Abstract
Prostate cancer is the second incidence of malignant tumors in men worldwide. Its incidence and mortality are increasing year by year. Enhanced expression of Cav1 in prostate cancer has been linked to both proliferation and metastasis of cancer cells, influencing disease progression. Dysregulation of the Cav1 gene shows a notable association with prostate cancer. Nevertheless, there is no systematic review to report about molecular signal mechanism of Cav1 and drug treatment in prostate cancer. This article reviews the structure, physiological and pathological functions of Cav1, the pathogenic signaling pathways involved in prostate cancer, and the current drug treatment of prostate cancer. Cav1 mainly affects the occurrence of prostate cancer through AKT/mTOR, H-RAS/PLCε, CD147/MMPs and other pathways, as well as substance metabolism including lipid metabolism and aerobic glycolysis. Baicalein, simvastatin, triptolide and other drugs can effectively inhibit the growth of prostate cancer. As a biomarker of prostate cancer, Cav1 may provide a potential therapeutic target for the treatment of prostate cancer.
Similar content being viewed by others
1 Introduction
Prostate cancer (PCa) is the most common malignant tumor of the male urinary system. It mainly affects men over 60 years of age. In recent years, as living standards elevate and population aging intensifies, the incidence of PCa has experienced a marked surge, casting a profound impact on the quality of human life [1, 2]. Contemporary radical prostatectomy is predominantly used for treatment paradigms of initial-stage PCa. For more advanced, locally invasive, or metastatic cases of PCa, therapeutic strategies typically pivot towards chemotherapy and androgen-deprivation therapy [3,4,5,6]. To date, the pathogenesis and underlying molecular biology of PCa are inadequately elucidated [7]. Further research into the pathogenesis of PCa is needed to find useful therapeutic approaches.
Cavelin-1 (Cav1) is located on the long arm of chromosome 7, and is localized at the D7S522 locus (7q31.1), which is a fragile site that is easily lost in cancer [8]. It has been found that deletion of the q31 region of chromosome 7 is closely related to PCa progression and death [9]. A large number of literatures have shown that Cav1 is closely related to PCa, which affect the occurrence and development of PCa [3, 10, 11]. Some scholars have found that the main function of secreted Cav1 in the microenvironment of PCa is to promote angiogenesis and cell survival [12]. In PCa, the abnormally expressed Cav1 interacts with AKT and activates specific oncogenic activities, leading to faster progression of PCa, which is not conducive to the treatment of PCa. Drugs such as baicalin [13], simvastatin [14], triptolide [15], and various chemicals such as phenylbutyrate [16], incadronate [17], cholesterol and phytosterols [18] affect Cav1 expression or participate in certain signaling pathways that delay the progression of PCa. Although a large number of drugs have been used to treat PCa, the therapeutic effect of some drugs has decreased year by year, leading to an increase in the recurrence rate of PCa. The mechanism of some drugs needs to require further study.
In this review, we introduce the function and structure of Cav1 and its relationship with clinical parameters, explore the signaling pathways involved in PCa, and how pharmacological regulation of Cav1 expression affects the progression of PCa. This will allow us to further understand the role of Cav1 in PCa and find more therapeutic methods for PCa.
2 Structure and function of Cav1
Caveolin represents a distinct vesicular structure present on the cellular membrane surface, serving as an integral structural and functional protein [19]. The caveolin family comprises three subtypes, including Cav1, Cav2, and Cav3 [20, 21]. Cav1 and Cav2 are widely expressed in normal human cells and tissues. Cav1 exhibits prevalent expression within a diverse array of cell types, including but not limited to vascular endothelial cells, adipose tissue, smooth muscle cells, and stromal cells. Cav3 is specifically expressed in muscle and has been reported in skeletal muscle tissue and cardiomyocytes [22, 23]. The structure and function of Cav1 are further elaborated.
