Abstract
Background and purpose
The enzyme methylenetetrahydrofolate reductase (MTHFR) plays a crucial role in directing folate species towards nucleotide synthesis or DNA methylation. The MTHFR polymorphisms C677T and A1298C have been linked to cancer susceptibility, but the evidence supporting this association has been equivocal. To investigate the individual and joint associations between MTHFR C677T, A1298C, and digestive system cancer in a Chinese hypertensive population, we conducted a population-based case–control study involving 751 digestive system cancer cases and one-to-one matched controls from the China H-type Hypertension Registry Study (CHHRS).
Methods
We utilized the conditional logistic regression model to evaluate multivariate odds ratios (ORs) and 95% confidence intervals (CIs) of digestive system cancer.
Results
The analysis revealed a significantly lower risk of digestive system cancer in individuals with the CT genotype (adjusted OR: 0.71; 95% CI 0.52, 0.97; P = 0.034) and TT genotype (adjusted OR: 0.57; 95% CI 0.40, 0.82; P = 0.003; P for trend = 0.003) compared to those with the 677CC genotype. Although A1298C did not show a measurable association with digestive system cancer risk, further stratification of 677CT genotype carriers by A1298C homozygotes (AA) and heterozygotes (AC) revealed a distinct trend within these subgroups.
Conclusion
These findings indicate a potential protective effect against digestive system cancer associated with the T allele of MTHFR C677T. Moreover, we observed that the presence of different combinations of MTHFR polymorphisms may contribute to varying susceptibilities to digestive system cancer.
Similar content being viewed by others
1 Introduction
One-carbon metabolism (OCM) is characterized by two main branches: one consists of reactions involving purine and thymidine synthesis, and the other is responsible for the synthesis of S-adenosylmethionine (SAM) for methylation reactions, including DNA methylation [1], and both pathways are implicated in human carcinogenesis [2,3,4]. The enzyme 5,10-methylenetetrahydrofolate reductase (MTHFR) catalyzes the irreversible conversion of 5,10-methylenetetrahydrofolate to 5- methyltetrahydrofolate (5-MTHF), the primary circulatory form of folate necessary for methionine synthesis [5]. The 5,10-methylenetetrahydrofolate is the folate cofactor for thymidylate synthase [6], thus MTHFR resides at a metabolic branch point for it directs the two folate species, either to nucleotide synthesis or to methylation reaction [7].
To date, many mutations in MTHFR have been identified; the most studied variants of MTHFR are C677T and A1298C. A C to T substitution at nucleotide 677 results in the substitution of a valine codon for alanine, causing an enzyme activity deficiency [5], thus inhibiting the remethylation of homocysteine (Hcy) to methionine, and affecting folate distribution. Many epidemiological studies have demonstrated that this variant results in increased circulating Hcy levels under the condition of impaired folate status [5, 8, 9], as well as clinical implications of cardiovascular disorders [10]. Of note, the prevalence of the MTHFR C677T mutation varies in different ethnicities [11], and it has been reported that Chinese populations have a higher rate of the homozygous variant MTHFR 677TT (~ 25%) [12]. The second most common mutation in MTHFR is A1298C, which changes glutamate into an alanine residue [13]. Studies on the A1298C polymorphism are limited and less documented than those of the C677T allele. It was determined that enzyme activity is 40% lower for this polymorphism in those with the 1298CC genotype (variant homozygotes) than the wildtype 1298AA genotype, but neither the homozygous nor the heterozygous state is associated with significantly higher plasma Hcy levels [13].
For the past decades, the role of OCM and genetic polymorphisms of the enzymes in folate metabolism has attracted much interest in epidemiological research on cancers [14, 15]. The associations between MTHFR polymorphisms and cancer risk have been extensively and widely studied [16,17,18], however, the results have been inconsistent and controversial. It has been reported that the associations for some cancers depend on the ethnicity and folate status of the participants enrolled [19, 20]. Therefore, we conducted a large-scale, case–control study to investigate the associations between these two common variants of MTHFR and the incidence of digestive system cancer in a community-based cohort of Chinese adults. Additionally, we aimed to explore the gene–gene interactions and potential effect modifiers within the OCM pathway.
