Abstract
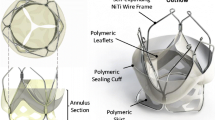
A growing number of elderly patients with significant co-morbidities do not meet the inclusion criteria for conventional cardiac surgical therapies, including aortic valve replacement and mechanical circulatory support. To meet this clinical need, an aortic valve bypass (AVB) system is being developed that may be implanted using subcostal or mini-thoracotomy surgical approaches without ventricular coring or cardiopulmonary bypass. The AVB system consists of an apical left ventricular (ALV) cannula made from pyrolytic carbon, a valved conduit with a locking mechanism, and a Nitinol clip for anastomosis to the descending aorta. To define design criteria and demonstrate efficacy, ALV cannulae with different diameters (7–14 mm), number of sideholes (6–12), sidehole size (1.9–4.6 mm wide) and tip shapes (tapered, straight) were designed, fabricated, and tested. Cannula efficacy was determined by quantifying flow rates and pressure drops across the ALV cannula using steady-state and dynamic mock circulation models simulating mild, moderate and severe aortic stenosis test conditions. Blood trauma testing was conducted to demonstrate hemocompatibility using the smallest diameter (7 mm) ALV cannula prototype fabricated from pyrolytic carbon (PYC). In vitro and blood trauma testing demonstrated that (1) the 7 mm PYC cannula did not produce significant hemolysis (<40 mg/dL pfHb), but was unable to achieve bypass flow rates above 1.4 L/min, (2) a minimum cannula diameter of 12 mm was required to produce flow rates >4.5 L/min for <10 mmHg pressure drop across the ALV cannula, and (3) the cannula tip shape did not significantly alter bypass flow rate or pressure drop. The ALV cannula may enable a minimally invasive surgical approach using a modified Seldinger’s technique for implantation in heart failure patients with aortic stenosis.







Similar content being viewed by others
References
Adams, C., L. R. Guo, P. M. Jones, C. Harle, J. W. Brown, J. S. Gammie, et al. Automated coring and apical connector insertion device for aortic valve bypass surgery. Ann. Thorac. Surg. 93(1):290–293, 2012.
Ambler, G., R. Z. Omar, P. Royston, R. Kinsman, B. E. Keogh, and K. M. Taylor. Generic, simple risk stratification model for heart valve surgery. Circulation 112(2):224–231, 2005.
ASTM F1841-97. Standard practice for assessment of hemolysis in continuous flow blood pumps, 2005.
ASTM F1830-97. Standard practice of for selection of blood for in vitro evaluation of blood pumps, 2005.
Bachman, T. N., J. K. Bhama, J. Verkaik, S. Vandenberghe, R. L. Kormos, and J. F. Antaki. In-vitro evaluation of ventricular cannulation for rotodynamic cardiac assist devices. Cardiovasc. Eng. Technol. 2(3):203–211, 2011.
Balaras, E., K. S. Cha, B. P. Griffith, and J. S. Gammie. Treatment of aortic stenosis with aortic valve bypass (apicoaortic conduit) surgery: an assessment using computational modeling. J. Thorac. Cardiovasc. Surg. 137(3):680–687, 2009.
Bonow, R. O., B. A. Carabello, K. Chatterjee, A. C. De Leon, Jr., D. P. Faxon, M. D. Freed, et al. Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 118(15):e523–e661, 2008.
Borow, M., and J. G. Crowley. Evaluation of central venous catheter thrombogenicity. Acta Anaesthesiol. Scand. Suppl. 81:59–64, 1985.
Crestanello, J. A., K. J. Zehr, R. C. Daly, T. A. Orszulak, and H. V. Schaff. Is there a role for the left ventricle apical-aortic conduit for acquired aortic stenosis? J. Heart Valve Dis. 13(1):57–62, 2004; (discussion 62–63).
