Abstract
Background/aims
The reciprocal promotion of cancer and stroke occurs due to changes in shared risk factors, such as metabolic pathways and molecular targets, creating a “vicious cycle.” Cancer plays a direct or indirect role in the pathogenesis of ischemic stroke (IS), along with the reactive medical approach used in the treatment and clinical management of IS patients, resulting in clinical challenges associated with occult cancer in these patients. The lack of reliable and simple tools hinders the effectiveness of the predictive, preventive, and personalized medicine (PPPM/3PM) approach. Therefore, we conducted a multicenter study that focused on multiparametric analysis to facilitate early diagnosis of occult cancer and personalized treatment for stroke associated with cancer.
Methods
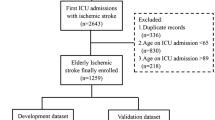
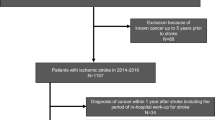
Admission routine clinical examination indicators of IS patients were retrospectively collated from the electronic medical records. The training dataset comprised 136 IS patients with concurrent cancer, matched at a 1:1 ratio with a control group. The risk of occult cancer in IS patients was assessed through logistic regression and five alternative machine-learning models. Subsequently, select the model with the highest predictive efficacy to create a nomogram, which is a quantitative tool for predicting diagnosis in clinical practice. Internal validation employed a ten-fold cross-validation, while external validation involved 239 IS patients from six centers. Validation encompassed receiver operating characteristic (ROC) curves, calibration curves, decision curve analysis (DCA), and comparison with models from prior research.
Results
The ultimate prediction model was based on logistic regression and incorporated the following variables: regions of ischemic lesions, multiple vascular territories, hypertension, D-dimer, fibrinogen (FIB), and hemoglobin (Hb). The area under the ROC curve (AUC) for the nomogram was 0.871 in the training dataset and 0.834 in the external test dataset. Both calibration curves and DCA underscored the nomogram’s strong performance.
Conclusions
The nomogram enables early occult cancer diagnosis in hospitalized IS patients and helps to accurately identify the cause of IS, while the promotion of IS stratification makes personalized treatment feasible. The online nomogram based on routine clinical examination indicators of IS patients offered a cost-effective platform for secondary care in the framework of PPPM.




Similar content being viewed by others
Data availability
The datasets upholding the outcomes of this study can be accessed through a judicious solicitation to the corresponding author.
Code availability
All software applications used are included in this article.
Abbreviations
- AUC:
-
Area under the ROC curve
- AUC-ROC:
-
Area under the receiver operating characteristic curves
- BBB:
-
Blood-brain barrier
- CA:
-
Carbohydrate antigen
- CI:
-
Confidence interval
- DALYs:
-
Disability-adjusted life years
- DCA:
-
Decision curve analysis
- DWI:
-
Diffusion-weighted imaging
- FIB:
-
Fibrinogen
- Hb:
-
Hemoglobin
- ICA:
-
Internal carotid artery
- IS:
-
Ischemic stroke
- LDA:
-
Linear discriminant analysis
- LDH:
-
Lactic dehydrogenase
- MRI:
-
Magnetic resonance imaging
- ORs:
-
Odds ratios
- PLT:
-
Platelet count
- PPPM/3PM:
-
Predictive, preventive, and personalized medicine
- ROC:
-
Receiver operating characteristic
- SBI:
-
Silent brain microinfarction
- SVM:
-
Support vector machine
- VBA:
-
Vertebral-basilar artery
- WSO:
-
World Stroke Organization
References
Feigin VL, Owolabi MO. Pragmatic solutions to reduce the global burden of stroke: a world stroke organization-lancet neurology commission. Lancet Neurol. 2023;22(12):1160–206. https://doi.org/10.1016/s1474-4422(23)00277-6.
Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820. https://doi.org/10.1016/s1474-4422(21)00252-0.
Navi BB, Iadecola C. Ischemic stroke in cancer patients: a review of an underappreciated pathology. Ann Neurol. 2018;83(5):873–83. https://doi.org/10.1002/ana.25227.
Chae WH, Vössing A, Li Y, et al. Treatment of acute ischemic stroke in patients with active malignancy: insight from a comprehensive stroke center. Ther Adv Neurol Disord. 2023;16:17562864231207508. https://doi.org/10.1177/17562864231207508.
Seystahl K, Hug A, Weber SJ, et al. Cancer is associated with inferior outcome in patients with ischemic stroke. J Neurol. 2021;268(11):4190–202. https://doi.org/10.1007/s00415-021-10528-3.
Costamagna G, Hottinger A, Milionis H, et al. Clinical and demographic characteristics, mechanisms, and outcomes in patients with acute ischemic stroke and newly diagnosed or known active cancer. Neurology. 2023;100(24):e2477–89. https://doi.org/10.1212/wnl.0000000000207341.
Dearborn JL, Urrutia VC, Zeiler SR. Stroke and cancer- a complicated relationship. J Neurol Transl Neurosci. 2014;2(1):1039.