2 Methods
2.1 Study population
The methods and major results of the China H-type Hypertension Registry Study (CHHRS, clinical trial registration number: ChiCTR1800017274) have been reported elsewhere [21]. Briefly, the CHHRS was a community-based, prospective, observational, real-world study that was conducted in Lianyungang, Jiangsu Province, and Rongcheng, Shandong Province, China. Started in 2016, the CHHRS was designed to investigate the prevalence of H-type hypertension and related risk factors in China. Eligible persons were aged 18 years or older with essential hypertension, defined as seated, systolic blood pressure (SBP) ≥ 140 mm Hg and/or seated, diastolic blood pressure (DBP) ≥ 90 mm Hg at the screening visit. There were no pre-specified exclusion criteria, except for those who were unable to participate in the follow-up or who were unable to demonstrate informed consent according to the study protocol. The study was approved by the Ethics Committee of the Institute of Biomedicine, Anhui Medical University, Hefei, China.
2.2 Primary outcome and case ascertainment
The primary outcome of interest in this study was incident digestive system cancer over the follow-up period from 2016 to 2018, excluding any previous history of cancer or tumor as assessed at the baseline study. Cancer or tumor diagnoses for all participants were obtained from the China Center for Disease Control at Lianyungang and Rongcheng. This information was cross-verified through the national health insurance system, which was electronically linked to all hospitalization data. Additionally, self-reports provided by participants during the follow-up visits, which occurred every three months as part of the CHHRS, contributed to the cross-verification process. All reported cancer cases were coded according to the International Classification of Diseases, 10th Revision (ICD-10).
2.3 Selection of matched case–control pairs
To maximize cost efficiency, the present study adopted a nested, case–control design. As shown in Fig. 1, during the follow-up period, 2021 patients were identified as having physician-diagnosed cancer. Controls were selected from the remaining 232,355 participants who were still alive at the end of the study and had never had cancer prior to or during the follow-up period. Controls were matched with incident cancer cases in a 1:1 ratio based on age (± 1 year), sex, study center, and residence at baseline. We excluded 1268 non-gastrointestinal cancer pairs and 1 pair with missing genotype data, resulting in 751 digestive system cancer case–control pairs for the final analysis.
2.4 Exposure assessment
At baseline, all study participants completed a standard questionnaire interview which included information on age, sex, education, occupation, medical history, current medical conditions, and medication intake. Trained research staff measured height, weight, and seated blood pressure according to the standard study protocol. Smoking habits and alcohol consumption status were collected at baseline, and study participants were grouped into three categories: never-smoker/drinker, ex-smoker/drinker, and current smoker/drinker.
2.5 Laboratory assays
Serum Hcy levels (arsenazo-III method) were measured using automatic clinical analyzers (Beckman Coulter); baseline fasting lipids and glucose levels were measured using automatic clinical analyzers (BeckmanCoulter); serum vitamin B12 and total folate levels were measured using a chemiluminescent immunoassay (New Industrial), as published previously [22]. The MTHFR C677T (rs1801133) and A1298C (rs1801131) polymorphisms were determined by the Taq Man assay as previously published [22]. Serum concentrations of 5-MTHF were measured by liquid chromatography-tandem mass spectrometry (LC–MS/MS) by the Tailored Medical Laboratory in Shenzhen (Shenzhen, China) following standard lab protocol and vigorous quality control procedures.
