cancer Med 10(June):5907–5916
Sacks GD, Shin P, Braithwaite RS, Soares KC, Kingham TP, D’Angelica MI et al (2023) The influence of patient preference on surgeons’ treatment recommendations in the management of intraductal papillary mucinous neoplasms. Ann Surg 278(5):E1068–E1072
Ziebland S, Chapple A, Evans J (2015) Barriers to shared decisions in the most serious of cancers: a qualitative study of patients with pancreatic cancer treated in the UK. Heal Expect. 18(6):3302–3312
Bresnen M, Hodgson D, Bailey S, Hassard J, Hyde P (2019) Hybrid managers, career narratives and identity work: a contextual analysis of UK healthcare organizations. Hum Relations 72(8):1341–1368
Giacomelli G, Ferré F, Furlan M, Nuti S (2019) Involving hybrid professionals in top management decision-making: how managerial training can make the difference. Heal Serv Manag Res 32(4):168–179
Linstone HA, Turoff M (2010) Delphi: a brief look backward and forward. Technol Forecast Soc Change 78(9):1712–1719
Keeney S, Hasson F, McKenna H (2011) The Delphi technique in nursing and health research. Wiley-Blackwell, Hoboken, pp 1–208
Dal Mas F, Garcia-Perez A, Sousa MJ, Lopes da Costa R, Cobianchi L (2020) Knowledge translation in the healthcare sector a structured literature review. Electron J Knowl Manag. 18(3):198–211
Stahel PF, Cobianchi L, Dal Mas F, Paterson-Brown S, Sakakushev BE, Nguyen C et al (2022) The role of teamwork and non-technical skills for improving emergency surgical outcomes: an international perspective. Patient Saf Surg. 16(1):1–10. https://doi.org/10.1186/s13037-022-00317-w
Dal Mas F, Bagarotto EM, Cobianchi L (2021) Soft skills effects on knowledge translation in healthcare. Evidence from the field. In: Lepeley MT, Beutell N, Abarca N, Majluf N (eds) soft skills for human centered management and global sustainability. Routledge, New York, pp 95–109. https://doi.org/10.4324/9781003094463-7-11
Pradarelli JC, Gupta A, Lipsitz S, Blair PG, Sachdeva AK, Smink DS et al (2020) Assessment of the Non-Technical Skills for Surgeons (NOTSS) framework in the USA. Br J Surg 107(9):1137–1144
R Development Core Team. The R Manuals. R. 2021. https://cran.r-project.org/manuals.html. Accessed 12 Mar 2021.
Reid M, Lee A, Urbach DR, Kuziemsky C, Hameed M, Moloo H et al (2021) Shared care in surgery: practical considerations for surgical leaders. Healthc Manag Forum. 34(2):77–80
Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D et al (2010) Burnout and medical errors among american surgeons. Ann Surg 251(6):995–1000
Elwyn G, Nelson E, Hager A, Price A (2020) Coproduction: when users define quality. BMJ Qual Saf 29(9):711–716
Batalden M, Batalden P, Margolis P, Seid M, Armstrong G, Opipari-arrigan L et al (2016) Coproduction of healthcare service. BMJ Qual Saf 25(7):509–517
Petersson C, Batalden P, Fritzell P, Borst S, Hedberg B (2019) Exploring the meaning of coproduction as described by patients after spinal surgery interventions. Open Nurs J 13(1):85–91
Dal Mas F, Biancuzzi H, Massaro M, Miceli L (2020) Adopting a knowledge translation approach in healthcare co-production. A case study. Manag Decis 58(9):1841–1862. https://doi.org/10.1108/MD-10-2019-1444
Cobianchi L, Dal Mas F, Pizzocaro E, Tripepi M, Butturini G (2023) Co-design, co-learning, and co-production of an app for pancreatic cancer patients—the “Pancreas Plus” study protocol. mHealth. https://doi.org/10.21037/mHealth-22-48
Secundo G, Toma A, Schiuma G, Passiante G (2019) Knowledge transfer in open innovation: a classification framework for healthcare ecosystems. Bus Process Manag J 25(1):144–163
Dal Mas F, Massaro M, Rippa P, Secundo G (2023) The challenges of digital transformation in healthcare: an interdisciplinary literature review, framework, and future research agenda. Technovation 123:102716. https://doi.org/10.1016/j.technovation.2023.102716
Bashkin O, Asna N, Amoyal M, Dopelt K (2023) the role of nurses in the quality of cancer care management: perceptions of cancer survivors and oncology teams. Semin Oncol Nurs. 39(4):151423
Htay M, Whitehead D (2021) The effectiveness of the role of advanced nurse practitioners compared to physician-led or usual care: a systematic review. Int J Nurs Stud Adv. 3:100034
Cobianchi L, Dal Mas F, Massaro M, Fugazzola P, Coccolini F, Kluger Y et al (2021) Team dynamics in emergency surgery teams: results from a first international survey. World J Emerg Surg 16:47. https://doi.org/10.1186/s13017-021-00389-6
Damoli I, Butturini G, Ramera M, Paiella S, Marchegiani G, Bassi C (2015) Minimally invasive pancreatic surgery - a review. Wideochirurgia i inne Tech maloinwazyjne. 10(2):141–149
Strobel O, Neoptolemos J, Jäger D, Büchler MW (2019) Optimizing the outcomes of pancreatic cancer surgery. Nat Rev Clin Oncol 16(1):11–26
Regione Lombardia. Determinazioni in merito all’attivazione della rete regionale dei centri di diagnosi e cura dei tumori al pancreas (Pancreas Unit). Milano: Regione Lombardia; 2022 p. Deliberazione XI / 6241.
