Abstract
Introduction
Since early 2020 the whole world has been challenged by the SARS-CoV-2 virus and the associated global pandemic (Covid-19). People with diabetes are particularly at high risk of becoming seriously unwell after contracting this virus.
Methods
This population-based study included people living in the Greater Manchester conurbation who had a recorded diagnosis of type 1 diabetes mellitus (T1DM) or type 2 diabetes mellitus (T2DM) and subsequent Covid-19 infection. Each individual with T1DM (n = 862) or T2DM (n = 13,225) was matched with three Covid-19-infected non-diabetes controls.
Results
For individuals with T1DM, hospital admission rate in the first 28 days after a positive Covid-19 test was 10% vs 4.7% in age/gender-matched controls [relative risk (RR) 2.1]. For individuals with T2DM, hospital admission rate after a positive Covid-19 test was 16.3% vs 11.6% in age/gender-matched controls (RR 1.4). The average Townsend score was higher in T2DM (1.8) vs matched controls (0.4), with a higher proportion of people with T2DM observed in the top two quintiles of greatest disadvantage (p < 0.001). For Covid-19-infected individuals with T1DM, factors influencing admission likelihood included age, body mass index (BMI), hypertension, HbA1c, low HDL-cholesterol, lower estimated glomerular filtration rate (eGFR), chronic obstructive pulmonary disease (COPD) and being of African/mixed ethnicity. In Covid-19-infected individuals with T2DM, factors related to a higher admission rate included age, Townsend index, comorbidity with COPD/asthma and severe mental illness (SMI), lower eGFR. Metformin prescription lowered the likelihood. For multivariate analysis in combined individuals with T2DM/controls, factors relating to higher likelihood of admission were having T2DM/age/male gender/diagnosed COPD/diagnosed hypertension/social deprivation (higher Townsend index) and non-white ethnicity (all groups).
Conclusion
In a UK population we have confirmed a significantly higher likelihood of admission in people with diabetes following Covid-19 infection. A number of factors mediate that increased likelihood of hospital admission. For T2DM, the majority of factors related to increased admission rate are common to the general population but more prevalent in T2DM. There was a protective effect of metformin in people with T2DM.
Similar content being viewed by others
People with diabetes are at particularly high risk of becoming seriously unwell and being hospitalised after contracting SARS-CoV-2 |
The relative risk of hospital admission vs matched controls was higher for individuals with T1DM than individuals with T2DM |
A number of factors including BMI, blood pressure, taking metformin, socioeconomic situation and ethnicity have been identified in this study as potentially mediating that increased likelihood of hospital admission |
For T2DM, the majority of factors related to increased risk of admission are common to the general population but are known to be more prevalent in T2DM |
Nevertheless our analysis suggests that there are as yet unknown factors which are modulating that risk |
Introduction
Since early 2020 the whole world has been challenged by the SARS-CoV-2 virus and its associated pandemic (Covid-19) [1]. People with diabetes are known to be at a higher risk of becoming unwell and dying following Covid-19 infection, when compared to people living without diabetes [2,3,4]. Barron et al. [4] reported a higher odds ratio (OR) for in-hospital Covid-19-related death for people with type 2 diabetes (T2DM) in the UK. A subsequent body of work is emerging in relation to why people with diabetes are more likely to become seriously unwell following a Covid-19 infection and why they are admitted into hospital. However a full appreciation of risk factors and their relative contributions to serious outcomes are as yet not fully available. Hippisley-Cox et al. [5] recently described a risk model for hospital admission post Covid-19 infection, using pooled National Health Service (NHS) primary care data.
In the CORONADO study [6] of people with diabetes hospitalized following a Covid-19 infection, multivariable analysis revealed that only body mass index (BMI) remained positively associated with the primary outcomes of death or assisted mechanical ventilation. Neither long-term glycaemic control (as assessed by HbA1c measurement) nor regular treatment with a renin–angiotensin–aldosterone system (RAAS) blocker were associated with a more adverse outcome following Covid-19 infection. Increasing age, microvascular and macrovascular complications were independently associated with death in the course of the hospital admission.
