Abstract
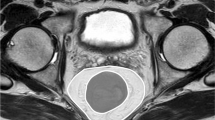
The aim of this study was to evaluate whether the mesorectal fat area (MFA) has an impact on the histopathology metrics of the specimen in male patients undergoing robotic total mesorectal excision (rTME) for cancer in the distal third of the rectum. Prospectively collected data of patients undergoing rTME for resectable rectal cancer by five surgeons during 3 years were extracted from the REgistry of Robotic SURgery for RECTal cancer (RESURRECT). MFA was measured at preoperative MRI. Distal rectal cancer was defined as within 6 cm from the anal verge. Specimen metrics included circumferential resection margin (CRM) measured by pathologists as involved if < 1 mm, distal resection margin (DRM) and TME quality. Of 890 patients who underwent rTME for rectal cancer, a subgroup analysis compared 116/581 (33.4%) with MFA > 20 cm2 to 231/581 (66.6%) with MFA ≤ 20 cm2. The mean CRM in patients with MFA > 20 cm2 was neither statistically nor clinically significantly different from patients with MFA ≤ 20 m2 (6.8 ± 5.6 mm vs. 6.0 ± 7.5 mm; p = 0.544). The quality of TME did not significantly differ: complete TME 84.3% vs. 80.3%; nearly complete TME 12.9% vs. 10.1%; incomplete TME 6.8% vs. 5.6%. The DRM was not significantly different: 1.9 ± 1.9 cm vs. 1.9 ± 2.5 cm; p = 0.847. In addition, the intraoperative complication rate was not significantly different: 4.3% (n = 5) vs. 2.2% (n = 5) (p = 0.314). This prospective multicenter study did not find any evidence to support that larger MFA would result in poorer histopathology metrics of the specimen when performing rTME in male patients with distal rectal cancer.




Similar content being viewed by others
References
Chapuis P, Bokey L, Fahrer M, Sinclair G, Bogduk N (2002) Mobilization of the rectum: anatomic concepts and the bookshelf revisited. Dis Colon Rectum 45:1–8. https://doi.org/10.1007/s10350-004-6104-5
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the alacart randomized clinical trial. JAMA 314:1356–1363. https://doi.org/10.1001/jama.2015.12009
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage ii or iii rectal cancer on pathologic outcomes: the acosog z6051 randomized clinical trial. JAMA 314:1346–1355. https://doi.org/10.1001/jama.2015.10529
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774. https://doi.org/10.1016/S1470-2045(14)70205-0
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332. https://doi.org/10.1056/NEJMoa1414882
Tou S, Bergamaschi R (2016) Laparoscopic rectal cancer resection: inferior to open or not? Colorectal Dis 18:233. https://doi.org/10.1111/codi.13270
Weaver KL, Grimm LM Jr, Fleshman JW (2015) Changing the way we manage rectal cancer-standardizing TME from open to robotic (including laparoscopic). Clin Colon Rectal Surg 28:28–37. https://doi.org/10.1055/s-0035-1545067
Ballian N, Yamane B, Leverson G, Harms B, Heise CP, Foley EF et al (2010) Body mass index does not affect postoperative morbidity and oncologic outcomes of total mesorectal excision for rectal adenocarcinoma. Ann Surg Oncol 17:1606–1613. https://doi.org/10.1245/s10434-010-0908-4
Ballian N, Lubner MG, Munoz A, Harms BA, Heise CP, Foley EF et al (2012) Visceral obesity is associated with outcomes of total mesorectal excision for rectal adenocarcinoma. J Surg Oncol 105:365–370. https://doi.org/10.1002/jso.22031
Son IT, Kim DW, Choe EK, Kim YH, Lee KH, Ahn S et al (2019) Oncologic evaluation of obesity as a factor in patients with rectal cancer undergoing laparoscopic surgery: a propensity-matched analysis using body mass index. Ann Surg Treat Res. 96:86–94. https://doi.org/10.4174/astr.2019.96.2.86
Kang J, Baek SE, Kim T, Hur H, Min BS, Lim JS et al (2012) Impact of fat obesity on laparoscopic total mesorectal excision: more reliable indicator than body mass index. Int J Colorectal Dis 27:497–505. https://doi.org/10.1007/s00384-011-1333-2