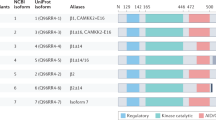
Cav1 is a structural membrane protein with a molecular weight of approximately 21 to 24 kDa. Cav1 is an essential component of the globular invagination of most types of plasma membranes and functions as a scaffold protein for caveolae (Fig. 1C). It is mainly composed of three exons located at 7q31.1 [24], with both N and C terminal facing the cytoplasm. Unlike Cav2 and Cav3, Cav1 has several domains, including tyrosine 14 phosphorylation (residues 1–60) [25], the N-terminal oligomeric domain (residues 61–101) [26, 27], the caveolin scaffold domain (CSD) (residues 82–101) [28], as well as transmembrane domains (residues 82–101) and membrane-spanning domains (residues 135–150) [29] (Fig. 1A). Tyrosine 14 phosphorylation is closely related to the migration and invasion of tumor cells [30]. The residues 61–101 have homologous oligomerization activity and fusion with GST proteins results in GST multimerization [27]. The CSD has the ability to participate in and regulate protein–protein interactions, and it also plays a crucial role in orchestrating the extensive signaling events requisite for endothelial cell recruitment and tumor progression [31]. The polarized structure of Cav1 is also shown [32, 33] (Fig. 1B). Cav1 contains two variants, cav1α (residues 1 to 178) and cav1β (residues 34 to 178) (Fig. 1A), which can be generated by alternative initiation of the same transcript or by alternative transcripts [34,35,36]. Cav1 phosphorylation is thought to be associated with cell migration and metastasis [37]. There are still other domains that need further investigation.
2.1 Physiological functions of Cav1
Cav1 expression in different cells and tissues can produce different physiological functions. Cav1 promotes adipogenesis when secreted by adipose tissue and adipocytes [38]. Cav1 has tumor suppressive and radioresistant effects if expressed in interstitial fibroblasts [33, 39]. Cav1 has been found in mitochondria and caveolin, but it is usually not expressed in the prostate epithelium or is rarely expressed. It is also involved in a variety of cellular processes such as molecular transport, cell transport, cell adhesion, signaling transduction between molecules, cell cycle change, cell endocytosis [20, 40,41,42,43]. Cav1 is also a type II AR coregulator that regulates some cholesterol and steroid receptors, such as estrogen receptors [25]. Cav1 can be secreted into the extracellular environment, which is an exogenous Cav1 and has a promoting effect on the formation of prostate balls. Cav1 regulates the proliferation and differentiation of vascular endothelial cells and is associated with a variety of physiological functions [44,45,46]. When Cav1 is silenced in stromal cells, the production of cholesterol and testosterone are increase [11].
2.2 Pathological function of Cav1
A large number of literature studies have shown that Cav1 is involved in various processes of tumorigenesis, progression, migration and invasion [13, 47, 48]. It has been reported that Cav1 belongs to an anti-apoptotic protein and is related to bcl family [49,50,51]. Cav1 is present in different cell types, tumor stages and locations, and its biological effects may vary. Cav1 may be closely related to the progression of some malignant tumors, such as bladder cancer [52, 53], ovarian cancer [54, 55], lung cancer [56, 57], among which its role in PCa [58, 59] being the most extensively explored. Cav1 expression is different in different types and stages of PCa, which affects the progression of PCa.
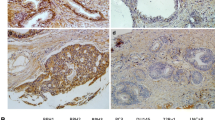
2.3 Relationship between Cav1 Expression and PCa
In PCa, the expression of Cav1 is correlated with clinical stage, pathological characteristics and other clinical parameters. Some studies have found that the Cav1 expression and metastases [14, 60], gleason score [11, 61,62,63,64,65,66,67,68,69,70,71,72], survival rate [10, 11, 14, 64, 69,70,71, 73, 74], clinical stage [10, 72,73,74] and lymph node involvement [68, 70, 75] are correlated. Cav1 expression is not correlated with age [14, 41, 69,70,71, 74,75,76,77]. The relationship between Cav1 and prostate specific antigen (PSA) is controversial, some studies suggest that there is a significant correlation between Cav1 and PSA in castration-resistant prostate cancer (CRPC) [61, 63, 64, 71, 72, 76], but some studies suggest that there is no significant correlation between Cav1 and PSA of difference stage and grade of PCa [14, 41, 69, 70, 73, 74] (Table 1). The relationship between Cav1 and PSA needs to be further studied.
