Abstract
Introduction
Opioid abuse and opioid overdose deaths have increased significantly over the past decade. Naloxone is a potentially life-saving medication that can reverse opioid-induced respiratory depression, though precipitated opioid withdrawal can pose acute risks to the patient and medical personnel. The optimal naloxone dose is unclear and few studies address this question.
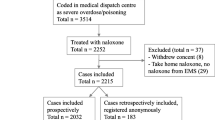
Methods
A convenience sample of commonly available references were queried for the recommended IV naloxone dose. When dosing recommendations were different for opioid-tolerant patients these were also recorded.
Results
Twenty-five references were located. 48% recommended a starting dose ≤ 0.05 mg while 36% recommend a dose ten-fold higher. More than half of medical toxicology and general medical sources recommended a low-dose strategy with a starting dose lower than 0.05 mg IV.
Conclusion
There are variations in the recommended doses for naloxone with ranges spanning an order of magnitude. Further exploration is needed to determine the dose that balances reversal of respiratory depression with mitigation of withdrawal.

Similar content being viewed by others
References
Volkow N. America’s addiction to opioids: heroin and prescription drug abuse. National Institute on Drug Abuse. 2014. http://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2014/americas-addiction-to-opioids-heroin-prescription-drug-abuse-_ftn4. Accessed 27 January 2015
Warner M, Hedegaard H, Chen L. Trends in drug-poisoning deaths involving opioid analgesics and heroin: United States, 1999–2012. In: Health E-Stat. Centers for Disease Control and Prevention’s National Vital Statistics System. 2014. http://www.cdc.gov/nchs/data/hestat/drug_poisoning/drug_poisoning.htm. Accessed 27 January 2015
Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR morbidity and mortality weekly report. 2016;64(50–51):1378–82. doi:10.15585/mmwr.mm6450a3
Rudd RA, Paulozzi LJ, Bauer MJ, Burleson RW, Carlson RE, Dao D, et al. Increases in heroin overdose deaths—28 States, 2010 to 2012. MMWR Morb Mortal Wkly Rep. 2014;63(39):849–54.
Hedegaard H, Chen LH, Warner M. Drug-poisoning deaths involving heroin: United States, 2000–2013. NCHS data brief. 2015(190):1–8
Hoffman JR, Schriger DL, Luo JS. The empiric use of naloxone in patients with altered mental status: a reappraisal. Ann Emerg Med. 1991;20(3):246–52.
Mills CA, Flacke JW, Miller JD, Davis LJ, Bloor BC, Flacke WE. Cardiovascular effects of fentanyl reversal by naloxone at varying arterial carbon dioxide tensions in dogs. Anesth Analg. 1988;67(8):730–6.
Kienbaum P, Thurauf N, Michel MC, Scherbaum N, Gastpar M, Peters J. Profound increase in epinephrine concentration in plasma and cardiovascular stimulation after mu-opioid receptor blockade in opioid-addicted patients during barbiturate-induced anesthesia for acute detoxification. Anesthesiology. 1998;88(5):1154–61.
Johnson C, Mayer P, Grosz D. Pulmonary edema following naloxone administration in a healthy orthopedic patient. J Clin Anesth. 1995;7(4):356–7.
Belz D, Lieb J, Rea T, Eisenberg MS. Naloxone use in a tiered-response emergency medical services system. Prehospital Emergency Care: Official Journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2006;10(4):468–71. doi:10.1080/10903120600885134
Buajordet I, Naess AC, Jacobsen D, Brors O. Adverse events after naloxone treatment of episodes of suspected acute opioid overdose. Eur J Emer Med: Off J Eur Soc Emerg Med. 2004;11(1):19–23.
Yip L, Megarbane B, Borron S. Opioids. In: Shannon M, Borron S, Burns M, editors. Haddad and Winchester’s clinical management of poisoning and drug overdose. Philadelphia: Saunders/Elsevier; 2007. p. 635–58.
Wong J. Naloxone and nalmefen. In: Olson K, editor. Poisoning & drug overdose. New York: McGraw-Hill; 2012.
Lewin N, Howland M. Antidotes in depth: opioid antagonists. In: Nelson L, Howland M, Hoffman R, Goldfrank L, Flomenbaum N, editors. Goldfrank’s toxicologic emergencies. New York: McGraw-Hill; 2011.
Stolbach A, Hoffman R. Opioid intoxication in adults. In: UpToDate, Traub S (Ed), UpToDate, Waltham, MA. Accessed 13 January 2016; 2013
Naloxone. In: Lexicomp online database [database on the Internet]. Lexicomp Inc., Hudson (OH). Accessed 30 November 2015
Vanden Hoek TL, Morrison LJ, Shuster M, Donnino M, Sinz E, Lavonas EJ, et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S829–61. doi:10.1161/circulationaha.110.971069.