For people with diabetes, the last 18 months have been a very challenging time because their condition puts them at significantly increased risk of becoming seriously unwell or dying following a Covid-19 infection [6]. Therefore, it is critical to understand how much a previous diagnosis of T1DM or T2DM and which aspects and comorbidities of their condition increase their risk of becoming seriously unwell and being admitted to hospital following a Covid-19 infection. Such information and insight are pivotal in order to provide better care.
The aim of this study was to identify potential factors relating to an increased likelihood of hospital admission in individuals with diabetes, to assess the difference in risk between individuals with and without diabetes and to investigate if any difference in risk could be explained by routinely measured factors.
Methods
This was a retrospective study. Study participants included all people who had a recorded diagnosis of T1DM or T2DM living in the UK Greater Manchester conurbation (total population 2.85 million) who were alive on 1 January 2020 and who had a proven Covid-19 infection, based on a recorded positive test in the general practice record. Each individual with diabetes (T1DM or T2DM) was matched with three controls—that is three people without diabetes matched for age and gender who had also tested positive within a 28-day period for a Covid-19 infection.
Data were de-identified at source and were extracted from the Greater Manchester Care Record (GMCR) database [7]. The follow-up period started on 1 January 2020 and ended on 31 May 2021. The GMCR pools information all general practices across the conurbation. The project was approved and overseen by Health Innovation Manchester [8], which is comparable to an ethics committee in relation to the management and supervision of access to the population health records of citizens of Greater Manchester for research purposes. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. This study was conducted in accordance with ethical guidelines.
The data were put through a rigorous checking and data cleaning process where all values were ‘sense checked’ for credible physiological ranges and internal clinical and demographic logic (e.g. dates of birth, height, weight, BMI, biomarker ranges). BMI was included only if recorded within 6 months of the positive Covid-19 test. We excluded digital health records with missing data. Statistical analyses were performed on the final data set to investigate the potential risk factors contributing to increased likelihood for hospital admission in diabetes following infection with Covid-19. Social disadvantage was described by Townsend score [9]. A higher Townsend index equates to greater social disadvantage. The Townsend score is contained within the NHS general practice record of all UK citizens and is a census-based index of material status calculated by the combination of four census variables. The Townsend index is an area-based measure and can be constructed for any geographical area for which UK census data are available. The 2001 census and NHS five groups were used to define ethnicity.
In order to take account of Covid-19 positive status being confirmed after hospital admission, we included all individuals with a Covid-19 virus positive test within 48 h of admission, in our analysis.
Following cleaning the data extracted were split into two cohorts:
-
Those with T1DM and their controls (1:3 matching)
-
Those with T2DM and their controls (1:3 matching)
Statistics
Digital health records often contain missing data and for medications and diagnosis. We assumed that missing data for these variables meant individuals were not on the medication or had a specific diagnosis. Imputation in relation to the comparison between individuals with diabetes and individuals without diabetes was not possible because of the degree of difference in availability of anthropometric and metabolic variables between the two groups. Therefore a complete case analysis was conducted. Comparison between continuous variables was by analysis of variance (ANOVA).
All substantive modelling was logistic regression, with 28-day hospital admission as the binary outcome variable, and diabetes status as the main exposure variable. Other variables were adjusted for in specific models, as detailed below. Townsend score comparisons were relative to a Townsend score of 1.
In order to investigate potential factors associated with admission of patients with diabetes we analysed the individuals with T1DM and those with T2DM, without the matched individuals, separately. To do so, we used univariate logistic regression, considering each possible factor in turn, for the two groups separately.
We then studied whether the difference in risk between patients with diabetes and patients without diabetes was explained by other measured factors. In order to do so we analysed each diabetes group with their matched cohort and compared the OR of diabetes in a model including only age, sex and diabetes with the OR of diabetes when adjusted for each additional factor in turn. Change of the diabetes OR in this comparison can be interpreted as the additional factor explaining part of the association between diabetes and hospitalisation (e.g. through confounding or mediation).