Governo e Parlamento. Istituita al Ministero della Salute una cabina di regia per la Rete Centri Pancreas Unit. Quotidiano Sanità. 2024 Mar 20; https://www.quotidianosanita.it/governo-e-parlamento/articolo.php?articolo_id=121007&fr=n
Funding
Open access funding provided by Università degli Studi di Pavia within the CRUI-CARE Agreement. No funding was received to assist with preparing this manuscript.
Author information
Authors and Affiliations
Contributions
LC and FDM conceived the idea of the study. LC, FDM, GM, GBu, and IF are part of the E-AHPBA PUECOF steering committee. LC and FDM conceived the study protocol and survey. GM, GBu, and IF reviewed the study protocol and survey. MAH, MA, SA, GBal, GBar, CB, MGB, MB, UB, KCC, RC, CD, SD, MF, GKF, AAG, AI, RM, DR, JMR, ER, RS, ASa, ASe, AKS, SS, OS, AZ, GM, and GBu participated in the data collection. FDM took care of data analysis. LC and FDM wrote the first draft of the paper. All the authors critically reviewed the paper before its submission.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no relevant financial or nonfinancial interests to disclose.
Ethical approval
Not applicable.
Human participants
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Delphi questionnaire: round 1
HPB surgical leaders’ expert consensus on the organizational factors of a formally established pancreas unit
Section 0: descriptive statistics
1. How many years of experience in pancreatic surgery do you have?
-
1.
< 10
-
2.
11 to 20
-
3.
> 20
2. What kind of institution do you work for?
-
1.
Academic
-
2.
Non-academic
3. What is your current position?
-
1.
Board-certified surgeon
-
2.
Senior consultant
-
3.
Head of the department
4. How many pancreatic resections does your institution perform every year?
-
1.
< 30
-
2.
from 31 to 50
-
3.
from 51 to 80
-
4.
over 81
5. What is your gender?
-
1.
Male
-
2.
Female
-
3.
Prefer not to answer
6. What is your age group?
-
1.
Under 40
-
2.
1–50
-
3.
50–60
-
4.
Over 60
7. Do you agree to be an author in the scientific publication(s) reporting the Delphi results?
-
1.
Yes
Section 1: organizational factors (14 items)
The aim of the section is to gather expert consensus on the importance of some organizational factors. Although all of them may seem perceived as relevant, please assess them by ranking seven and up only those elements that, to you, should have the priority in the establishment of a multidisciplinary pancreas unit.