3 Role of Cav1 in PCa
Cav1 is secreted by PCa cells and observed in the serum of PCa patients, showing a trend of positive correlation with tumor stage and grade. Cav1 is an autocrine/paracrine factor that is up-regulated in metastatic PCa, CRPC and androgen insensitive prostate cancer, but not in hormone sensitive prostate cancer [75]. When Cav1 is overexpressed, it will lead to the proliferation of PCa [78, 79]. Cav1 is associated with ID-1 (differentiation and DNA binding inhibitors) in the helix-loop-helix transcription factor family via HLH structure and has implications for EMT and cell survival in PCa [80]. Non-caveolar Cav1 influences the expression of VEGF-A in PCa cells, thereby impacting the proliferation, migration, and invasion of lymphatic endothelial cells. These alterations, in turn, bear significant implications for the prognosis and survival rates associated with PCa. It has been shown that the expression level of Cav1 in stromal is negatively correlated with epithelial Cav1 expression and AKT activation, affecting the metastasis and invasion of PCa.
The regulation of testosterone and various growth factors in PCa patients can affect the expression of Cav1. Testosterone can affect the survival and growth of PCa cells by regulating [81]. Cav1 can regulate androgen-insensitive prostate cancer cells. It has been reported that inhibition of Cav1 expression can change the insensitivity of androgen-insensitive prostate cancer cells to androgen and slow down the progression of PCa [82]. C-myc belongs to an oncogene, it is closely related to PCa, c-myc induces apoptosis of PCa cells, but the increased expression of Cav1 leads to the decreased apoptotic ability of PCa cells [67]. Cav1 can regulate the expression of acetyl-CoA carboxylase-1 (ACC1) and fatty acid synthase (FASN) in the adipose tissue of PCa cells, participate in the synthesis of fatty acid, further regulate the hormone resistance, and affect the progression and resistance of PCa.
4 Cav1 and signal pathway in PCa
Cav1 plays a pivotal role in an array of signaling pathways. It encompasses a compact 20-amino acid domain, which allows for numerous signaling molecules to interact with Cav1 within the caveolin structure [83]. They include protein kinase C isoforms, heterotrimeric G protein subunits, GTP enzymes, endothelial nitric oxide synthase, SRC-associated tyrosine kinases, epidermal growth factor receptor (EGF-R), phospholipase Cγ1 (PLCγ1), integrin β1 (ITGβ1), p53 and integrin-related proteins [32, 34, 84,85,86]. The progression of PCa is affected by multiple signaling pathways. Therefore, we will review the signal pathways of Cav1 involved in PCa (Fig. 2).
4.1 Wnt-β-catenin
Wnt proteins are important components of a family of cysteine-rich secretory ligands that affect growth and development in nematodes and mammals [87]. Wnt-β-catenin can regulate cell proliferation and differentiation, and even lead to tumor formation. Cav1 can activate the Wnt-β-catenin pathway and induce internalization of low-density lipoprotein receptor-associated protein 6 (LRP6) [88]. Within the context of PCa, Cav1 assumes a pivotal role in lipid anabolism, particularly in the sphere of lipid synthesis. The regulation of lipid metabolism is an important factor in tumorigenesis. Cav1 can regulate the phosphorylation of LRP6 in PCa, and the interaction between them affects the Wnt-β-Catenin signaling pathway, which in turn affects the phosphorylation of IGF-1R/IR, activates the insulin/IGF-1R pathway, and indirectly affects aerobic glycolysis [89]. Therefore, altering Cav1 expression in human body can affect the lipid anabolic process mediated by Wnt-β-catenin signaling pathway, thereby slowing the progression of PCa.
4.2 PI3K-AKT-eNOS
In PCa, Cav1 fosters cell migration, tubule formation, and nitric oxide production by modulating the PI3K-AKT-eNOS signaling pathway. [90]. Cav1 is able to stimulate angiogenic activity mainly due to CSD mediated. The CSD is where many signaling proteins interact [91]. The expression of Cav1 increases vascular endothelial growth factor by activating AKT phosphorylation, which promotes the proliferation of endothelial cells and is of great significance for angiogenesis [92, 93]. PP1 and PP2A belong to serine/threonine protein phosphatases, and they are closely associated with the phosphorylation of AKT and eNOS [94]. Cav1 overexpression inhibits PP1/PP2A expression, leading to phosphorylation of AKT and eNOS [95]. The combined effect of eNOS and NO affects the migration ability of PCa [96]. Cav1 can stimulate the angiogenesis of PCa through the P13K-AKT-eNOS signaling pathway, which leads to PCa more likely to metastasize.