Finally, we fitted a fully adjusted multivariable model, separately in each matched cohort, to measure the extent of attenuation of the diabetes OR when all additional factors are accounted for.
All analyses were undertaken in R (version 3.6.2) (R Foundation for Statistical Computing, Vienna, Austria). Data are presented as mean ± standard deviation, unless stated otherwise.
Results
In the population examined, 862 individuals with T1DM with a mean ± standard deviation (SD) age of 39.4 ± 17.4 years had a confirmed positive Covid-19 test; 13,225 individuals with T2DM and a mean age of 63.1 ± 14.4 years were confirmed to have a positive Covid-19 test.
Hospital Admission Rates
As summarised in Table 1, for individuals with T1DM, the hospital admission rate in the first 28 days after a positive Covid-19 test was 10.0% vs 4.7% in matched controls [relative risk (RR) 2.1]. There was no difference in average or quintile of Townsend score and no difference in BMI between T1DM (27.2 SD ± 5.8) and matched controls (27.9 SD ± 6.2). There was a trend for length of stay (LOS) to be longer in individuals with T1DM. Mean HbA1c level for individuals with T1DM was 67.6 mmol/mol (SD ± 22.7) and for the matched controls it was 34.5 mmol/mol (SD ± 8.8). A significantly higher proportion of those with T1DM were taking aspirin, clopidogrel or an angiotensin-converting enzyme (ACE) inhibitor than matched controls.
As seen in Table 1 for individuals with T2DM, the hospital admission rate in the first 28 days after a positive Covid-19 test was 16.3% vs 11.6% in matched controls. The RR of admission was 1.4. LOS was longer in T2DM at 8.2 days vs 6.7 days in controls. There was a significant difference in Townsend score (1.8 ± 3.7 for T2DM vs 0.5 ± 3.7 for matched controls); a higher score equates to greater social disadvantage) with a higher proportion of people with T2DM in the top 2 quintiles of deprivation. BMI was higher in individuals with T2DM than in matched controls (31.7 ± 6.9 vs 28.6 ± 6.1). Mean HbA1c for individuals with T2DM was significantly higher than in matched controls (56.6 ± 21.0 vs 36.1 ± 9.1) with vitamin D level lower. There was a higher proportion of people with asthma or chronic obstructive pulmonary disease (COPD) in individuals with T2DM compared to controls. A significantly higher proportion of those with T2DM were taking aspirin, clopidogrel or ACE inhibitors than matched controls.
Kaplan–Meier curves were generated for hospital admission in individuals with T1DM (Fig. 1a) and individuals with T2DM (Fig. 1b) up to 15 months following a positive Covid-19 test. At 3 months there was a 7.1% higher admission rate post positive Covid-19 test for individuals with T1DM and 5.1% for individuals with T2DM, versus their respective controls.
Univariate Analysis
In the univariate analysis within the group of individuals with T1DM (Table 2), the likelihood of hospital admission was higher in people with a higher HbA1c and BMI, lower HDL-cholesterol and lower eGFR, in older individuals and in those with COPD or hypertension. Likelihood of hospital admission was also higher in those people taking and ACE inhibitor, aspirin or metformin and in those of African or mixed ethnicity compared to Caucasians.
A somewhat different profile was observed within the group of individuals with T2DM (Table 2) where the likelihood of hospital admission was higher in older individuals and in men, those with African heritage, in people with a more disadvantaged social situation as based on the Townsend Index and individuals with a history of enduring severe mental illness (SMI), hypertension, COPD or asthma. Admission was also higher in individuals with a lower eGFR and vitamin D, lower total and LDL-cholesterol and in those taking aspirin, an ACE inhibitor or clopidogrel. Hospital admission rate was lower in individuals with T2DM on metformin or South Asian ethnic origin compared to Caucasians.
Regarding androgen status, in men with T2DM a lower total testosterone level was not related to an increased likelihood of admission in the first 28 days after a positive Covid-19 test (OR 0.998, 95% CI 0.96–1.03). It was not possible to perform this analysis in individuals with T1DM because of the low numbers of men with a testosterone measurement.