Doyon S. Opioids. In: Tinitinalli J, Stapczynski J, Ma O, Cline D, Cydulka R, Meckler G, editors. Tintinalli’s emergency medicine: a comprehensive study guide. New York: McGraw-Hill; 2011.
Bardsley C. Opioids. In: Marx J, Hockberger R, Walls R, al. e, editors. Rosen’s emergency medicine: concepts and clinical practice. Philadelphia: Mosby Elsevier; 2014. p. 2055.
Naloxone. In: Butterworth JF, Mackey DC, Wasnick JD, Morgan GE, Mikhail MS, Morgan GE, editors. Morgan & Mikhail’s clinical anesthesiology. New York: McGraw-Hill; 2013.
Hoffmann C, Tourtier J. Antidotes. In: Atchabahian A, Gupta R, editors. The anesthesia guide. New York: McGraw-Hill; 2013.
Opioids. In: Wiki Tox open source clinical toxicology curriculum 2006. Accessed 30 November 2015
Lee C, Tschudy M, Arcara K. Drug doses. In: Tschudy M, Arcara K, editors. The Harriet lane handbook. Philadelphia: Mosby; 2011.
Stephens E. Emedicine: opioid toxicity, treatment and management. 2011.
O’Donnell K, Ewald M. Poisonings. In: Kleigman R, Stanton B, III JG, Schor N, Behrman R, editors. Nelson textbook of pediatrics. Philadelphia: Saunders; 2011.
Kosten TR. Chapter 393. Opioid drug abuse and dependence. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, editors. Harrison’s principles of internal medicine, 18e. New York, NY: The McGraw-Hill Companies; 2012
Ford M. Acute poisoning. In: Goldman L, Schager A, editors. Goldman’s Cecil medicine. Philadelphia: Elsevier/Saunders; 2012. p. 670–84.
Common medical emergencies. In: Gomella L, Haist S, editors. Clinicians pocket reference. New York: McGraw-Hill; 2007.
Yaksh T, Wallace M. Opioids, analgesia, and pain management. In: Brunton L, Blumenthal B, Murri N, Hilal-Dandan R, Knollmann B, editors. Goodman & Gilman’s the pharmacological basis of therapeutics. New York: McGraw-Hill; 2011.
Poisoning. In: Stone C, Humphries R, editors. Current diagnosis & treatment: emergency medicine. New York: McGraw-Hill; 2012.
Lank P, Kusin S. Ethanol and opioid intoxication and withdrawal. In: Adams J, Barton E, Collings J, DeBlieux P, Gisondi M, Nadel E, editors. Emergency medicine: clinical essentials. Philadelphia: Elsevier; 2013.
Fukuda K. Opioids. In: Miller R, Eriksson L, Fleisher L, Weiner-Kronish J, Young W, editors. Miller’s anesthesia. Philadelphia: Churchill Livingstone; 2009. p. 769–823.
Rosow C, Dershwitz M. Pharmacology of opioid analgesics. In: Longnecker D, Brown D, Newman M, Zapol W, editors. Anesthesiology. New York: McGraw-Hill; 2012.
Cortazzo MH, Copenhaver, D, Fishman, Scott M. Major opioids and chronic opioid therapy. In: Benzon HT, Rathmell, James P, Wu, Christopher L, Turk, Dennis C, Argoff, Charles E, Hurley, Robert W., editor. Practical Management of Pain. Mosby; 2014. p. 495–507.
Hayes BD. Academic life in emergency medicine: trick of the trade: naloxone dilution for opioid overdose. http://www.aliem.com/2014/trick-trade-naloxone-dilution/. Accessed 30 March 2016
Cadogan M. Life in the fast lane antidotes: naloxone. http://lifeinthefastlane.com/tox-library/antidote/naloxone/. Accessed 30 March 2016
NIH. Monitoring the future 2015 survey results. https://www.drugabuse.gov/related-topics/trends-statistics/infographics/monitoring-future-2015-survey-results. Accessed 30 March 2016
Kim HK, Nelson LS. Reversal of opioid-induced ventilatory depression using low-dose naloxone (0.04 mg): a case series. Journal of Medical Toxicology: Official Journal of the American College of Medical Toxicology. 2015. doi:10.1007/s13181-015-0499-3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
None
Sources of Funding
None
Additional information
Previously Presented as:
Connors NJ, Nelson LS. Wide Variation in Naloxone Dosing Recommendations for Acute Opioid Toxicity. Poster presentation: American College of Medical Toxicology (ACMT) Scientific Meeting. Phoenix, AZ, 2014.
Rights and permissions
About this article
Cite this article
Connors, N.J., Nelson, L.S. The Evolution of Recommended Naloxone Dosing for Opioid Overdose by Medical Specialty. J. Med. Toxicol. 12, 276–281 (2016). https://doi.org/10.1007/s13181-016-0559-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13181-016-0559-3