Abstract
Purpose
The objective of this study was to evaluate whether uptake on 18F-fluorodeoxyglucose (18F-FDG) PET could help differentiate HER2-positive from HER2-negative breast cancer brain metastases.
Methods
In this retrospective, cross-sectional study of a cohort of 14 histologically proven breast cancer brain metastases, we analyzed both preoperative 18F-FDG PET/CT and HER2 status of the resected/biopsied brain specimens. The maximum standardized uptake values (SUVmax) of the lesions were normalized to contralateral normal white matter and compared using Mann–Whitney U tests.
Results
The study cohort was comprised of 12 women with breast cancer with a mean age of 59 years (range: 43–76 years) with a total of 14 distinct brain metastatic lesions. The SUVmax ratio of HER2-positive breast cancer brain metastases was significantly greater than that of HER2-negative lesions (3.98 vs 1.79, U = 38.00, p = 0.008).
Conclusion
The SUVmax ratio may help to identify the HER2 status of breast cancer brain metastases, if validated prospectively.
Similar content being viewed by others
Introduction
Approximately 30–50% of patients with metastatic breast cancer develop brain metastases [1]. Patients with human epidermal growth factor 2 (HER2)-positive breast cancer have an even greater risk of developing brain metastases when compared to patients with HER2-negative breast cancer [2]. Among women with metastatic HER2 positive breast cancer, 19% have central nervous system (CNS) metastases at diagnosis, and greater than 50% will develop brain metastases over the course of their disease [3,4,5]. Historically, HER2-positive breast cancers have been associated with a more aggressive clinical course and poorer cancer-specific outcomes in comparison to HER2-negative breast cancers [6, 7]. However, HER2-directed therapies, such as trastuzumab, pertuzumab, and trastuzumab deruxtecan, have been shown to improve survival outcomes for patients at all stages of HER2-positive breast cancer [1, 6, 8,9,10].
Because of tumor heterogeneity and the influence of systemic therapy, HER2 status in a patient can change over the course of time. Multiple groups have reported the presence of HER2 status discordance between the primary breast cancer and metastatic sites, such as within the brain [11,12,13,14]. Prior studies have shown that there is discordance between the HER2 status of the brain metastasis and the primary breast cancer in 10–15% of patients [14, 15]. Because repeated biopsies of brain lesions are neither feasible nor practical, a non-invasive method of determining candidacy for HER2-directed therapies is needed.
Several studies have shown that HER2 overexpression promotes glucose uptake and metabolism [16, 17]. Kim et al. evaluated the 18F-FDG PET uptake of primary breast cancers and found that HER2-positive breast cancers exhibited more avid 18F-FDG uptake than HER2-negative breast cancers [18]. The goal of this proof-of-concept, pilot study was to investigate whether 18F-FDG PET uptake could help differentiate HER2-positive from HER2-negative breast cancer brain metastases.
Materials and Methods
Patients
We queried our institution’s pathology database to identify all histologically proven cases of breast cancer brain metastases from 2018 to 2022. Fifty-seven histologically proven lesions were identified in this query. Eligibility criteria included patients with a histologically confirmed breast cancer brain metastasis and preoperative 18F-FDG PET/CT imaging of the brain. Forty-three lesions were excluded due to lack of a preoperative 18F-FDG PET/CT imaging of the brain, resulting in a study cohort of 14 histologically proven lesions. The cohort of 14 histologically proven lesions corresponded to a total of 12 patients, all of whom were women. Two patients each had two HER2-positive lesions. Seven of the 14 brain metastases (50%) were diagnosed at resection, while the remaining 7 brain metastases (50%) were diagnosed at biopsy. For all 14 lesions, HER2 analyses were performed on the resected/biopsied brain specimens. 18F-FDG PET/CT imaging for each of the lesions was acquired prior to treatment. This cross-sectional study was approved by the Institutional Review Board; informed consent was waived due to the retrospective nature of this study.