Analyses of Combined Patients with T1DM and Controls and Combined Patients with T2DM and Controls
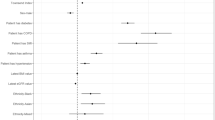
In Fig. 2 and Table 3, the change in OR indicates how much each factor changes the baseline OR for hospitalisation, thus indicating whether a factor may be related to more serious consequences of Covid-19 virus infection in people with diabetes.
In Covid-19-infected individuals with T1DM vs their controls, we found no factors significantly mediating likelihood of admission vs age-matched controls. Deviations from baseline were small and OR confidence intervals were large for the T1DM match cohort model because of much lower numbers than for the T2DM group.
In Covid-19-infected patients with T2DM, factors potentially related to a higher admission rate vs age-matched controls were Townsend index, ethnicity, BMI, hypertension, low eGFR, being on ACE inhibitor, aspirin, or clopidogrel with metformin lowering the risk.
Finally we combined the variables that had the biggest change in the OR compared to the base model (taking into account data standard deviations) in a multivariable risk model for combined patients with T1DM and controls (Table 4), factors to determine the factors independently associated with a higher likelihood of admission. These were having T1DM, age, social disadvantage (higher Townsend index), having diagnosed COPD and being of mixed ethnicity. The T1DM model accounted for 34% of the difference from the baseline model.
For combined patients with T2DM and controls (Table 4) factors relating to a higher likelihood of admission were having T2DM, age, male gender, BMI, diagnosed COPD, diagnosed hypertension, social deprivation (higher Townsend index) and non-white ethnicity (all groups). The T2DM model accounted for 49% of the difference from the baseline model.
Discussion
A previous diagnosis of diabetes mellitus is known to be a significant risk factor for increased Covid-19-related severity and worse outcomes, including higher hospital admission rates over time. In this prospective study we aimed to understand why this is the case using population-level data. We have extended our understanding of this observation by quantifying how much a diagnosis of diabetes increases the risk of hospital admission after a Covid-19 infection in Greater Manchester, UK. The RR of hospital admission vs matched controls was higher for individuals with T1DM than individuals with T2DM and comparable to that described by Barron et al. [4] for patients requiring hospital treatment for Covid-19 infection. Hospital admission rates remained higher after infection for up to 3 months (Fig. 1). This is one of the few analyses to report hospital admission rates for people with T1DM and Covid-19 infection.
Our analysis suggests a protective effect of metformin in people with T2DM. This is a novel finding in relation to the consequences of a Covid-19 infection, but is in keeping with a large body of evidence regarding the benefits of metformin in reducing the likelihood of severe consequences of T2DM [10]. The opposite association was seen in T1DM, likely because metformin is mostly given to people with T1DM who are overweight.
We found substantive overlap between the factors that put people at increased risk of admission with T2DM compared to the background population, such as hypertension or raised BMI. A very strong effect of ethnicity was seen in individuals with T2DM as previously described [5, 11, 12]. The multivariate model accounted for 49% of the variation in risk of admission from the base model. COPD and Townsend index also increased the risk of admission for individuals with T2DM. The association of lower total and LDL-cholesterol with an increased likelihood of hospital admission may relate to the application of more intensive statin dose titration in people with established cardiovascular disease, resulting in lower total and LDL-cholesterol levels in these individuals.
We have shown that for individuals with T1DM and those with T2DM, age, non-Caucasian ethnicity, eGFR, hypertension, a history of respiratory disorder and BMI and additionally in individuals with T2DM social disadvantage and SMI are factors that relate independently to a less favourable outcome in the 28 days following a Covid-19 infection, here manifesting as hospital admission. Furthermore being prescribed an ACE inhibitor or antiplatelet agent (associated with hypertension and diagnosed cardiovascular disease) was also associated with an increased likelihood of admission as was social disadvantage as measured by the Townsend index.
The underlying causes and processes that determine which individuals develop a severe clinical course requiring hospitalisation following Covid-19 infection will be complex and multifactorial. Some of these will determine how the innate and the acquired immune systems deal with the virus whereas other factors will clearly relate to how well an infected individual can regulate and maintain homeostasis following gross perturbations in the metabolic pathways and physiological processes. The likelihood is that in a proportion of individuals with diabetes the already existing consequences of associated pathologies and multi-comorbidity will in part explain why Covid-19 has such severe consequences.