Gammie, J. S., J. W. Brown, J. M. Brown, R. S. Poston, R. N. Pierson, 3rd, P. N. Odonkor, et al. Aortic valve bypass for the high-risk patient with aortic stenosis. Ann. Thorac. Surg. 81(5):1605–1610, 2006.
Gammie, J. S., L. S. Krowsoski, J. M. Brown, P. N. Odonkor, C. A. Young, M. J. Santos, et al. Aortic valve bypass surgery: midterm clinical outcomes in a high-risk aortic stenosis population. Circulation 118(14):1460–1466, 2008.
Giridharan, G. A., M. A. Sobieski, M. Ising, M. S. Slaughter, and S. C. Koenig. Blood trauma testing for mechanical circulatory support devices. Biomed. Instrum. Technol. 45(4):334–339, 2011.
Goodman, S. L., K. S. Tweden, and R. M. Albrecht. Platelet interaction with pyrolytic carbon heart-valve leaflets. J. Biomed. Mater. Res. 32(2):249–258, 1996.
Grigioni, M., C. Daniele, U. Morbiducci, G. D’Avenio, G. Di Benedetto, C. Del Gaudio, et al. Computational model of the fluid dynamics of a cannula inserted in a vessel: incidence of the presence of side holes in blood flow. J. Biomech. 35(12):1599–1612, 2002.
Kameneva, M. V., G. W. Burgreen, K. Kono, B. Repko, J. F. Antaki, and M. Umezu. Effects of turbulent stresses upon mechanical hemolysis: experimental and computational analysis. ASAIO J. 50(5):418–423, 2004.
Kirklin, J. K., D. C. Naftel, R. L. Kormos, L. W. Stevenson, F. D. Pagani, M. A. Miller, et al. Second INTERMACS annual report: more than 1,000 primary left ventricular assist device implants. J. Heart Lung Transplant. 29(1):1–10, 2010.
Koenig, S. C., G. M. Pantalos, K. J. Gillars, D. L. Ewert, K. N. Litwak, and S. W. Etoch. Hemodynamic and pressure-volume responses to continuous and pulsatile ventricular assist in an adult mock circulation. ASAIO J. 50(1):15–24, 2004.
Koenig, S. C., C. Woolard, G. Drew, L. Unger, K. Gillars, D. Ewert, et al. Integrated data acquisition system for medical device testing and physiology research in compliance with good laboratory practices. Biomed. Instrum. Technol. 38(3):229–240, 2004.
Leverett, L. B., J. D. Hellums, C. P. Alfrey, and E. C. Lynch. Red blood cell damage by shear stress. Biophys. J. 12(3):257–273, 1972.
Medtronic. Hancock Specialty Products, 2012. www.medtronic.com/for-healthcare-professionals/products-therapies/cardiovascular/heart-valves-surgical/hancock-specialty-products. Accessed 2 July 2012.
Mihaljevic, T., Y. Ootaki, J. O. Robertson, A. K. Durrani, K. Kamohara, M. Akiyama, et al. Beating heart cardioscopy: a platform for real-time, intracardiac imaging. Ann. Thorac. Surg. 85(3):1061–1065, 2008.
Milano, C. A., A. A. Simeone, L. J. Blue, and J. G. Rogers. Presentation and management of left ventricular assist device inflow cannula malposition. J. Heart Lung Transplant. 30(7):838–840, 2011.
Olcott, E. L. Pyrolytic biocarbon materials. J. Biomed. Mater. Res. 8(3):209–217, 1974.
Padala, M., J. H. Jimenez, A. P. Yoganathan, A. Chin, and V. H. Thourani. Transapical beating heart cardioscopy technique for off-pump visualization of heart valves. J. Thorac. Cardiovasc. Surg. 144(1):231–234, 2012.
Parsa, C. J., C. A. Milano, A. D. Proia, G. B. Mackensen, and G. C. Hughes. A previously unreported complication of apicoaortic conduit for severe aortic stenosis. Ann. Thorac. Surg. 87(3):927–928, 2009.