Castro HHG, Alencar AP, Bensenor IM, Lotufo PA, Goulart AC. Multimorbidities are associated to lower survival in ischaemic stroke: results from a Brazilian Stroke Cohort (EMMA Study). Cerebrovasc Dis. 2017;44(3–4):232–9. https://doi.org/10.1159/000479827.
Lin J, Wu S, Xu R, et al. Clinical Characteristics and risk factors of lung cancer-associated acute ischemic stroke. Biomed Res Int. 2019;2019:6021037. https://doi.org/10.1155/2019/6021037.
Rioux B, Touma L, Nehme A, Gore G, Keezer MR, Gioia LC. Frequency and predictors of occult cancer in ischemic stroke: a systematic review and meta-analysis. Int J Stroke. 2021;16(1):12–9. https://doi.org/10.1177/1747493020971104.
Wang W, Yan Y, Guo Z, et al. All around suboptimal health - a joint position paper of the suboptimal health study consortium and european association for predictive preventive and personalised medicine. EPMA J. 2021;12(4):403–33. https://doi.org/10.1007/s13167-021-00253-2.
Golubnitschaja O, Potuznik P, Polivka J Jr, et al. Ischemic stroke of unclear aetiology: a case-by-case analysis and call for a multi-professional predictive, preventive and personalised approach. EPMA J. 2022;13(4):535–45. https://doi.org/10.1007/s13167-022-00307-z.
Navi BB, Kasner SE, Elkind MSV, Cushman M, Bang OY, DeAngelis LM. Cancer and embolic stroke of undetermined source. Stroke. 2021;52(3):1121–30. https://doi.org/10.1161/strokeaha.120.032002.
Jiang J, Shang X, Zhao J, et al. Score for predicting active cancer in patients with ischemic stroke: a retrospective study. Biomed Res Int. 2021;2021:5585206. https://doi.org/10.1155/2021/5585206.
Selvik HA, Bjerkreim AT, Thomassen L, Waje-Andreassen U, Naess H, Kvistad CE. When to screen ischaemic stroke patients for cancer. Cerebrovasc Dis. 2018;45(1–2):42–7. https://doi.org/10.1159/000484668.
Seystahl K, Gramatzki D, Wanner M, et al. A risk model for prediction of diagnosis of cancer after ischemic stroke. Sci Rep. 2023;13(1):111. https://doi.org/10.1038/s41598-022-26790-y.
Grisold W, Oberndorfer S, Struhal W. Stroke and cancer: a review. Acta Neurol Scand. 2009;119(1):1–16. https://doi.org/10.1111/j.1600-0404.2008.01059.x.
Kubatka P, Mazurakova A, Koklesova L, et al. Antithrombotic and antiplatelet effects of plant-derived compounds: a great utility potential for primary, secondary, and tertiary care in the framework of 3P medicine. EPMA J. 2022;13(3):407–31. https://doi.org/10.1007/s13167-022-00293-2.
Polivka J Jr, Kralickova M, Polivka J, Kaiser C, Kuhn W, Golubnitschaja O. Mystery of the brain metastatic disease in breast cancer patients: improved patient stratification, disease prediction and targeted prevention on the horizon? EPMA J. 2017;8(2):119–27. https://doi.org/10.1007/s13167-017-0087-5.
Nouh AM, Staff I, Finelli PF. Three Territory Sign: an MRI marker of malignancy-related ischemic stroke (Trousseau syndrome). Neurol Clin Pract. 2019;9(2):124–8. https://doi.org/10.1212/CPJ.0000000000000603.
Gon Y, Okazaki S, Terasaki Y, et al. Characteristics of cryptogenic stroke in cancer patients. Ann Clin Transl Neurol. 2016;3(4):280–7. https://doi.org/10.1002/acn3.291.
Grazioli S, Paciaroni M, Agnelli G, et al. Cancer-associated ischemic stroke: a retrospective multicentre cohort study. Thromb Res. 2018;165:33–7. https://doi.org/10.1016/j.thromres.2018.03.011.
Quintas S, Rogado J, Gullon P, et al. Predictors of unknown cancer in patients with ischemic stroke. J Neurooncol. 2018;137(3):551–7. https://doi.org/10.1007/s11060-017-2741-0.
Lee MJ, Chung JW, Ahn MJ, et al. Hypercoagulability and mortality of patients with stroke and active cancer: the OASIS-CANCER study. J Stroke. 2017;19(1):77–87. https://doi.org/10.5853/jos.2016.00570.
Kono T, Ohtsuki T, Hosomi N, et al. Cancer-associated ischemic stroke is associated with elevated D-dimer and fibrin degradation product levels in acute ischemic stroke with advanced cancer. Geriatr Gerontol Int. 2012;12(3):468–74. https://doi.org/10.1111/j.1447-0594.2011.00796.x.
Vermeer SE, Longstreth WT Jr, Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007;6(7):611–9. https://doi.org/10.1016/s1474-4422(07)70170-9.
Han H, Guo W, Shi W, et al. Hypertension and breast cancer risk: a systematic review and meta-analysis. Sci Rep. 2017;7:44877. https://doi.org/10.1038/srep44877.