Brain 18F-FDG PET-CT Acquisition
After fasting for a minimum of 8 h and resting for 10 min in a quiet room, patients received an intravenous dose of approximately 5 MBq/kg of 18F-FDG, followed by a 60-min uptake period. All patients had a serum glucose level less than 120 mg/dL at the time of injection. All 18F-FDG PET-CT examinations were performed on the Discovery STE scanner (GE Healthcare, Milwaukee, Wisconsin, USA) or the Biograph Vision scanner (Siemens Medical Solutions, Erlangen, Germany). Helical low dose, non-contrast CT images (tube voltage 100 kVp, current intensity 62 mAs, slice thickness 3.75 mm) were obtained for attenuation correction, similar to other groups [18, 19]. PET images were acquired in three-dimensional mode and reconstructed to 128 × 128 image matrices using an iterative algorithm. Images were sent to our institution’s picture archiving and communications system (Sectra PACS, Sectra Medical, Linkoping, Sweden).
Image Analyses
A fellowship-trained neuroradiologist with 5 years of experience (who was blinded to the HER2 status of the breast cancer brain metastases) placed an approximately 50 mm2 circular region of interest (ROI) on the most intensely 18F-FDG-avid part of each lesion. A fellowship trained neuroradiologist with 20 years of experience (who was also blinded to the HER2 status of the breast cancer brain metastases) reviewed each ROI for appropriate placement. The maximum standardized uptake value (SUVmax) within each ROI was recorded. An approximately 50 mm2 circular ROI was placed in the contralateral normal-appearing white matter as a standard internal reference. The SUVmax ratio was obtained for each lesion by dividing the SUVmax of the lesion by the SUVmax of the contralateral normal-appearing white matter. Each patient in the study cohort also had a preoperative contrast-enhanced brain MRI. The maximal lesion diameter on axial contrast-enhanced images from the preoperative brain MRI was measured to obtain the size of each lesion.
HER2 Status Assessment
Immunohistochemistry (IHC) and fluorescent in situ hybridization (FISH) were performed to determine the HER2 status of the resected/biopsied brain specimens. The FDA-approved Ventana PATHWAY 4B5 clone (Ventana, Tucson, Arizona, USA) was utilized for IHC analyses. Subspecialty-trained breast pathologists interpreted the IHC analyses according to the 2018 American Society of Clinical Oncology (ASCO)/College of American Pathologists (CAP) practice guidelines [20]. The PathVysion HER2 DNA Probe Kit (Abbott Laboratories, Abbott Park, Illinois, USA) was used for FISH analyses for the detection of HER2 gene amplification. Board-certified cytogeneticists interpreted the FISH analyses according to the 2018 ASCO/CAP practice guidelines. Formalin-fixed, paraffin-embedded tissue sections of the resected or biopsied brain metastases were used for all HER2 tests. A brain metastasis was classified as HER2-positive if the brain metastasis met the criteria for HER2 positivity in the 2018 ASCO/CAP practice guidelines by either FISH or IHC.
All 14 breast cancer brain metastases in our study cohort underwent IHC analyses. Twelve of the 14 breast cancer brain metastases in our cohort underwent FISH analyses. The results of the HER2 IHC and FISH analyses were obtained from the pathology reports in our institution’s electronic medical record. Estrogen receptor (ER) and progesterone receptor (PR) status and tumor grade were also obtained from the pathology reports in our institution’s electronic medical record. For 10 of the 14 breast cancer brain metastases in our cohort, the tumor grade of the breast cancer brain metastasis was specified in the pathology report. For the other 4 breast cancer brain metastases in our study cohort, tumor grade was not specified in the pathology report. In these cases, tumor grade was obtained from the pathology report for the primary breast cancer.