2.6 Statistical analysis
Continuous variables were reported as mean and standard deviation, while categorical variables were presented as numbers and percentages. To compare the characteristics of cases and controls, nonparametric Wilcoxon rank sum tests were used for continuous variables, and chi-squared tests were employed for categorical variables. P-values were calculated using a two-sided test. Odds ratios and 95% confidence intervals for the association between MTHFR polymorphisms and cancer risk were estimated by conditional logistic regression models. All regression analyses were adjusted for potential confounding variables that may impact the association between the polymorphisms and cancer. This adjustment also considered two specific variables known to be risk factors for cancer, namely smoking and alcohol drinking status.
All statistical analyses were performed using R (version 4.0.5).
3 Results
3.1 Study participants and baseline characteristics
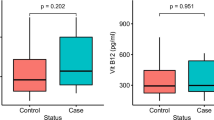
As shown in Fig. 1, 751 digestive system cancer cases and matched controls with complete MTHFR genotypes data were included in the final analysis. Table 1 presents the baseline characteristics of the participants by case–control status. The mean age of participants was 68.2 years and 65.1% were male. The allele frequencies for MTHFR 677-CC, CT, and TT were 21.3%, 57.3%, and 21.4%, respectively among the cases, and 15.3%, 57.5%, and 27.2%, respectively among the controls, the difference between cases and controls was significant (P = 0.002), however, the frequencies of the A1298C (rs1801131) genotypes showed no difference between the two groups. In addition, the proportion of current smoking, former smoking, and never smoking was 32.6%, 11.7%, and 55.7%, respectively for cases, and 26%, 11.7%, and 62.3%, respectively for controls, and this difference was significant (p < 0.014). Other baseline characteristics including education background, Proportion of patients with hypertension, blood pressure, BMI, Fasting glucose, Uric acid, parameters of blood lipid, and serum levels for components of OCM showed no significant differences between the two groups.
3.2 Association between MTHFR C677T, A1298C and the risk of digestive system cancer
For MTHFR C677T, as shown in Table 2, after adjusting for potential confounders, compared to participants with the CC genotype, CT carriers conferred a substantially decreased trend for digestive system cancer risk (adjusted OR 0.71; 95% CI 0.52, 0.97, P = 0.034), as did TT carriers (adjusted OR 0.57; 95% CI 0.40, 0.82, P = 0.003; P for trend = 0.003). However, for the variant of A1298C, compared with the AA genotype, the AC and CC genotypes were not significantly associated with changed cancer risk.
3.3 The joint association of MTHFR C677T and A1298C with digestive system cancer risk
The joint effects of the two MTHFR polymorphisms on digestive system cancer were examined (Table 3). Of note, there were no participants in the subgroup with the 677CT/1298CC combination, nor were there any participants who were homozygous TT at 677 while having a C allele at 1298.
Multivariable logistic regression was conducted to evaluate the joint association of C677T and A1298C (Fig. 2). The 677CT genotype accounted for 57.4% of the total population analyzed in the present study. When stratified by A1298C homozygotes (AA) and heterozygotes (AC), a distinct trend was observed where heterozygotes for both the C677T and A1298C mutation, which accounted for approximately 16.2% of case–control pairs, showed a significantly decreased risk (OR = 0.65; 95% CI 0.44, 0.97; P = 0.033), which was similar to that seen among 677TT homozygotes, but the 677CT/1298AA genotypes showed less of a risk reduction (OR = 0.74; 95% CI 0.53, 1.03; P = 0.074).
ORs and 95%CI of the combination of the C677T and A1298C polymorphisms on the risk of digestive system cancer. Conditional logistic regression models were used. Adjusted for age, sex, study center, education level, smoking status, drinking status, history of hypertension, SBP, body mass index, pulse, total cholesterol, triglycerides, fasting glucose, Vitamin B12, total folate, and Hcy
4 Discussion
In the current study, we evaluated the possible associations between the MTHFR C677T and A1298C polymorphisms and the susceptibility to digestive system cancer, which is ranked the first prevalent cancer subtype in the CHHRS follow-up period. The T allele of CT677T was found to bring a significantly decreased risk of digestive system cancer among Chinese adults with hypertension.