4.3 ACC1-FASN
In PCa, Cav1 expression was significantly positively correlated with ACC1 and FASN expression, further indicating that Cav1 is involved in the process of fatty acid synthesis [97]. The effects of CD36 and ACC1/FASN are similar. CD36 belongs to the fatty acid translocase, which transports cholesterol and long-chain fatty acids across the plasma membrane. Cav1 interacts with CD36 and affects lipid synthesis, thereby affecting tumor metastasis [90]. Cav1 can interact with ACC1 and FASN to affect the growth of PCa cells. FASN and ACC1 are closely related to fatty acid synthesis [98, 99]. FASN belongs to the relatively large homodimeric enzymes [100]. It produces long-chain fatty acids. Cav1 can alter the RNA expression of ACC1 and FASN and promote palmitic acid synthesis, and FASN/Cav1 interacts to make Cav1 palmitoylated [101]. The signal pathway was supported by that overexpression of Cav1 in PCa promotes ACC1-FASN expression, leading to lipid synthesis and further promoting hormone resistance [102], which can lead to decreased efficacy of hormone therapy and affect the survival of PCa.
4.4 Acid sphingomyelinase (ASMase)/ceramide
The acid sphingosine hydrolase (ASMase)/ Ceramide pathway plays a crucial role in the radiation resistance of cancer cells and radiation-induced endothelial cell (EC) apoptosis. ASMase is highly expressed in EC, which may indicate that EC is sensitive to radiation-induced apoptosis [103, 104]. Cav1 regulates the ASMase/Ceramide mediated ionizing radiation response [105]. Ionizing radiation has some effect on the raft microdomain [106, 107] of cytoplasmic membrane organization. High-dose ionizing radiation can increase membrane ceramide content through the ASMase-Ceramide pathway. When Cav1 is deficient in endothelial cells, membrane signalers are increased, which can affect the downstream targets P38 and AKT [108] and ultimately lead to EC apoptosis. Thus, Cav1 can regulate ceramide-dependent plasma membrane organization. Ceramide-dependent plasma membrane architecture can in turn influence the radiation response of EC and adjacent PCa cells, so as to play a role in the treatment of PCa.
4.5 TF/FVIIa/IGF1R
Tissue factor (TF) is a transmembrane protein and a promoter of blood coagulation. TF is able to bind factor VII (FVII) and FVIIa to form a TF/FVIIa complex [109]. IGF-1R belongs to the transmembrane receptor tyrosine kinase [110], which mainly regulates cell proliferation, apoptosis and migration. IGF-1 binds to IGF-1 receptor (IGF-1R) and IR to activate the migration pathway of PCa, which may lead to the lethal development of PCa. Both TF and IGF-1R are able to bind CSD [111]. The CSD of Cav1 regulates FVIIa-induced phosphorylation of IGF-1R. TF/FVIIa induces the phosphorylation of Cav1 tyrosine 14 via β1 integrin. In PCa, Cav1 and β1 integrins play a role in the anti-apoptotic signaling of TF/FVIIa/IGF1R [109].
4.6 H-RAS/ PLCε
Phosphatidylinositol-specific phospholipase Cε (PLCε) is a member of the human phosphatidylinositol-PLC family. In contrast to other phospholipase Cε isoforms, PLCε has a domain of a GTPase nucleotide exchange factor that can be used to activate Ras family GTPases, but it also is regulated by RAS family GTP [112]. RAS is the most frequently mutated gene family in cancer, and H-RAS belongs to RAS family. PLCε expression is increased in urologic tumors, and it promotes AR nuclear translocation in PCa [113]. The expression of H-RAS and PLCε is positively correlated with Cav1. PLCε regulates CRPC invasion and migration in metastatic CRPC. When Cav1 expression is reduced, it can reduce PLCε expression through H-RAS, thereby inhibiting CRPC invasion and migration [14]. Further studies on Cav1 inhibitors targeting the Cav1/H-RAS/PLCε pathway is needed to slow the progression of CRPC.