Statistical Analyses
Mann–Whitney U tests were utilized to compare the SUVmax ratio of HER2-positive lesions and HER2-negative lesions. Mann–Whitney U and Chi-squared tests were utilized to compare the lesion size and location distribution, as well as the ER and PR status, of the HER2-positive and HER2-negative breast cancer brain metastases. Differences with p-values less than 0.05 were considered statistically significant. SPSS 27 (IBM Corp, Armonk, NY, USA) was used to perform the statistical analyses. To account for potential clustering effects, the data were also analyzed including only one lesion per patient. To account for potential effects from scanner differences, the data were analyzed including only lesions that were imaged on the GE Discovery STE scanner. To account for potential effects from differences in tumor grade, the data were analyzed including only grade 3 lesions.
Results
HER2-Positive and HER2-Negative Breast Cancer Brain Metastases
Baseline characteristics for the breast cancer brain metastases in our study cohort are shown in Table 1. The mean patient age at diagnosis was 59 years (range: 43–76 years). The mean time from PET/CT imaging to resection or biopsy was 47 days (range: 7–181 days). Of the 14 total breast cancer brain metastases in our study cohort, 10 of the lesions were HER2-positive, and 4 of the lesions were HER2-negative. The mean lesion size was 3.2 cm for HER2-positive breast cancer brain metastases and 3.5 cm for HER2-negative breast cancer brain metastases; this difference was not statistically significant (U = 17.00, p = 0.73). The location distribution was not significantly different between the HER2-positive and HER2-negative breast cancer brain metastases (χ2 = 3.38, p = 0.34). The ER status (χ2 = 0.53, p = 0.47) and PR status (χ2 = 1.26, p = 0.26) were not significantly different between the HER2-positive and HER2-negative breast cancer brain metastases. The majority of the lesions in our study cohort had a high tumor grade (13/14). Eleven of the lesions were imaged on the GE Discovery STE scanner, while the remaining 3 lesions were imaged on the Siemens Biograph Vision scanner.
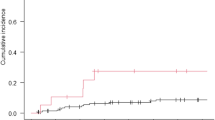
SUVmax Ratio
The SUVmax ratio of HER2-positive breast cancer brain metastases was significantly greater than the SUVmax ratio of HER2-negative breast cancer brain metastases (3.98 vs 1.79, U = 38.00, p = 0.008), as presented in Figs. 1, 2, 3. The SUVmax of HER2-positive breast cancer brain metastases was greater than the SUVmax of HER2-negative breast cancer brain metastases, although this difference was not statistically significant (14.82 vs 7.88, U = 32.50, p = 0.076). The SUVmax of the contralateral normal-appearing white matter was not significantly different between HER2-positive and HER2-negative breast cancer brain metastases (3.82 vs, 4.48, U = 9.50, p = 0.142).
18F-FDG PET/CT and contrast-enhanced MRI images of a HER2-positive breast cancer metastasis. Non-contrast CT (A), 18F-FDG PET (B), fused 18F-FDG PET and CT (C), and axial T1-weighted post-contrast (D) images of a HER2-positive breast cancer brain metastasis in a 44-year-old woman. A representative region of interest is shown in white. This lesion had an SUVmax ratio of 4.99. 18F-FDG = 18F-fluorodeoxyglucose. SUVmax = maximum standardized uptake value
18F-FDG PET/CT and contrast-enhanced MRI images of a HER2-negative breast cancer metastasis. Non-contrast CT (A), 18F-FDG PET (B), fused 18F-FDG PET and CT (C), and axial T1-weighted post-contrast (D) images of a HER2-negative breast cancer brain metastasis in a 68-year-old woman. A representative region of interest is shown in white. This lesion had an SUVmax ratio of 2.19. 18F-FDG = 18F-fluorodeoxyglucose. SUVmax = maximum standardized uptake value
To account for potential clustering effects, the data were also analyzed including only one lesion per patient. The results were similar. The SUVmax ratio of HER2-positive lesions was significantly greater than the SUVmax ratio of the HER2-negative lesions (4.31 vs 1.78, U = 31.00, p = 0.008).
To account for potential effects from scanner differences, the data were analyzed including only lesions that were imaged on the GE Discovery STE scanner. The results were similar. The SUVmax ratio of HER2-positive lesions was significantly greater than the SUVmax ratio of HER2-negative lesions (4.07 vs 1.92, U = 22.00, p = 0.048).