The relationship between the two MTHFR polymorphisms and genetic susceptibility to different types of cancer has been widely evaluated, but the results are controversial. For the C677T variants, and consistent with our results, TT genotype carriers have been shown to exhibit a reduced risk of colorectal cancer [23,24,25], colorectal adenocarcinomas [26], as well as non-digestive system malignancies, including childhood acute lymphoblastic leukemia [27, 28], oral cancer [29], breast cancer [2], and prostate cancer [30]. In addition, the results of several meta-analysis reviews on colorectal cancer were also consistent with the present study [19, 25, 31]. However, other studies have reported that those with the TT genotype had an increased risk of gastric cancer [32, 33] and colorectal cancer [34], whereas some studies failed to find any association between this variant and the risk of colorectal cancer [35], gastric cancer [36, 37], and other non-digestive system cancers [38, 39].
The conflicting results observed in these studies may be caused by small sample size and inadequate statistical power, or due to demographic differences in the study populations. It has been hypothesized that folate status may modify the relationship between the MTHFR C677T polymorphism and cancer. Several case–control studies have shown a more pronounced protective effect for individuals with the 677TT genotype compared with those with the CC genotype in those with adequate dietary folate intake [40], or in populations who live in relatively higher plasma folate regions [20]. This suggests that the impact of MTHFR C677T on cancer development is influenced by dietary folate intake. It is possible that the differential ability of folate metabolism between different genotypes of MTHFR C677T, as well as variations in the forms of folate present, may not be adequately highlighted due to insufficient substrate availability under conditions of low folate intake. However, high alcohol or low methionine intake has been shown to abolish the reduction in the risk of colorectal cancer in individuals with the TT genotype [23, 41]. Further research is necessary to verify and support the reproducibility of these results, as well as to gain a deeper understanding of their potential underlying mechanisms. The MTHFR A1298C polymorphism, however, differed from the C677T, in that we did not observe any significant correlation between this variant and the occurrence of digestive system cancer. This result is in agreement with previously reported results of gastric cancer from meta-analyses [42].
Previous studies have reported that people who are compound heterozygous for the C677T and A1298C alleles, had 50–60% of control enzyme activity, a value that was lower than that of single heterozygotes, and tended to have a biochemical profile similar to C677T homozygous mutation carriers, with lower plasma folate concentrations and elevated Hcy levels [11, 43]. Thus, in our analysis, we explored the combination of the C677T and A1298C polymorphisms on the risk of digestive system cancer for the first time. Interestingly, we found that when the C677T heterozygous genotype was stratified by the A1298C polymorphism, different risks between 677CT/1298AA and 677CT/1298AC genotypes were observed.
The present result is biologically plausible. It has been confirmed that the deficient methylation of dUMP to dTMP and subsequent incorporation of uracil into DNA, could lead to chromosome instability and DNA strand breakage [44], which are often present in human preneoplastic cells and may promote carcinogenesis. The 677TT genotype may reduce cancer risk for it reduces the activity of the thermolabile variant and expands the intracellular pool of 5,10-methylenetetrahydrofolate [45], which is utilized in thymine synthesis, and as a result, the availability of thymine is increased [46] for nucleotide synthesis, and the possibilities of uracil incorporation into DNA are reduced [19, 47]. In agreement with our result, a study examined the combined effect of these two common variants on the MTHFR activities, when compared with individuals who have a 677CT/1298AA genotype, significantly decreased activities were observed in individuals heterozygous for both variants (677CT/1298AC) [13]. Therefore, the variability between carriers of the 677CT/1298AA and the 677CT/1298AC genotypes, combined with the comparability between the 677CT/1298AC and the 677TT genotypes may confirm the hypothesis that the cancer risk difference between genotypes stems from disturbances in the folate metabolism pathway, and this disturbances may be driven by the gradual changed MTHFR activities.