5 Targeting Cav1 signaling pathway in PCa therapy
So far, a large number of drugs such as baicalein, simvastatin, triptolide and some chemicals have been used to treat PCa. These drugs mainly affect some signaling pathways involved in Cav1 to treat PCa (Table 2). We further explored the specific effects of these drugs.
5.1 Baicalein
Scutellaria is an herb and baicalein can be extracted from the root of Scutellaria. Baicalein is a bioactive flavonoid that has been shown to treat hypertension, infectious diseases, inflammation, and cardiovascular diseases [116]. Most importantly, baicalein has anti-tumor effects on cancer cells [117], and it is able to inhibit the anti-apoptotic ability of Cav1 [118]. Baicalein inhibited the activation and phosphorylation of AKT. The downstream product of AKT is mTOR, and phosphorylated mTOR is able to promote cancer cell proliferation, migration, and invasion [119]. The anticancer effect of baicalein was enhanced when AKT expression was inhibited. Therefore, baicalein may inhibit the occurrence and development of androgen-independent prostate cancer through the Cav1/AKT/mTOR pathway [13]. Baicalein can still be used as a drug for the treatment of androgen-independent prostate cancer and improve the survival rate.
5.2 Simvastatin
Simvastatin is an inhibitor of Hydroxymethylglutaryl Coenzyme A (HMG-CoA) reductase, which plays a role in the conversion of HMG-CoA to mevalonate and prevents cholesterol biosynthesis [120]. Cav1 is involved in cholesterol regulation, and it can directly bind to cholesterol to form caveolin [121]. Cav1 is highly expressed in metastatic CRPC. Simvastatin can regulate the expression of Cav1 and inhibit the migration of CRPC through H-RAS/PLCε pathway. It has been shown that simvastatin inhibits de novo cholesterol synthesis in CRPC cells and inhibits Cav-1 expression, which further enhances the anticancer effect of androgen receptor antagonists [14]. Inhibition of Cav1 expression or cholesterol synthesis by simvastatin combined with some drugs may still be a therapeutic strategy for CRPC.
5.3 Triptolide
Triptolide is mainly extracted from a medicinal plant, tripterygium wilfordii, which is a diterpene trioxide. It has the functions of resisting inflammation, immunosuppression and promoting apoptosis. Triptolide can inhibit the migration and invasion of PCa cells through the Cav1/CD147/MMPs pathway [15]. CD147, a member of the immunoglobulin superfamily, plays a critical role in numerous processes including the secretion of matrix metalloproteinases (MMPs), intercellular communication, and the invasion and migration of tumor cells [122, 123]. CD147 exhibits a high degree of specificity in binding to the 39-amino acid domains of Cav1. This interaction with MMPs exerts a significant influence on the process of tumor invasion [124]. Triptolide can down-regulate the expression of Cav-1, CD147 and MMPs to inhibit the migration and invasion of PCa cells. In the future, the combination of Cav1 inhibitor and triptolide may more effective treatment of aggressive PCa.
5.4 Dasatinib and sunitinib
Dasatinib, an oral agent capable of activating the Bcr-Abl enzyme and inhibiting the Src family kinase (SFK) protein [125, 126], inhibits the proliferation and migration of PCa cells. Sunitinib (SU11248) operates as a receptor tyrosine kinase (RTK) inhibitor that targets vascular endothelial growth factor (VEGF), exhibiting both antiangiogenic and antitumor properties [127, 128]. In PCa, Cav1 is overexpressed, leading to PCa cells proliferation and migration. Studies have shown that dasatinib and sunitinib affect Cav1 expression by inhibiting RTK/TK signaling activity in PCa cells. Dasatinib and sunitinib combined with anti-Cav1 antibody can significantly inhibit the proliferation and migration of PCa cells [115]. This will provide us with a new way to combine drugs with anti-Cav1 antibodies in the treatment of PCa.