To account for potential effects from differences in tumor grade, the data were analyzed including only grade 3 lesions. The results were similar. The SUVmax ratio of HER2-positive lesions was significantly greater than the SUVmax ratio of HER2-negative lesions (3.98 vs 1.63, U = 30.00, p = 0.007).
Discussion
We found that the SUVmax ratio of HER2-positive breast cancer brain metastases was significantly greater than the SUVmax ratio of HER2-negative breast cancer brain metastases. To our knowledge, our study is the first to demonstrate an association between uptake on 18F-FDG PET and the HER2 status of breast cancer brain metastases.
Survival outcomes for patients with HER2-positive metastatic breast cancer have significantly improved due to the development of effective HER2-directed therapies. These therapies have converted what once was an extremely aggressive cancer into a chronic disease. With HER2-directed agents, approximately 38% of patients with HER2-positive metastatic breast cancer are still alive eight years after the development of metastatic disease [21]. Patients with HER2-positive metastatic breast cancer are now living longer, and greater than 50% of women with HER2-positive metastatic breast cancer will develop brain metastases over the course of their disease. Fortunately, these new HER2-directed agents have shown great efficacy in treating brain metastases and thus can delay the need for whole brain irradiation and its accompanying toxicity (most notably cognitive impairment) [2, 22,23,24]. However, the current assessment of the HER2 status of brain metastases requires pathologic tissue sampling for either IHC or FISH analyses. Because it is often not feasible nor practical to biopsy every CNS lesion, a non-invasive imaging biomarker for HER2 status in breast cancer brain metastases is clearly needed and may help to guide individualized therapy.
The mechanism for the association of 18F-FDG PET uptake and HER2 status is not yet known. However, we suspect that this association may be related to HER2-driven glucose uptake and metabolism [16]. HER2 overexpression has been shown to trigger a signal transduction cascade involving dihydroceramide desaturase 1 (DES1) that promotes increased glucose uptake and reprogramming of metabolic pathways [25]. HER2 overexpression in breast cancer cell lines promotes aerobic glycolysis and increased glucose consumption [17].
There are several potential limitations to our study. First, this was a small, proof-of-concept, exploratory study assessing the association between 18F-FDG PET uptake and HER2 status. Our findings should be validated in a large prospective trial. The size of our study cohort is partially due to the fact that we included only histologically proven breast cancer brain metastases with HER2 analyses of the resected or biopsied brain specimens. In contradistinction to many of the published studies investigating imaging biomarkers of HER2 status, which have correlated brain MRI imaging parameters with the HER2 status of the primary breast cancer [26,27,28,29], our study correlated 18F-FDG PET uptake with the HER2 status of the breast cancer brain metastases. This is a crucial distinction, as there is discordance between the HER2 status of the breast cancer brain metastasis and the HER2 status of the primary breast cancer in 10–15% of patients [14, 15]. Second, due to the retrospective nature of our study, all of the brain metastases were not imaged with the same PET/CT scanner. Nevertheless, most of the lesions (11 of 14) were imaged on the GE Discovery STE scanner, while the remaining 3 lesions were imaged on the Siemens Biograph Vision scanner. When the data were analyzed including only lesions imaged on the GE Discovery STE scanner, the results were similar. In addition, in our analyses, SUVmax values were normalized to a standard internal control, contralateral normal-appearing white matter. Third, we did not have follow-up 18F-FDG PET imaging for the breast cancer brain metastases in our study cohort. As a result, we could not investigate whether uptake on 18F-FDG PET could be utilized longitudinally to evaluate the HER2 status of breast cancer brain metastases.