Despite that the C677T transition has been implicated in many disorders [48,49,50] and that it might influence the disease profile in some populations, it should not be regarded a priori as a genetic defect that causes disease. While the MTHFR 677TT genotype does appear to increase the risk of some diseases, it also appears to protect against others. This may explain the observation showing no correlation between this genotype and longevity [51].
This study has several limitations. Firstly, the generalizability of our findings to other populations with different characteristics may be limited since the study population primarily consisted of rural Chinese individuals with hypertension. Secondly, the specific sample size collected in this study might not have been sufficient to detect subtle and intricate correlations. This highlights the need for larger sample sizes in future studies to validate our results. Furthermore, we failed to confirm the hypothesis that analogous cancer risk of 677CT/1298AC genotype and 677TT genotype participants may be sourced from the similarity of folate metabolism profiles as substantial data missing. In addition, we were unable to analyze detailed cancer subtypes due to sample size limitations, and lack of cytohistologic and histopathological data for further classification.
In conclusion, we observed an inverse association of the MTHFR 677TT genotype with digestive system cancer among a Chinese hypertensive population. Our study is the first to demonstrate that different combined genotypes of MTHFR polymorphisms may confer significantly different susceptibilities. Considering the high prevalence and lethality of digestive system cancer in China and around the world, these results may guide precise prevention strategies against this fatal disease.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Matsuo K, Hamajima N, Suzuki R, Ogura M, Kagami Y, Taji H, et al. Methylenetetrahydrofolate reductase gene (MTHFR) polymorphisms and reduced risk of malignant lymphoma. Am J Hematol. 2004;77(4):351–7.
Chou Y, Wu M, Yu J, Lee M, Yang T, Shih H, et al. Genetic polymorphisms of the methylenetetrahydrofolate reductase gene, plasma folate levels and breast cancer susceptibility: a case–control study in Taiwan. Carcinog. 2006;27(11):2295–300.
Nishiyama A, Nakanishi M. Navigating the DNA methylation landscape of cancer. Trends Genet. 2021;37(11):1012–27.
Saghafinia S, Mina M, Riggi N, Hanahan D, Ciriello G. Pan-cancer landscape of aberrant DNA methylation across human tumors. Cell Rep. 2018;25(4):1066-1080.e8.
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, et al. A candidate genetic risk factor for vascular disease a common mutation in methylenetetrahydrofolate reductase. Nat Genet. 1995;10:111–3.
Kim Y. Folate and carcinogenesis: evidence, mechanisms, and implications. J Nutr Biochem. 1999;10:66–88.
Ueland PM, Hustad S, Schneede J, Refsum H, Vollset SE. Biological and clinical implications of the MTHFR C677T polymorphism. Trends Pharmacol Sci. 2001;22(4):195–201.
Murakami S, Matsubara N, Saitoh M, Miyakawa S, Shoji M, Kubo T. The Relation between plasma homocysteine concentration and methylenetetrahydrofolate reductase gene polymorphism in pregnant women. J Obstet Gynaecol Res. 2001;27(6):349–52.
Holmes MV, Newcombe P, Hubacek JA, Sofat R, Ricketts SL, Cooper J, et al. Effect modification by population dietary folate on the association between MTHFR genotype, homocysteine, and stroke risk: a meta-analysis of genetic studies and randomised trials. Lancet. 2011;378(9791):584–94.
Klerk M, Verhoef P, Clarke R, Blom HJ, Kok FJ, Schouten EG, et al. MTHFR 677C→T polymorphism and risk of coronary heart disease. JAMA. 2002;288:2023–31.
Botto LD, Yang Q. 5,10-Methylenetetrahydrofolate reductase gene variants and congenital anomalies: a HuGE review. Am J Epidemiol. 2000;151(9):862–77.