It should be mentioned that the advent of treatment of hospitalised patients with dexamethasone, when patients are hospitalised with the pulmonary consequences of a Covid-19 infection, has significantly reduced mortality rates across the world [13]. Use of this drug continues to influence outcomes positively as new virus variants have emerged. Additional agents are also now available for Covid-19-affected patients who become severely unwell [14].
Within our analysis to determine what may differentiate individuals with diabetes and from those without diabetes regarding likelihood of admission, a lower eGFR and higher average blood glucose (as reflected by HbA1c) are shown to be potential differentiating factors. Both have been previously linked to an impaired cell-mediated immune response [15], which is critical for effective acquired immunity to a Covid-19 infection.
It has been reported that within T2DM both a diagnosis of COPD [16] and non-white ethnicity [17] resulted in a higher likelihood of hospital admission. Previously we reported that being older was the major risk factor for death in people with T2DM, as also observed in the general population [18].
Vitamin D level may be a differentiating factor linked to a more adverse outcome for people with T2DM, is important and is further evidence for the influence of vitamin D levels on Covid-19 outcome [19, 20], although this remains an area of much debate.
As we go forward in the ‘post pandemic’ world, where new variants of the Covid-19 may arise, any evidence concerning factors that confer greater risk of hospitalisation in people with T1DM and T2DM will be helpful. This can be seen in the context that potential pathogenic links between the Covid-19 and diabetes mellitus include the influence of glucose homeostasis and potentially altered immune status on the progression of the SARS-CoV-2 viral infection once established [21].
Much remains to be determined about why having diabetes increases the risk of likelihood of serious consequences of a Covid-19 infection. Parveen et al. [22] reported that both a diagnosis of diabetes and of hypertension had a negative effect on the health status of patients with Covid-19 and pointed out that large prevalence studies were required. There were similar conclusions from Abdi et al. [23], as supported by our findings.
We report that the presence of COPD/asthma in association with a diagnosis of T2DM increased the likelihood of admission as previously described [24, 25], but also that a diagnosis of SMI was associated with an increased likelihood of admission. This accords with previous findings reported by Lee et al. in a Korean study [26] and may relate to many people with SMI being in relatively poor health and being in a more disadvantaged sociodemographic situation.
Our findings indicate that being on clopidogrel, aspirin or an ACE inhibitor is related to an increased risk of hospital admission within patients with diabetes. This is likely to relate to these agents only being given to people with hypertension, proteinuria and/or a history of vascular disease. Nevertheless we found that much of the elevated likelihood of admission in individuals with diabetes cannot be accounted for by risk factors that have been measured in the course of routine care.
Dexamethasone for the treatment of an acute Covid-19 infection can increase blood glucose levels [13] particularly in people with diabetes. Therefore, frequent blood glucose monitoring and personalized adjustment of medications are required [27], with addition of glucose-lowering therapy sometimes being necessary.
Much less has been published about outcomes in T1DM following Covid-19 infection. Ebekozien et al. [28] described the most common presenting symptoms and outcomes for 64 people with T1DM who have confirmed or suspected Covid-19. More than 50% of all cases reported hyperglycemia, and nearly one-third of patients experienced diabetic ketoacidosis.
We suggest that while individuals with particular conditions have a higher risk for admission or dying following a Covid-19 infection, this might be explained by there being a composite/multifactorial measure of immunological/metabolic resilience and reserve capacity for dealing with acute inflammation and infection. Resilience vs vulnerability would likely exist on a continuum and be largely influenced by such key factors as age, body mass index, respiratory health/capacity, underlying immunodeficiency/autoimmunity status, renal function, cardiovascular health and current/latent infections.
In the same way that we have developed a ‘frailty score’ we do not have a Covid-19 infection resilience score in people with diabetes. Such an approach would provide a cornerstone for planning any future prevention strategies.