Several investigators have evaluated MRI biomarkers to determine the HER2 status of breast cancer brain metastases. The intensity of enhancement on contrast-enhanced brain MRI has been shown to have an association with the HER2 status of breast cancer brain metastases [30]. In addition, lesion contour and lesion composition on brain MRI have been shown to be associated with HER2 status [31]. The relative cerebral blood volume from dynamic susceptibility contrast-enhanced perfusion brain MRI has been shown to be associated with HER2 status [32]. Because of the small size of our study cohort, we chose to focus on the difference in 18F-FDG PET uptake between HER2-positive and HER2-negative breast cancer brain metastases. Future large prospective trials should evaluate the effectiveness of combining 18F-FDG PET uptake and MRI features in differentiating HER2-positive and HER2-negative breast cancer brain metastases.
While breast cancer commonly metastasizes to other organs (such as the lungs and bones), in addition to the brain, our study focused on the association between 18F-FDG PET uptake and the HER2 status of breast cancer brain metastases because patients with HER2-positive breast cancer have a greater likelihood of developing brain metastases, and determining the HER2 status of breast cancer brain metastases noninvasively has a direct impact on clinical management. New HER2-directed therapies are effective in treating brain metastases and can potentially spare patients from receiving whole brain irradiation and its associated toxicities. In addition, identifying a non-invasive imaging biomarker for HER2 status in breast cancer brain metastases can potentially spare patients from the risks associated with brain biopsies. Future studies should examine the association between 18F-FDG PET uptake and the HER2 status of breast cancer lung and bone metastases.
Uptake on 18F-FDG PET may assist in differentiating HER2-positive breast cancer brain metastases from HER2-negative lesions, if validated in a large prospective trial. A non-invasive method of identifying the HER2 status of breast cancer brain metastases may help to guide personalized patient care while avoiding the risks of brain biopsy. Furthermore, a baseline 18F-FDG PET prior to treatment may be helpful to evaluate new brain metastases and to compare their 18F-FDG uptake profiles to prior treated lesions.
Data Availability
The data are available to qualified investigators upon reasonable request.
Abbreviations
- HER2:
-
Human epidermal growth factor receptor 2
- CNS:
-
Central nervous system
- 18F-FDG:
-
18F-fluorodeoxyglucose
- ROI:
-
Region of interest
- SUVmax:
-
Maximum standardized uptake value
- IHC:
-
Immunohistochemistry
- FISH:
-
Fluorescent in situ hybridization
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- ROC:
-
Receiver operating characteristic
References
Garcia-Alvarez A, Papakonstantinou A, Oliveira M. Brain metastases in HER2-positive breast cancer: current and novel treatment strategies. Cancers (Basel). 2021;13:2927.
Zimmer AS, Van Swearingen AED, Anders CK. HER2-positive breast cancer brain metastasis: a new and exciting landscape. Cancer Rep (Hoboken). 2020;5: e1274.
Martin AM, Cagney DN, Catalano PJ, Warren LE, Bellon JR, Punglia RS, et al. Brain metastases in newly diagnosed breast cancer: a population-based study. JAMA Oncol. 2017;3:1069–77.
Pestalozzi BC, Holmes E, de Azambuja E, Metzger-Filho O, Hogge L, Scullion M, et al. CNS relapses in patients with HER2-positive early breast cancer who have and have not received adjuvant trastuzumab: a retrospective substudy of the HERA trial (BIG 1–01). Lancet Oncol. 2013;14:244–8.
Lin NU, Amiri-Kordestani L, Palmieri D, Liewehr DJ, Steeg PS. CNS metastases in breast cancer: old challenge, new frontiers. Clin Cancer Res. 2013;19:6404–18.
Wang J, Xu B. Targeted therapeutic options and future perspectives for HER2-positive breast cancer. Signal Transduct Target Ther. 2019;4:34.
Elias SG, Adams A, Wisner DJ, Esserman LJ, van T Veer LJ, et al. Imaging features of HER2 overexpression in breast cancer: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2014;23:1464–83.
Marchiò C, Annaratone L, Marques A, Casorzo L, Berrino E, Sapino A. Evolving concepts in HER2 evaluation in breast cancer: heterogeneity, HER2-low carcinomas and beyond. Semin Cancer Biol. 2021;72:123–5.