Huang X, Qin X, Yang W, Liu L, Jiang C, Zhang X, et al. MTHFR gene and serum folate interaction on serum homocysteine lowering: prospect for precision folic acid treatment. Arterioscler Thromb Vasc Biol. 2018;38(3):679–85.
van der Put NM, Gabreëls F, Stevens EM, Smeitink JA, Trijbels FJ, Eskes TK, et al. A second common mutation in the methylenetetrahydrofolate reductase gene: an additional risk factor for neural-tube defects? Am J Hum Genet. 1998;62(5):1044–51.
Gong Z, Yao S, Zirpoli G, David Cheng TY, Roberts M, Khoury T, et al. Genetic variants in one-carbon metabolism genes and breast cancer risk in European American and African American women. Int J Cancer. 2015;137(3):666–77.
Li Q, Lan Q, Zhang Y, Bassig BA, Holford TR, Leaderer B, Boyle P, et al. Role of one-carbon metabolizing pathway genes and gene–nutrient interaction in the risk of non-Hodgkin lymphoma. Cancer Causes Control. 2013;24(10):1875–84.
Gong JM, Shen Y, Shan WW, He YX. The association between MTHFR polymorphism and cervical cancer. Sci Rep. 2018;8(1):7244.
Nisevic I, Dinic J, Nikolic A, Djordjevic V, Lukic S, Ugljesic M, et al. MTHFR C677T polymorphism in chronic pancreatitis and pancreatic adenocarcinoma. Cell Biochem Funct. 2008;26(6):659–63.
Shen H, Xu Y, Zheng Y, Qian Y, Yu R, Qin Y, et al. Polymorphisms of 5,10-methylenetetrahydrofolate reductase and risk of gastric cancer in a Chinese population: a case-control study. Int J Cancer. 2001;95:332–6.
Sheng X, Zhang Y, Zhao E, Lu S, Zheng X, Ge H, et al. MTHFR C677T polymorphism contributes to colorectal cancer susceptibility: evidence from 61 case–control studies. Mol Biol Rep. 2012;39(10):9669–79.
Yang Z, Zhang X, Liu H, Hao Y, Zhao C. MTHFR C677T polymorphism and colorectal cancer risk in Asians: a meta-analysis of 21 studies. Asian Pac J Cancer Prev. 2012;13(4):1203–8.
Wei Y, Xu B, He Q, Chen P, Zhang Q, Zhang X, Yuan H, Duan Y, Wang Z, Zhou Z, Liu L. Serum total folate, 5-methyltetrahydrofolate and Vitamin B12 concentrations on incident risk of lung cancer. Int J Cancer. 2023;152(6):1095–106.
Huo Y, Li J, Qin X, Huang Y, Wang X, Gottesman RF, et al. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT randomized clinical trial. JAMA. 2015;313(13):1325–35.
Marchand LL, Wilkens LR, Kolonel LN, Henderson BE. The MTHFR C677T polymorphism and colorectal cancer the multiethnic cohort study. Cancer Epidemiol Biomark Prev. 2005;14(4):1198–203.
Ma J, Stampfer MJ, Giovannucci E, Artigas C, Hunter DJ, Fuchs C, et al. Methylenetetrahydrofolate reductase polymorphism, dietary interactions, and risk of colorectal cancer. Cancer Res. 1997;57(6):1098–102.
Hubner RA, Houlston RS. MTHFR C677T and colorectal cancer risk: a meta-analysis of 25 populations. Int J Cancer. 2006;120(5):1027–35.
Yin G, Kono S, Toyomura K, Hagiwara T, Nagano J, Mizoue T, et al. MTHFR C677T and A1298C polymorphisms and colorectal cancer: The Fukuoka colorectal cancer study. Cancer Sci. 2004;95(11):908–13.
Tong N, Fang Y, Li J, Wang M, Lu Q, Wang S, et al. Methylenetetrahydrofolate reductase polymorphisms, serum methylenetetrahydrofolate reductase levels, and risk of childhood acute lymphoblastic leukemia in a Chinese population. Cancer Sci. 2010;101(3):782–6.