Strengths/Limitations
A limitation common to all Covid-19 research is that during the first few months of the pandemic there was limited capacity to test for Covid-19 infection, and so the true prevalence is unknown and can only be estimated. Thus there is the likelihood of there being an underestimate of the total number of positive Covid-19 test results. However there is no reason to suspect that this would affect individuals with diabetes vs those without diabetes differentially. A strength is that by matching our cohort on the date of positive coronavirus test, as well as age and sex, we are able to correct for this and focus on the differences between the diabetes cohort and the general population.
A further limitation is that the data only covers Greater Manchester and we have relied on general practice record coded diagnoses.
Conclusion
In a UK population we have confirmed a significantly higher likelihood of admission in people with diabetes following a Covid-19 infection. A number of factors including BMI, blood pressure, socioeconomic situation and ethnicity have been identified as possibly mediating that increased likelihood of hospital admission. For T2DM, the majority of factors related to increased risk of admission are common to the general population but more prevalent in T2DM. Metformin was protective.
References
WHO. https://www.who.int/health-topics/coronavirus. Accessed 24 Aug 2021.
Tadic M, Cuspidi C, Sala C. COVID-19 and diabetes: is there enough evidence? J Clin Hypertens (Greenwich). 2020;22:943–8.
Katulanda P, Dissanayake HA, Ranathunga I, et al. Prevention and management of COVID-19 among patients with diabetes: an appraisal of the literature. Diabetologia. 2020;63:1440–52.
Barron E, Bakhai C, Kar P, et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol. 2020;8:813–22.
Hippisley-Cox J, Coupland CA, Mehta N, et al. Risk prediction of covid-19 related death and hospital admission in adults after covid-19 vaccination: national prospective cohort study. BMJ. 2021;374:n2244.
Cariou B, Hadjadj S, Wargny M, et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia. 2020; 63:1500–1515.
Health Innovation Manchester. https://healthinnovationmanchester.com/thegmcarerecord/the-gm-care-record-for-secondary-uses-research. Accessed 21 May 2021.
Health Innovation Manchester. https://healthinnovationmanchester.com. Accessed 21 May 2021.
Dolan SA, Jarman B, Bajekal M, Davies PM, Hart D. Measuring disadvantage: changes in the underprivileged area, Townsend, and Carstairs scores 1981–91. J Epidemiol Community Health. 1995;49(Suppl 2):S30–3.
Scheen AJ. Metformin and COVID-19: from cellular mechanisms to reduced mortality. Diabetes Metab. 2020;46:423–6.
Clift AK, Coupland CAC, Keogh RH, et al. Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study. BMJ. 2020;371:m3731.
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. https://doi.org/10.1001/jama.2020.6775. (Erratum in JAMA 2020;323:2098).
RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384(8):693–704. https://doi.org/10.1056/NEJMoa2021436.
Izda V, Jeffries MA, Sawalha AH. COVID-19: a review of therapeutic strategies and vaccine candidates. Clin Immunol. 2021;222:108634.
Paces J, Strizova Z, Smrz D, Cerny J. COVID-19 and the immune system. Physiol Res. 2020; 69:379–388.
Nandy K, Salunke A, Pathak SK, et al. Coronavirus disease (COVID-19): a systematic review and meta-analysis to evaluate the impact of various comorbidities on serious events. Diabetes Metab Syndr. 2020;14(5):1017–1025.
Learoyd AE, Douiri A, Hart N. COVID-19 and ethnicity: has history repeated itself? Thorax. 2021;76:537–8.
Tian Z, Heald AH, Stedman M, et al. Age of people with type 2 diabetes and the risk of dying following SARS-CoV-2 infection. Int J Clin Pract. 2021;75:e14053.
Bilezikian JP, Bikle D, Hewison M, et al. Mechanisms in endocrinology: vitamin D and COVID-19. Eur J Endocrinol. 2020;183:R133–47.
Mercola J, Grant WB, Wagner CL. Evidence regarding vitamin D and risk of COVID-19 and its severity. Nutrients. 2020;12:3361.
Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17:11–30.