Liang Z, Xie B, Li J, et al. Hypertension and risk of prostate cancer: a systematic review and meta-analysis. Sci Rep. 2016;6:31358. https://doi.org/10.1038/srep31358.
Copland E, Canoy D, Nazarzadeh M, et al. Antihypertensive treatment and risk of cancer: an individual participant data meta-analysis. Lancet Oncol. 2021;22(4):558–70. https://doi.org/10.1016/S1470-2045(21)00033-4.
Ahmad FB, Anderson RN. The leading causes of death in the US for 2020. JAMA. 2021;325(18):1829–30. https://doi.org/10.1001/jama.2021.5469.
Vandenberghe D, Albrecht J. The financial burden of non-communicable diseases in the European Union: a systematic review. Eur J Public Health. 2020;30(4):833–9. https://doi.org/10.1093/eurpub/ckz073.
Simonetto M, Rutrick S, LeMoss NM, et al. Adherence to guideline-recommended cancer screening in stroke survivors: a nationwide analysis. J Stroke Cerebrovasc Dis. 2022;31(3):106297. https://doi.org/10.1016/j.jstrokecerebrovasdis.2021.106297.
Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021;52(7):e364–467. https://doi.org/10.1161/STR.0000000000000375.
Golubnitschaja O, Liskova A, Koklesova L, et al. Caution, “normal” BMI: health risks associated with potentially masked individual underweight-EPMA Position Paper 2021. EPMA J. 2021;12(3):243–64. https://doi.org/10.1007/s13167-021-00251-4.
Kropp M, De Clerck E, Vo TKS, Thumann G, Costigliola V, Golubnitschaja O. Short communication: unique metabolic signature of proliferative retinopathy in the tear fluid of diabetic patients with comorbidities - preliminary data for PPPM validation. EPMA J. 2023;14(1):43–51. https://doi.org/10.1007/s13167-023-00318-4.
Crigna AT, Samec M, Koklesova L, et al. Cell-free nucleic acid patterns in disease prediction and monitoring-hype or hope? EPMA J. 2020;11(4):603–27. https://doi.org/10.1007/s13167-020-00226-x.
Nezu T, Hosomi N, Naito H, et al. Clinical characteristics and tumor markers in ischemic stroke patients with active cancer. Intern Emerg Med. 2022;17(3):735–41. https://doi.org/10.1007/s11739-021-02862-1.
Wilbers J, Sondag L, Mulder S, Siegerink B, van Dijk EJ. Cancer prevalence higher in stroke patients than in the general population: the Dutch String-of-Pearls Institute (PSI) Stroke study. Eur J Neurol. 2020;27(1):85–91. https://doi.org/10.1111/ene.14037.
Verhoeven JI, Fan B, Broeders MJM, et al. Association of stroke at young age with new cancer in the years after stroke among patients in the Netherlands. JAMA Netw Open. 2023;6(3):e235002. https://doi.org/10.1001/jamanetworkopen.2023.5002.
Funding
We acknowledge the substantial support rendered by the Natural Science Foundation of China (Grants nos. 82072777), the Key Project of Natural Science Foundation of Fujian Province (Grants nos. 2021J02057), and the Natural Science Foundation of Fujian Province (Grants nos. 2022J011358, 2022J011365, 2020J02063). Additionally, we extend our gratitude to the Medical and Health Key Project of Xiamen (Grants nos. 3502Z20204006), as well as the Xiamen Municipal Health Commission and the Xiamen Municipal Bureau of Science and Technology (Grants nos. 3502Z20209005).
Author information
Authors and Affiliations
Contributions
We present a comprehensive summary of the roles undertaken by the authors in this scholarly endeavor. The conceptualization was primarily orchestrated by J.F. and Q.M., whereas the study design was meticulously crafted by J.F. and J.W. In consonance, data collection and quality control were executed by the entire team. The analytical facet of data was proficiently managed by J.W. Subsequently, the initial manuscript draft was skillfully composed by J.W., with subsequent iterations and editing being jointly administered by J.F. and J.W. Lastly, the ultimate manuscript was reviewed and endorsed by all authors, underscoring their collective commitment. This collaborative effort underscores their involvement in writing, substantiates their engagement with the manuscript, and attests to their consensus on its finalization.
Corresponding authors
Ethics declarations
Ethics approval
Approval for the study was duly granted by the Ethics Committee of the First Affiliated Hospital of Xiamen University (ID: XMYY-2021KYSB074).
Consent to participate
Given the retrospective, non-interventional nature of this study wherein the personal data of patients were not gathered, the requirement for informed consent was duly obviated.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Disclaimer
It is pertinent to note that the funders played no role in shaping the study’s inception and execution, encompassing aspects such as design, data collection, analysis, and manuscript preparation, review, and final endorsement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fang, J., Wu, J., Hong, G. et al. Cancer screening in hospitalized ischemic stroke patients: a multicenter study focused on multiparametric analysis to improve management of occult cancers. EPMA Journal 15, 53–66 (2024). https://doi.org/10.1007/s13167-024-00354-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-024-00354-8