Paul, R., J. Apel, S. Klaus, F. Schugner, P. Schwindke, and H. Reul. Shear stress related blood damage in laminar couette flow. Artif. Organs 27(6):517–529, 2003.
Rhodes, N. P., T. V. Kumary, and D. F. Williams. Influence of wall shear rate on parameters of blood compatibility of intravascular catheters. Biomaterials 17(20):1995–2002, 1996.
Richenbacher, W. E., and J. D. Marks. Cannula selection and cannulation techniques for nonpulsatile mechanical ventricular assistance. Artif. Organs 19(6):519–524, 1995.
Schroeder, M. J., B. Perreault, D. L. Ewert, and S. C. Koenig. HEART: an automated beat-to-beat cardiovascular analysis package using Matlab. Comput. Biol. Med. 34(5):371–388, 2004.
Seldinger, S. I. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol. 39(5):368–376, 1953.
Selzman, C. H., and B. C. Sheridan. Off-pump insertion of continuous flow left ventricular assist devices. J. Card. Surg. 22(4):320–322, 2007.
Slaughter, M. S., B. Pederson, J. D. Graham, M. A. Sobieski, and S. C. Koenig. Evaluation of new Forcefield technology: reducing platelet adhesion and cell coverage of pyrolytic carbon surfaces. J. Thorac. Cardiovasc. Surg. 142(4):921–925, 2011.
Stauffer, C. E., J. Jeudy, M. Ghoreishi, C. Vliek, C. Young, B. Griffith, et al. Magnetic resonance investigation of blood flow after aortic valve bypass (apicoaortic conduit). Ann. Thorac. Surg. 92(4):1332–1337, 2011; (discussion 7–8).
Sutera, S. P., and M. H. Mehrjardi. Deformation and fragmentation of human red blood cells in turbulent shear flow. Biophys. J. 15(1):1–10, 1975.
Thourani, V. H., W. B. Keeling, R. A. Guyton, A. Dara, S. D. Hurst, and O. M. Lattouf. Outcomes of off-pump aortic valve bypass surgery for the relief of aortic stenosis in adults. Ann. Thorac. Surg. 91(1):131–136, 2011.
Tuzun, E., K. Roberts, W. E. Cohn, M. Sargin, C. J. Gemmato, B. Radovancevic, et al. In vivo evaluation of the HeartWare centrifugal ventricular assist device. Tex. Heart Inst. J. 34(4):406–411, 2007.
Vassiliades, Jr., T. A. Off-pump apicoaortic conduit insertion for high-risk patients with aortic stenosis. Eur. J. Cardiothorac. Surg. 23(2):156–158, 2003.
Vliek, C. J., E. Balaras, S. Li, J. Y. Lin, C. A. Young, C. R. DeFilippi, et al. Early and midterm hemodynamics after aortic valve bypass (apicoaortic conduit) surgery. Ann. Thorac. Surg. 90(1):136–143, 2010.
Yamada, Y., T. Nishinaka, T. Mizuno, Y. Taenaka, E. Tatsumi, and K. Yamazaki. Neointima-inducing inflow cannula with titanium mesh for left ventricular assist device. J. Artif. Organs 14(4):269–275, 2011.
Yeo, K. K., and R. I. Low. Aortic stenosis: assessment of the patient at risk. J. Interv. Cardiol. 20(6):509–516, 2007.
Acknowledgments
This work was supported by the Roger M. Prizant Research Trust Fund for ventricular assist device-related research at the University of Louisville.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Keefe B. Manning oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Soucy, K.G., Graham, J.D., Benzinger, C.J. et al. Apical-Ventricular Cannula for Aortic Valve Bypass Therapy. Cardiovasc Eng Tech 4, 161–170 (2013). https://doi.org/10.1007/s13239-013-0144-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-013-0144-8