Giordano SH, Temin S, Chandarlapaty S, Crews JR, Esteva FJ, Kirshner JJ, et al. Systemic therapy for patients with advanced human epidermal growth factor receptor 2-positive breast cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36:2736–40.
Cortés J, Kim S-B, Chung W-P, Im S-A, Park YH, Hegg R, et al. Trastuzumab deruxtecan versus trastuzumab emtansine for breast cancer. N Engl J Med. 2022;386:1143–54.
Yeh R-H, Yu J-C, Chu C-H, Ho C-L, Kao H-W, Liao G-S, et al. Distinct MR imaging features of triple-negative breast cancer with brain metastasis. J Neuroimaging. 2015;25:474–81.
Hadjipanteli A, Doolan P, Kyriacou E, Constantinidou A. Breast cancer brain metastasis: the potential role of MRI beyond current clinical applications. Cancer Manag Res. 2020;12:9953–64.
Hoefnagel LDC, van de Vijver MJ, van Slooten H-J, Wesseling P, Wesseling J, Westenend PJ, et al. Receptor conversion in distant breast cancer metastases. Breast Cancer Res. 2010;12:R75–R75.
Hulsbergen AFC, Claes A, Kavouridis VK, Ansaripour A, Nogarede C, Hughes ME, et al. Subtype switching in breast cancer brain metastases: a multicenter analysis. Neuro Oncol. 2020;22:1173–81.
Thomson AH, McGrane J, Mathew J, Palmer J, Hilton DA, Purvis G, et al. Changing molecular profile of brain metastases compared with matched breast primary cancers and impact on clinical outcomes. Br J Cancer. 2016;114:793–800.
Chang S, Chesney J, Trent JO, Telang S. Abstract 2519: Targeting glucose metabolism in HER2+breast cancer. Cancer Res. 2021;81:2519–619.
Farhadi P, Yarani R, Valipour E, Kiani S, Hoseinkhani Z, Mansouri K. Cell line-directed breast cancer research based on glucose metabolism status. Biomed Pharmacother. 2022;146: 112526.
Kim JY, Lee SH, Kim S, Kang T, Bae YT. Tumour 18 F-FDG uptake on preoperative PET/CT may predict axillary lymph node metastasis in ER-positive/HER2-negative and HER2-positive breast cancer subtypes. Eur Radiol. 2015;25:1172–81.
Nitchingham A, Pereira JV, Wegner EA, Oxenham V, Close J, Caplan GA. Regional cerebral hypometabolism on 18F-FDG PET/CT scan in delirium is independent of acute illness and dementia. Alzheimers Dement. 2023;19:97–106.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline focused update. Arch Pathol Lab Med. 2018;142:1364–82.
Swain SM, Miles D, Kim S-B, Im Y-H, Im S-A, Semiglazov V, et al. End-of-study analysis from the phase III, randomized, double-blind, placebo (Pla)-controlled CLEOPATRA study of first-line (1L) pertuzumab (P), trastuzumab (H), and docetaxel (D) in patients (pts) with HER2-positive metastatic breast cancer (MBC). J Clin Oncol. 2019;37:1020–120.
Modi S, Saura C, Yamashita T, Park YH, Kim S-B, Tamura K, et al. Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N Engl J Med. 2019;382:610–21.
Saura C, Oliveira M, Feng YH, Dai MS, Chen SW, Hurvitz SA, et al. Neratinib plus capecitabine versus lapatinib plus capecitabine in HER2-positive metastatic breast cancer previously treated with ≥ 2 HER2-directed regimens: Phase III NALA Trial. J Clin Oncol. 2020;38:3138–49.
Lin NU, Borges V, Anders C, Murthy RK, Paplomata E, Hamilton E, et al. Intracranial efficacy and survival with tucatinib plus trastuzumab and capecitabine for previously treated HER2-positive breast cancer with brain metastases in the HER2CLIMB trial. J Clin Oncol. 2020;38:2610–9.