Kartheuser AH, Leonard DF, Penninckx F, Paterson HM, Brandt D, Remue C et al (2013) Waist circumference and waist/hip ratio are better predictive risk factors for mortality and morbidity after colorectal surgery than body mass index and body surface area. Ann Surg 258:722–730. https://doi.org/10.1097/SLA.0b013e3182a6605a
Jung M, Volonte F, Buchs NC, Gayet-Ageron A, Pugin F, Gervaz P et al (2014) Perirenal fat surface area as a risk factor for morbidity after elective colorectal surgery. Dis Colon Rectum 57:201–209. https://doi.org/10.1097/DCR.0000000000000029
Boyle KM, Chalmers AG, Finan PJ, Sagar PM, Burke D (2009) Morphology of the mesorectum in patients with primary rectal cancer. Dis Colon Rectum 52:1122–1129. https://doi.org/10.1007/DCR.0b013e31819ef62f
Allen SD, Gada V, Blunt DM (2007) Variation of mesorectal volume with abdominal fat volume in patients with rectal carcinoma: assessment with MRI. Br J Radiol 80:242–247. https://doi.org/10.1259/bjr/66311683
Yamaoka Y, Yamaguchi T, Kinugasa Y, Shiomi A, Kagawa H, Yamakawa Y et al (2019) Mesorectal fat area as a useful predictor of the difficulty of robotic-assisted laparoscopic total mesorectal excision for rectal cancer. Surg Endosc 33:557–566. https://doi.org/10.1007/s00464-018-6331-9
Escal L, Nougaret S, Guiu B, Bertrand MM, de Forges H, Tetreau R et al (2018) MRI-based score to predict surgical difficulty in patients with rectal cancer. Br J Surg 105:140–146. https://doi.org/10.1002/bjs.10642
Gachabayov M, You K, Kim SH, Yamaguchi T, Jimenez-Rodriguez R, Kuo LJ et al (2019) Meta-analysis of the impact of the learning curve in robotic rectal cancer surgery on histopathologic outcomes. Surg Technol Int 34:139–155
Pan AF, Zheng NX, Wang J, Kabemba JLT, Zheng K, Shen F et al (2022) Role of perirectal fat in the carcinogenesis and development of early-onset rectal cancer. J Oncol 2022:4061142. https://doi.org/10.1155/2022/4061142
Acknowledgements
RESURRECT Study Group: Seon-Hahn Kim, Colorectal Division, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, South Korea. Guglielmo Niccolo Piozzi, Colorectal Division, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, South Korea. Rosa Jimenez-Rodriguez, Section of Colorectal Surgery, Hospital Universitario Virgen del Rocio, Sevilla, Spain. Li-Jen Kuo, Division of Colorectal Surgery, Department of Surgery, Taipei Medical University Hospital, Taipei, Taiwan. Tomohiro Yamaguchi, Division of Colon and Rectal Surgery, Shizuoka Cancer Center Hospital, Shizuoka, Japan. Fabio Cianchi, Department of Surgery and Translational Medicine, Careggi Hospital, University of Florence, Florence, Italy. Oktar Asoglu, Bosphorus Clinical Research Academy, Istanbul, Turkey. Vusal Aliyev, Department of General Surgery, Istanbul Florence Nightingale Hospital, Istanbul, Turkey. Dejan Ignjatovic, Surgical Department, Akershus University Hospital, Lørenskog, Norway. Yosef Nasseri, Cedar Sinai Medical Center, Los Angeles, CA, USA. Moshe Barnajian, Cedar Sinai Medical Center, Los Angeles, CA, USA.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All the authors disclose financial or non-financial interests that are directly or indirectly related to the work submitted for publication.
Research involving human participants and/or animals
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by Western Institutional Review Board (reference number: 1-1329396-1).
Informed consent
Informed consent was obtained from all the individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Felsenreich, D.M., Gachabayov, M., Bergamaschi, R. et al. Does the mesorectal fat area impact the histopathology metrics of the specimen in males undergoing TME for distal rectal cancer?. Updates Surg 75, 581–588 (2023). https://doi.org/10.1007/s13304-022-01429-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-022-01429-9