Abstract
Objective
To determine critical factors and barriers to postpartum intrauterine contraceptive device (PPIUCD) use in India in order to guide programs aimed at reducing maternal and child mortality.
Methods
All pregnant women were enrolled for contraception counseling during their visit to the antenatal outpatient clinic. Women who opted for PPIUCDs were enrolled in the study and offered PPIUCD insertion, irrespective of mode of delivery. Those who withdrew consent when in labor or soon after delivery, experienced severe bleeding, or exhibited unstable vital signs were excluded, as were febrile women and those diagnosed with chorioamnionitis.
Results
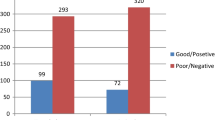
A total of 66,508 women were enrolled in the study. 86.1% indicated they discussed family planning options with their partners/husbands before making a decision. 178 respondents (0.3%) could not mention one advantage of PPIUCDs, while 23.1% could not mention one disadvantage. 13.9% of the women withdrew consent. Family member objections (43.44%), husband/partner objection (27.94%), and deciding on another method (15.59%) were the main reasons for consent withdrawal.
Conclusions
Awareness of PPIUCDs is not a limiting factor in women’s consent to PPIUCD insertion. As a woman’s decision to use a PPIUCD is significantly influenced by family members and her partner/husband, awareness initiatives that target these populations should be considered.
Similar content being viewed by others
References
Yazdkhasti M, Pourreza A, Pirak A, et al. Unintended pregnancy and its adverse social and economic consequences on health system: a narrative review article. Iran J Public Health. 2015;44(1):12–21.
Le HH, Connolly MP, Bahamondes L, et al. The burden of unintended pregnancies in Brazil: a social and public health system cost analysis. Int J Women’s Health. 2014;6:663–70. https://doi.org/10.2147/IJWH.S61543.
Wado YD, Afework MF, Hindin MJ, et al. Unintended pregnancies and the use of maternal health services in south western Ethiopia. BMC Int Health Hum Rights. 2013;13:36.
Firdous N, Qureshi A, Manzoor R, et al. Impact of interpregnacy interval on perinatal outcome. JK Pract. 2014;19(3/4):75–9.
Haq A, Lallar M, Akhter S, et al. Interpregnancy interval raise odds of adverse perinatal outcome in high fertility region Mewat, Haryana. Int J Reprod Contracept Obstet Gynecol. 2014;3:598–603. https://doi.org/10.5455/2320-1770.ijrcog20140934.
de Jonge HC, Azad K, Seward N, et al. Determinants and consequences of short birth interval in rural Bangladesh: a cross-sectional study. BMC Pregnancy Childbirth. 2014;14:427. https://doi.org/10.1186/s12884-014-0427-6.
Chen I, Jhangri GS, Lacasse M, et al. Relationship between interpregnancy interval and adverse perinatal and neonatal outcomes in Northern Alberta. J Obstet Gynaecol Canada. 2015;37(7):598–605. https://doi.org/10.1016/S1701-2163(15)30197-3.
Trussell J, Henry N, Hassan F, et al. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154–61.
Lassi ZS, Mansoor T, Salam RA, et al. Essential pre-pregnancy and pregnancy interventions for improved maternal, newborn and child health. Reprod Health. 2014;11(Suppl 1):S1.
Ball SJ, Pereira G, Jacoby P, et al. Re-evaluation of link between interpregnancy interval and adverse birth outcomes: retrospective cohort study matching two intervals per mother. BMJ. 2014;349:g4333. https://doi.org/10.1136/bmj.g4333.
Smits LJM, Elzenga HM, Gemke RJ, et al. The association between interpregnancy interval and birth weight: What is the role of maternal polyunsaturated fatty acid status? BMC Pregnancy Childbirth. 2013;13:23.
Government of India. Postpartum IUCD Reference manual. 2010 (last updated reference manual).
Kumar S, Sethi R, Balasubramaniam S, et al. Women’s experience with postpartum intrauterine contraceptive device use in India. Reprod Health. 2014;11:32. https://doi.org/10.1186/1742-4755-11-32.
Jayanthi TP, Abishek B. Birth spacing: women’s knowledge, methods adopted and barriers. Natl J Res Community Med. 2017;6(2):187–94.
Singh A, Meena P, Radhakrishnan G, et al. A knowledge, attitude and practice study on awareness and acceptance of contraception in postpartum women in a tertiary care hospital. Int J Reprod Contracept Obstet Gynecol. 2016;5:1921–4.
Ganatra B, Faundes A. Role of birth spacing, family planning services, safe abortion services and post-abortion care in reducing maternal mortality. Best Pract Res Clin Obstet Gynaecol. 2016;36:145–55. https://doi.org/10.1016/j.bpobgyn.2016.07.008.
Dixit P, Dwivedi LK, Gupta A. Role of maternal and child health care services on postpartum contraceptive adoption in India. Sage Open: Thousand Oaks; 2017.