5.5 Other chemical reagents
Phenylbutyrate (PB), characterized as a short-chain fatty acid, acts through the inhibition of histone deacetylase activity [16]. It is capable of inducing the differentiation and apoptosis of PCa cells [129, 130]. It has been found that PB can inhibit the expression of Cav1 in PCa cell, leading to a decrease in the invasive ability of PCa cells. Incadronate is a third-generation bisphosphonate. It inhibits the expression of Cav1 by inhibiting key enzymes in isoprenoid biosynthesis pathway and affects the progression of PCa [17]. ProstaCaid (PC) is a dietary supplement consisting of 33 Chinese herbs and nutrients, including ganoderma lucidum, resveratrol, epigallocatechin-3-gallate, vitamin D3 [114], etc. Vitamin D3 can down-regulate Cav1 expression, inhibit MMP-9 activity, and affect cell cycle changes. The common feature of these drugs is their ability to affect Cav1 expression, which in turn hinders the progression of PCa.
6 Conclusion
In this review, structure, the signaling pathways and therapeutic drugs involved in Cav1 are summarized, mainly to provide theoretical basis for better treatment of PCa. Its unstable location and CSD domain make Cav1 play a critical role in PCa. Cav1 indirectly affects lipid anabolic processes in Wnt-β-catenin pathway and glycolytic pathway through insulin/IGF-IR pathway. Cav1 can affect tumor angiogenesis through PI3K-AKT-eNOS. The activation of ACC1-FASN pathway leads to hormone resistance of PCa cells and is not conducive to hormone therapy of PCa. Cav1 affects the expression of ceramide in the ASMase/ceramide pathway, thereby affecting the sensitivity of PCa cells to radiotherapy and reducing the effect of radiotherapy. The TF/FVIIa/IGF1R pathway has an anti-apoptotic effect, and TF/FVIIa activates Cav1 and β-1 integrin and affects the expression of IGF1R. These signaling pathways are not conducive to the treatment and prognosis of PCa. Therapeutic agents such as baicalin, simvastatin, triptolide, prostacaid, dasatinib, and sunitinib have been leveraged in PCa treatment, influencing the signaling pathways implicated in Cav1 regulation. In order to improve the survival rate of PCa patients, the pathway of Cav1 involved in PCa still needs to be further studied.
7 Future perspectives
Taken together, Cav1 serves a crucial function in the molecular mechanism of PCa. The role of Cav1 in modulating multiple signaling pathways in PCa holds substantial significance for therapeutic strategies. ACC1-FASN, Tf/FVIIa/IGF-1R/IR and AKT signal pathways might be potential pathways in the treatment of PCa. The utilization of novel nanotechnology to combine chemical drugs like phenylbutyric acid and incadronate, or anti-Cav1 antibody, with PCa drugs such as baicalein and triptolide, holds potential for a new direction in PCa treatment. More research could be focused on the molecular mechanism of Cav1 and drug therapy in PCa.
Data availability
Not applicable.
Code availability
Not applicable.
References
Wong ECL, Kapoor A. Epidemiology of prostate and kidney cancer in the Aboriginal population of Canada: A systematic review. Can Urol Assoc J. 2017;11(5):E222–32.
Trama A, Botta L, Nicolai N, Rossi PG, Contiero P, Fusco M, et al. Prostate cancer changes in clinical presentation and treatments in two decades: an Italian population-based study. Eur J Cancer. 2016;67:91–8.
Kamibeppu T, Yamasaki K, Nakahara K, Nagai T, Terada N, Tsukino H, et al. Caveolin-1 and -2 regulate cell motility in castration-resistant prostate cancer. Res Rep Urol. 2018;10:135–44.
Swami U, McFarland TR, Nussenzveig R, Agarwal N. Advanced prostate cancer: treatment advances and future directions. Trends in Cancer. 2020;6(8):702–15.
Achard V, Putora PM, Omlin A, Zilli T, Fischer S. Metastatic prostate cancer: treatment options. Oncology. 2022;100(1):48–59.
Yamada Y, Beltran H. The treatment landscape of metastatic prostate cancer. Cancer Lett. 2021;519:20–9.
Terada N, Akamatsu S, Kobayashi T, Inoue T, Ogawa O, Antonarakis ES. Prognostic and predictive biomarkers in prostate cancer: latest evidence and clinical implications. Ther Adv Med Oncol. 2017;9(8):565–73.
Engelman JA, Zhang XL, Lisanti MP. Genes encoding human caveolin-1 and -2 are co-localized to the D7S522 locus (7q31.1), a known fragile site (FRA7G) that is frequently deleted in human cancers. FEBS Lett. 1998;436(3):403–10.