Parveen R, Sehar N, Bajpai R, Agarwal NB. Association of diabetes and hypertension with disease severity in covid-19 patients: a systematic literature review and exploratory meta-analysis. Diabetes Res Clin Pract. 2020;166:108295.
Abdi A, Jalilian M, Sarbarzeh PA, Vlaisavljevic Z. Diabetes and COVID-19: a systematic review on the current evidences. Diabetes Res Clin Pract. 2020;166:108347.
Leung JM, Niikura M, Yang CWT, Sin DD. COVID-19 and COPD. Eur Respir J. 2020;56:2002108.
Schultze A, Walker AJ, MacKenna B, et al. Risk of COVID-19-related death among patients with chronic obstructive pulmonary disease or asthma prescribed inhaled corticosteroids: an observational cohort study using the OpenSAFELY platform. Lancet Respir Med. 2020;8:1106–1120.
Lee SW, Yang JM, Moon SY, et al. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry. 2020;7:1025–31.
Zhang F, Karam JG. Glycemic profile of intravenous dexamethasone-induced hyperglycemia using continuous glucose monitoring. Am J Case Rep. 2021;22:e930733.
Ebekozien OA, Noor N, Gallagher MP, Alonso GT. Type 1 diabetes and COVID-19: preliminary findings from a multicenter surveillance study in the U.S. Diabetes Care. 2020;43;e83–e85.
Acknowledgements
The time of DJ, RW and NP was funded by the National Institute for Health Research (NIHR) Greater Manchester Patient Safety Translational Research Centre. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The datasets generated during and analyzed during the current study are not publicly available as all data access is subject to review by Health Innovation Manchester.
Funding
There was no external funding for this study. There was no external funding for this study. The journal’s Rapid service Fee was funded by the corresponding author.
Compliance with Ethics Guidelines
Data were de-identified at source and were extracted from the Greater Manchester Care Record (GMCR) database [7]. The follow-up period started on 1 January 2020 and ended on 31 May 2021. The GMCR pools information all general practices across the conurbation. The project was approved and overseen by Health Innovation Manchester [8], which is comparable to an ethics committee in relation to the management and supervision of access to the population health records of citizens of Greater Manchester for research purposes. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. This study was conducted in accordance with ethical guidelines.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Adrian H Heald: Conception of the project and drafting the manuscript. Contributions were as follows: David A Jenkins: Data handling, statistical analysis and drafting the manuscript. Richard Williams: Data curation and drafting the manuscript. Matthew Sperrin: Statistical analysis and drafting the manuscript. Helene Fachim: Conceptualisation and drafting the manuscript. Rajshekhar N Mudaliar: Expert input and reviewing the manuscript. Akheel Syed: Expert input and reviewing the manuscript. Asma Naseem: Expert input and reviewing the manuscript. J Martin Gibson: Conceptualisation, expert input and drafting the manuscript. Kelly A Bowden Davies: Conceptualisation and drafting the manuscript. Niels Peek: Expert input and reviewing the manuscript. Simon G Anderson: Conceptualisation, statistical analysis and drafting the manuscript. Yonghong Peng: Conceptualisation, expert input and reviewing the manuscript. William Ollier: Conceptualisation and reviewing the manuscript.
Disclosures
None of the co-authors has any conflict of interest. Specifically Adrian H Heald, David A Jenkins, Richard Williams, Matthew Sperrin, Helene Fachim, Rajshekhar N Mudaliar, Akheel Syed, Asma Naseem, J Martin Gibson, Kelly A Bowden Davies, Niels Peek, Simon G Anderson, Yonghong Peng, William Ollier have no disclosures to make.
Data Availability
The datasets generated during and analyzed during the current study are not publicly available as all data access is subject to review by Health Innovation Manchester.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Heald, A.H., Jenkins, D.A., Williams, R. et al. The Risk Factors Potentially Influencing Hospital Admission in People with Diabetes, Following SARS-CoV-2 Infection: A Population-Level Analysis. Diabetes Ther 13, 1007–1021 (2022). https://doi.org/10.1007/s13300-022-01230-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01230-2