Achyut P, Mishra A, Montana L, et al. Integration of family planning with maternal health services: an opportunity to increase postpartum modern contraceptive use in urban Uttar Pradesh, India. J Fam Plan Reprod Health Care. 2016;42(2):107–15. https://doi.org/10.1136/jfprhc-2015-101271.
Teka TT, Feyissa TR, Melka AS, et al. Role of antenatal and postnatal care in contraceptive use during postpartum period in western Ethiopia: a cross sectional study. BMC Res Notes. 2018;11(1):581. https://doi.org/10.1186/s13104-018-3698-6.
Kumari SS. Permanent sterilisation to long-acting reversible contraception: Is a paradigm shift necessary? J Obstet Gynaecol India. 2016;66(3):149–53. https://doi.org/10.1007/s13224-016-0866-2.
Bhushan H, Bhardwaj A. Task shifting: a key strategy in the multipronged approach to reduce maternal mortality in India. Int J Gynecol Obstet. 2015;131:S67–70. https://doi.org/10.1016/j.ijgo.2015.03.016.
Ministry of Health and Family Welfare, Government of India. National Family Health Survey (2015–2016). http://rchiips.org/nfhs/pdf/NFHS4/India.pdf. Accessed Mar 2019.
Garg S, Singh R. Need for integration of gender equity in family planning services. Indian J Med Res. 2014;140(Suppl 1):S147–51.
Pachauri S. Priority strategies for India’s family planning programme. Indian J Med Res. 2014;140(Suppl 1):S137–46.
Mishra A, Nanda P, Speizer IS, et al. Men’s attitudes on gender equality and their contraceptive use in Uttar Pradesh, India. Reprod Health. 2014;11:41. https://doi.org/10.1186/1742-4755-11-41.
Sedgh G, Hussain R. Reasons for contraceptive nonuse among women having unmet need for contraception in developing countries. Stud Fam Plan. 2014;45(2):151–69.
Sambath S, Balasubramanian T, Ilangovan S, et al. Awareness of contraception and the reasons for having more than two children: a survey among antenatal women. Int J Reprod Contracept Obstet Gynecol. 2016;5(4):959–61. https://doi.org/10.18203/2320-1770.ijrcog20160840.
Thummalachetty N, Mathur S, Mullinax M, et al. Contraceptive knowledge, perceptions, and concerns among men in Uganda. BMC Public Health. 2017;17(1):792. https://doi.org/10.1186/s12889-017-4815-5.
FIGO PPIUCD Project, July–September 2015. https://us12.campaign-archive.com/?u=d060766a782b60c73971a6d7d&id=b264e5025e&e=febe718f69. Accessed Mar 2019.
Acknowledgements
We would like to thank the Government of India, Ministry of Health and Family Welfare (Ms Vandana Gurnani, Joint Secretary, Dr Sikdar Commissioner Family Planning), FOGSI team (All Presidents, Vice Presidents, General Secretaries, Deputy Secretaries, Treasurers, Joint Treasurers, Joint Secretaries and Staff), Center Teams (Chief Coordinators, Deputy Coordinators, Nursing Staff, Advisors, Nodal Officers and Counsellors), and Avni Health Foundation team members who have all contributed to the successful program implementation. Additionally, the team thanks all the FIGO PPIUCD team members including Prof S Arulkumaran and Dr A Makins for the technical support, funding, and the ongoing partnership for the PPIUCD program implementation.
Funding
Anonymous Donors funded the program through FIGO.
Author information
Authors and Affiliations
Contributions
HD and AB were responsible for hypothesis formulation, data analysis, and initial drafting of the manuscript. AB, TS, and PS contributed to the development, implementation, and management of the training program described. CNP contributed to the development, partnerships with the government, administrative support for program implementation, and reviewing the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
PPIUCD program is implemented as per the approved guidelines “IUCD reference manual for medical officers and nursing personnel”—September 2013 issued by Government of India—Family Planning Division, Ministry of Health and Family Welfare (GOI).
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
Each and every subject was informed about the PPIUCD program, and consent was taken.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dr. Hema Divakar is a Director of Divakar’s Specialty Hospital, Bengaluru, India. Ajey Bhardwaj is a Director of Avni Health Foundation. Chittaranjan Narhari Purandare is President FIGO during 2016–2018—The International Federation of Gynecology and Obstetrics (FIGO), Emeritus Dean—Indian College of Obstetricians and Gynaecologists and Consultant OBGYN—Purandare Hospital. Thelma Sequeira is a Project Director of Avni Health Foundation. Pooja Sanghvi is a Program Officer of Avni Health Foundation.
Rights and permissions
About this article
Cite this article
Divakar, H., Bhardwaj, A., Purandare, C.N. et al. Critical Factors Influencing the Acceptability of Post-placental Insertion of Intrauterine Contraceptive Device: A Study in Six Public/Private Institutes in India. J Obstet Gynecol India 69, 344–349 (2019). https://doi.org/10.1007/s13224-019-01221-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-019-01221-7