In a pancreas unit, how would you rate the importance of the following items from 1 to 9, where: 1 = not important at all, 9 = very important, when it comes to the organizational factors in pancreatic cancer care? | Importance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
1 | Organizing frequent meetings among multidisciplinary clinical professionals | |||||||||
2 | The presence of metrics/key performance indicators assessing all steps of the patient journey | |||||||||
3 | Having spaces fully dedicated to the pancreas unit | |||||||||
4 | Defining team leaders for each clinical and organizational function | |||||||||
5 | Using new technologies (e.g., telemedicine) in managing collaboration and work relations within the unit’s staff | |||||||||
6 | Using new technologies (e.g., telemedicine) in managing the relations with the patients | |||||||||
7 | Sharing knowledge, cases, … with other pancreas units | |||||||||
8 | Disseminate knowledge by being present on the local press | |||||||||
9 | Disseminate knowledge by being present on social media | |||||||||
10 | Defining multidisciplinary clinical training paths for all the unit’s staff members | |||||||||
11 | Defining multidisciplinary management/organizational training paths for all the unit’s staff members | |||||||||
12 | Integrating data across clinical and administrative unit | |||||||||
13 | Introducing “case managers”, in charge to follow the patient and the case over different clinic departments/expertise | |||||||||
14 | Covering all patients journey, in an “extended view”, starting from prevention (e.g., promotion of good habits like avoiding smoke and alcohol and enhancing physical activity) and early diagnosis (increasing awareness in familial cases through National Registry inclusion; spreading the culture about the most common non-specific symptoms like back pain, diabetes, wight loss, steatorrhea,..) | |||||||||
Section 2: stakeholders (18 items)
The aim of the section is to gather expert consensus on the importance of engaging certain stakeholders, than others. Although all of them may seem perceived as relevant, please assess them by ranking seven and up only those actors that, to you, should have the priority in the establishment of a multidisciplinary pancreas unit.
In a pancreas unit, how would you rate the importance of the following items from 1 to 9, where: 1 = not important at all 9 = very important when it comes to stakeholders' engagement in pancreatic cancer care? | Importance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
1 | Involving traditional clinical professionals (e.g., surgeons, oncologists, radiation therapists, palliative care specialists, …) | |||||||||
2 | Involving non-traditional clinical professionals (physiotherapists, psychologists, …) | |||||||||
3 | Involving clinicians from partner institutions according to a hub/spokes model | |||||||||
4 | Involving the patient | |||||||||
5 | Involving the patient’s family | |||||||||
6 | Involving the patients’ associations | |||||||||
7 | Involving other NGOs (non-governmental organizations) and no-profit entities | |||||||||
8 | Involving other public sector entities | |||||||||
9 | Involving ethical committees | |||||||||
10 | Involving clinicians from international institutions | |||||||||
11 | Involving scientific societies | |||||||||
12 | Involving other pancreas units | |||||||||
13 | Involving pure research institutions and universities | |||||||||
14 | Involving private firms/companies active in the pharma sector | |||||||||
15 | Involving private firms/companies active in the biotech sector | |||||||||
16 | Involving private firms/companies active in the surgical technology sector | |||||||||
17 | Involving private firms/companies active in the media sector | |||||||||
18 | Involving colleagues characterized by diverse features | |||||||||
Section 3: non-technical skills (1 + 16 items)
Non-technical skills appear today as a key topic in surgical practice. Non-technical or soft skills represent those personal features and traits that facilitate the relationships with others—namely, team members, colleagues from other disciplines, the patient and families, and other stakeholders like other institutions, communities, scientific societies. The aim of the section is to gather expert consensus on the importance of some non-technical skills. Although all of them may seem perceived as relevant, please assess them by ranking seven and up only those features that, to you, can facilitate the relationships within all the stakeholders of the pancreas unit.
In a pancreas unit, how would you rate the importance of non-technical or soft skills from 1 to 9, where: 1 = not important at all, 9 = very important, when it comes to pancreatic cancer care? | Importance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
1 | Non-technical or soft skills in general terms | |||||||||
In a pancreas unit, how would you rate the importance of the following items from 1 to 9, where: 1 = not important at all, 9 = very important, when it comes to non-technical skills in pancreatic cancer care? | Importance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
1 | Decision-making | |||||||||
2 | Coping with fatigue | |||||||||
3 | Communication | |||||||||
4 | Leadership | |||||||||
5 | Situational awareness | |||||||||
6 | Managing stress | |||||||||
7 | Team working | |||||||||
8 | Ideas creation ability | |||||||||
9 | Coordination ability | |||||||||
10 | Multicultural ability | |||||||||
11 | Planning ability | |||||||||
12 | Learning ability | |||||||||
13 | Professionalism | |||||||||
14 | Information management ability | |||||||||
15 | Agility | |||||||||
16 | Ethics | |||||||||
Section 4: processes and knowledge translation facilitators (31 items)
The relationships among the various actors in a pancreas unit and among different pancreas units (from the surgical and the clinical staff to the patients, from the other institutions to the scientific societies) can be tough. The aim of the section is to gather expert consensus on the importance of some tools and facilitators that can enhance the outcome of such relationships. Although all of them may seem perceived as relevant, please assess them by ranking seven and up only those tools that, to you, can facilitate the relationships within all the stakeholders of the pancreas unit.