Yan J, Yin M, Dreyer ZE, Scheurer ME, Kamdar K, Wei Q, et al. A meta-analysis of MTHFR C677T and A1298C polymorphisms and risk of acute lymphoblastic leukemia in children. Pediatr Blood Cancer. 2012;58(4):513–8.
Sailasree R, Nalinakumari KR, Sebastian P, Kannan S. Influence of methylenetetrahydrofolate reductase polymorphisms in oral cancer patients. J Oral Pathol Med. 2011;40(1):61–6.
Safarinejad MR, Shafiei N, Safarinejad S. Relationship between three polymorphisms of methylenetetrahydrofolate reductase (MTHFR C677T, A1298C, and G1793A) gene and risk of prostate cancer: a case–control study. Prostate. 2010;70(15):1645–57.
Zhong S, Yang J, Liu K, Jiao BH, Chang Z. Quantitative assessment of the association between MTHFR C677T polymorphism and colorectal cancer risk in East Asians. Tumor Biol. 2012;33(6):2041–51.
Graziano F, Kawakami K, Ruzzo A, Watanabe G, Santini D, Pizzagalli F, et al. Methylenetetrahydrofolate reductase 677C/T gene polymorphism, gastric cancer susceptibility and genomic DNA hypomethylation in an at-risk Italian population. Int J Cancer. 2006;118(3):628–32.
Lacasaña-Navarro M, Galván-Portillo M, Chen J, López-Cervantes M, López-Carrillo L. Methylenetetrahydrofolate reductase 677C >T polymorphism and gastric cancer susceptibility in Mexico. Eur J Cancer. 2006;42(4):528–33.
Shannon B, Gnanasampanthan S, Beilby J, Iacopetta B. A polymorphism in the methylenetetrahydrofolate reductase gene predisposes to colorectal cancers with microsatellite instability. Gut. 2002;50:520–4.
Derwinger K, Wettergren Y, Odin E, Carlsson G, Gustavsson B. A study of the MTHFR gene polymorphism C677T in colorectal cancer. Clin Colorectal Cancer. 2009;8(1):43–8.
Kim JK, Kim S, Han JH, Kim HJ, Chong SY, Hong SP, et al. Polymorphisms of 5,10-methylenetetrahydrofolate reductase and risk of stomach cancer in a Korean population. Anticancer Res. 2005;25:2249–52.
Vollset SE, Igland J, Jenab M, Fredriksen A, Meyer K, Eussen S, et al. The association of gastric cancer risk with plasma folate, cobalamin, and methylenetetrahydrofolate reductase polymorphisms in the european prospective investigation into cancer and nutrition. Cancer Epidemiol Biomark Prev. 2007;16(11):2416–24.
Suzuki T, Matsuo K, Hasegawa Y, Hiraki A, Wakai K, Hirose K, et al. One-carbon metabolism-related gene polymorphisms and risk of head and neck squamous cell carcinoma: case–control study. Cancer Sci. 2007;98(9):1439–46.
Hekim N, Ergen A, Yaylım I, Yılmaz H, Zeybek Ü, Öztürk O, İsbir T. No association between methylenetetrahydrofolate reductase C677T polymorphism and breast cancer. Cell Biochem Funct. 2007;1:115–7.
Kim Y. Methylenetetrahydrofolate reductase polymorphisms, folate, and cancer risk a paradigm of gene-nutrient interactions in carcinogenesis. Nutr Rev. 2000;58(7):205–9.
Chen J, Giovannucci E, Kelsey K, Rimm EB, Stampfer MJ, Colditz GA, et al. A methylenetetrahydrofolate reductase polymorphism and the risk of colorectal cancer. Cancer Res. 1996;56:4862–4.
Dong X, Wu J, Liang P, Li J, Yuan L, Liu X. Methylenetetrahydrofolate reductase C677T and A1298C polymorphisms and gastric cancer: a meta-analysis. Arch Med Res. 2010;41(2):125–33.