Linzer RW, Guida DL, Aminov J, Snider JM, Khalife G, Buyukbayraktar AB, et al. Dihydroceramide desaturase 1 (DES1) promotes anchorage-independent survival downstream of HER2-driven glucose uptake and metabolism. FASEB J. 2022;36: e22558.
Kyeong S, Cha YJ, Ahn SG, Suh SH, Son EJ, Ahn SJ. Subtypes of breast cancer show different spatial distributions of brain metastases. PLoS ONE. 2017;12: e0188542.
Laakmann E, Witzel I, Scriba V, Grzyska U, Zu Eulenburg C, Burchardi N, et al. Radiological patterns of brain metastases in breast cancer patients: a subproject of the German Brain Metastases in Breast Cancer (BMBC) Registry. Int J Mol Sci. 2016;17:1615.
Ahn SJ, Park M, Bang S, Cho E, Ahn SG, Suh SH, et al. Apparent diffusion coefficient histogram in breast cancer brain metastases may predict their biological subtype and progression. Sci Rep. 2018;8:9947.
Ulu E, Ozturk B, Atalay K, Okumus IB, Erdem D, Gul MK, et al. Diffusion-weighted imaging of brain metastasis: correlation of MRI parameters with histologic type. Turk Neurosurg. 2022;32:58–68.
Young JR, Ressler JA, Mortimer JE, Schmolze D, Fitzgibbons M, Chen BT. Performance of enhancement on brain MRI for identifying HER2 overexpression in breast cancer brain metastases. Eur J Radiol. 2021;144: 109948.
Young JR, Ressler JA, Mortimer JE, Schmolze D, Fitzgibbons M, Chen BT. Association of lesion contour and lesion composition on MR with HER2 status in breast cancer brain metastases. Magn Reson Imaging. 2023;96:60–6.
Young JR, Ressler JA, Shiroishi MS, Mortimer JE, Schmolze D, Fitzgibbons M, et al. Association of relative cerebral blood volume from dynamic susceptibility contrast-enhanced perfusion MR with HER2 status in breast cancer brain metastases. Acad Radiol. 2023;30:1816–22.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium
Author information
Authors and Affiliations
Contributions
Guarantor of integrity of the entire study: Jonathan R. Young, MD. Study concepts and design: Jonathan R. Young, MD; Julie A. Ressler, MD; Joanne E. Mortimer, MD; Daniel Schmolze, MD; Mariko Fitzgibbons, MD; and Bihong T. Chen, MD, PhD. Literature research: Jonathan R. Young, MD; Joanne E. Mortimer, MD; and Daniel Schmolze, MD. Clinical studies: Jonathan R. Young, MD; Julie A. Ressler, MD; Mariko Fitzgibbons, MD; and Bihong T. Chen, MD, PhD. Experimental studies/data analysis: Jonathan R. Young, MD; Julie A. Ressler, MD; Mariko Fitzgibbons, MD; and Bihong T. Chen, MD, PhD. Statistical analysis: Jonathan R. Young, MD and Bihong T. Chen, MD, PhD. Manuscript preparation: Jonathan R. Young, MD. Manuscript editing: Jonathan R. Young, MD; Julie A. Ressler, MD; Joanne E. Mortimer, MD; Daniel Schmolze, MD; Mariko Fitzgibbons, MD; and Bihong T. Chen, MD, PhD.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This cross-sectional study was approved by the Institutional Review Board; informed consent was waived due to the retrospective nature of this study. This study was performed in accordance with the Helsinki declaration as revised in 2013 and its later amendments.
Consent for Publication
Not applicable.
Competing Interests
Jonathan R. Young, MD; Julie A. Ressler, MD; Joanne E. Mortimer, MD; Daniel Schmolze, MD; Mariko Fitzgibbons, MD; and Bihong T. Chen, MD, PhD declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Young, J.R., Ressler, J.A., Mortimer, J.E. et al. Association Between 18F-FDG PET Activity and HER2 Status in Breast Cancer Brain Metastases. Nucl Med Mol Imaging 58, 113–119 (2024). https://doi.org/10.1007/s13139-024-00843-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-024-00843-8