In a pancreas unit, how would you rate the importance of the following items from 1 to 9, where: 1 = not important at all, 9 = very important, when it comes to facilitators in pancreatic cancer care? | Importance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
1 | The pathogenesis and mechanisms behind diseases | |||||||||
2 | Mobile electronic medical records and online tools | |||||||||
3 | Design | |||||||||
4 | Web portals | |||||||||
5 | Image tagging | |||||||||
6 | Lesson learned and best practices | |||||||||
7 | Tours to share experiences with others | |||||||||
8 | Committees and meetings | |||||||||
9 | Journal publications | |||||||||
10 | In-person visit and talking | |||||||||
11 | Establishment of mixed teams | |||||||||
12 | Co-production | |||||||||
13 | Leaflets and brochures | |||||||||
14 | Training | |||||||||
15 | Clinical cases and critical review of complicated cases | |||||||||
16 | Clinical guidelines | |||||||||
17 | Use of interpersonal skills | |||||||||
18 | Discussions, debates, curiosity | |||||||||
19 | New technological tools | |||||||||
20 | Mentoring and leadership | |||||||||
21 | Testimonials | |||||||||
22 | Engaging with the patient's family | |||||||||
23 | Empowerment | |||||||||
24 | Community of practice | |||||||||
25 | Multidisciplinary people (e.g., degree in medicine + IT) | |||||||||
26 | Use of evidence-based methods | |||||||||
27 | Quality assessment by stakeholders | |||||||||
28 | Partecipation in national and international meetings | |||||||||
29 | Simulations | |||||||||
30 | Self-assessment | |||||||||
31 | Use of a simple language | |||||||||
Delphi questionnaire: Round 2
Definition of new macro-topics

In a pancreas unit, how would you rate the importance of the following items from 1 to 9, where:
1= not important at all,
9 = very important,
when it comes to the organizational factors in pancreatic cancer care?
In a pancreas unit, how would you rate the importance of the following items from 1 to 9, where: 1 = fully disagree, 5 = neutral, 9 = fully agree, when it comes to the organizational factors in pancreatic cancer care? | Importance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
1 | Clinical results should be shared with industry partners (technological and surgical device producers, pharma companies, …) to enhance progress in pancreatic cancer care | |||||||||
2 | Industry partners should be encouraged to promote and finance projects along with pancreas units | |||||||||
3 | Industry partners (technological and surgical device producers, pharma companies, …) may represent meaningful stakeholders in pancreatic cancer care | |||||||||
4 | Patients’ associations and other nonprofit entities can provide patients and institutions with meaningful support—providing patients with assistance | |||||||||
5 | Patients’ associations and other nonprofit entities can provide patients and institutions with meaningful support—raising funds | |||||||||
6 | Patients’ associations and other nonprofit entities can provide patients and institutions with meaningful support—spreading information about the care path | |||||||||
7 | Disseminating general information about pancreatic cancer can be helpful for the population | |||||||||
8 | Social media networks represent a solid channel for disseminating general information about pancreatic cancer | |||||||||
9 | The press represents a solid channel for disseminating general information about pancreatic cancer | |||||||||
10 | Clinical results should be shared among the pancreatic surgical community to enhance progress in pancreatic cancer care | |||||||||
11 | Clinical results should be shared among the multidisciplinary pancreatic medical community to enhance progress in pancreatic cancer care | |||||||||
12 | Experimental trials can enhance progress in pancreatic cancer care | |||||||||
13 | The availability of electronic medical records and other digital patients’ data can facilitate work within the multidisciplinary care team | |||||||||
14 | There are effective e-health tools that pancreatic surgeons can use to take care of their patients, e.g., for teleconsultation | |||||||||
15 | Clinical results should be shared with industry partners in the e-health business to enhance progress in designing and experimenting new telemedicine tools for pancreatic cancer care | |||||||||
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cobianchi, L., Dal Mas, F., Abu Hilal, M. et al. Toward a new paradigm of care: a surgical leaders’ Delphi consensus on the organizational factors of the new pancreas units (E-AHPBA PUECOF study). Updates Surg (2024). https://doi.org/10.1007/s13304-024-01839-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01839-x