Weisberg I, Tran P, Christensen B, Sibani S, Rozen R. A second genetic polymorphism in methylenetetrahydrofolate reductase (MTHFR) associated with decreased enzyme activity. Mol Genet Metab. 1998;64:169–72.
Blount BC, Mack MM, Wehr CM, Macgregor JT, Hiatt RA, Wang G, et al. Folate deficiency causes uracil misincorporation into human DNA and chromosome breakage: implications for cancer and neuronal damage. Proc Natl Acad Sci USA. 1997;94:3290–5.
Bagley PJ, Selhub J. A common mutation in the methylenetetrahydrofolate reductase gene is associated with an accumulation of formylated tetrahydrofolates in red blood cells. Proc Natl Acad Sci USA. 1998;95:13217–20.
Quinlivan EP, Davis SR, Shelnutt KP, Henderson GN, Ghandour H, Shane B, et al. Methylenetetrahydrofolate reductase 677C→T polymorphism and folate status affect one-carbon incorporation into human DNA deoxynucleosides. J Nutr. 2005;135(3):389–96.
Sohn KJ, Croxford R, Yates Z, Lucock M, Kim YI. Effect of the methylenetetrahydrofolate reductase C677T polymorphism on chemosensitivity of colon and breast cancer cells to 5-fluorouracil and methotrexate. JNCI J Natl Cancer Inst. 2004;96(2):134–44.
Yang B, Fan S, Zhi X, Xia R, Wang Y, Zheng Q, et al. Geographical and ethnic distribution of MTHFR gene polymorphisms and their associations with diseases among Chinese population. Clin Genet. 2017;92(3):243–58.
Meng Y, Liu X, Ma K, Zhang L, Lu M, Zhao M, et al. Association of MTHFR C677T polymorphism and type 2 diabetes mellitus (T2DM) susceptibility. Mol Genet Genom Med. 2019;7(12): e1020.
Qian X, Lu Z, Tan M, Liu H, Lu D. A meta-analysis of association between C677T polymorphism in the methylenetetrahydrofolate reductase gene and hypertension. Eur J Hum Genet. 2007;15(12):1239–45.
Brattströma L, Zhang Y, Hurtig M, Refsum H, Stensson S, Fransson L, et al. A common methylenetetrahydrofolate reductase gene mutation and longevity. Atherosclerosis. 1998;141:315–9.
Acknowledgements
We acknowledge all of the study participants who participated in this project and the contribution of all the staff members who made this study possible. We also thank Ms. Emmy Graham for her valuable suggestions and edits to the manuscript.
Funding
Funding for this project was supported by the National Key Research and Development Program, 2022YFC2009600 and 2022YFC2009601 (to BW). The Guangdong Provincial Key Laboratory of H-type Hypertension and Stroke Precision Prevention Research and Development Enterprise, 2020B121202010 (to XX), the Department of Science and Technology of Guangdong Province, and the Development and Reform Commission of Shenzhen Municipality, XMHT20220104055 (to BW). The National Key Research and Development Program 2018ZX09739010 and 2018ZX09301034003 (to XX); and the Science, Technology and Innovation Committee of Shenzhen, JSGG20180703155802047, JSGG20201103153807021 and KCXFZ20211020163801002 (to XX). The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Author information
Authors and Affiliations
Contributions
QH, XX and YD contributed to the study conception and design; BW, XX, YS, LL, PC, SL and YW contributed to the collection and assembly of the data; Data analysis and interpretation were done by YW, QL, HZ, and QH; QH drafted the manuscript; Manuscript review and editing were carried out by QH, SL, BW and YD. Final approval of the manuscript was given by all authors.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Institute of Biomedicine, Anhui Medical University, Hefei, China.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
He, Q., Wei, Y., Zhu, H. et al. The combined effect of MTHFR C677T and A1298C polymorphisms on the risk of digestive system cancer among a hypertensive population. Discov Onc 15, 97 (2024). https://doi.org/10.1007/s12672-024-00960-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-024-00960-y