Jenkins R, Takahashi S, DeLacey K, Bergstralh E, Lieber M. Prognostic significance of allelic imbalance of chromosome arms 7q, 8p, 16q, and 18q in stage T3N0M0 prostate cancer. Genes Chromosomes Cancer. 1998;21(2):131–43.
Nassar ZD, Hill MM, Parton RG, Francois M, Parat MO. Non-caveolar caveolin-1 expression in prostate cancer cells promotes lymphangiogenesis. Oncoscience. 2015;2(7):635–45.
Ayala G, Morello M, Frolov A, You S, Li R, Rosati F, et al. Loss of caveolin-1 in prostate cancer stroma correlates with reduced relapse-free survival and is functionally relevant to tumour progression. J Pathol. 2013;231(1):77–87.
Thompson TC, Tahir SA, Li L, Watanabe M, Naruishi K, Yang G, et al. The role of caveolin-1 in prostate cancer: clinical implications. Prostate Cancer Prostatic Dis. 2009;13(1):6–11.
Guo Z, Hu X, Xing Z, Xing R, Lv R, Cheng X, et al. Baicalein inhibits prostate cancer cell growth and metastasis via the caveolin-1/AKT/mTOR pathway. Mol Cell Biochem. 2015;406(1–2):111–9.
Gao Y, Li L, Li T, Ma L, Yuan M, Sun W, et al. Simvastatin delays castration-resistant prostate cancer metastasis and androgen receptor antagonist resistance by regulating the expression of caveolin-1. Int J Oncol. 2019;54(6):2054–68.
Yuan S, Wang L, Chen X, Fan B, Yuan Q, Zhang H, et al. Triptolide inhibits the migration and invasion of human prostate cancer cells via Caveolin-1/CD147/MMPs pathway. Biomed Pharmacother. 2016;84:1776–82.
Goh M, Chen F, Paulsen MT, Yeager AM, Dyer ES, Ljungman M. Phenylbutyrate attenuates the expression of Bcl-X (L), DNA-PK, caveolin-1, and VEGF in prostate cancer cells. Neoplasia. 2001;3(4):331–8.
Iguchi K, Matsunaga S, Nakano T, Usui S, Hirano K. Inhibition of caveolin-1 expression by incadronate in PC-3 prostate cells. Anticancer Res. 2006;26(4B):2977–81.
Ifere GO, Equan A, Gordon K, Nagappan P, Igietseme JU, Ananaba GA. Cholesterol and phytosterols differentially regulate the expression of caveolin 1 and a downstream prostate cell growth-suppressor gene. Cancer Epidemiol. 2010;34(4):461–71.
Wang X, Liu Z, Yang Z. Expression and clinical significance of Caveolin-1 in prostate cancer after transurethral surgery. BMC Urol. 2018;18(1):102.
Williams TM, Lisanti MP. The caveolin proteins. Genome Biol. 2004;5(3):214.
Scherer PE, Okamoto T, Chun M, Nishimoto I, Lodish HF, Lisanti MP. Identification, sequence, and expression of caveolin-2 defines a caveolin gene family. Proc Natl Acad Sci USA. 1996;93(1):131–5.
Fridolfsson HN, Roth DM, Insel PA, Patel HH. Regulation of intracellular signaling and function by caveolin. FASEB J. 2014;28(9):3823–31.
Sonnino S, Prinetti A. Sphingolipids and membrane environments for caveolin. FEBS Lett. 2009;583(4):597–606.
Wu HC, Chang CH, Tsou YA, Tsai CW, Lin CC, Bau DT. Significant association of caveolin-1 (CAV1) genotypes with prostate cancer susceptibility in Taiwan. Anticancer Res. 2011;31(2):745–9.
Bennett N, Hooper JD, Lee CS, Gobe GC. Androgen receptor and caveolin-1 in prostate cancer. IUBMB Life. 2009;61(10):961–70.
Song KS, Tang Z, Li S, Lisanti MP. Mutational analysis of the properties of caveolin-1. A novel role for the C-terminal domain in mediating homo-typic caveolin-caveolin interactions. J Biol Chem. 1997;272(7):4398–403.
Sargiacomo M, Scherer PE, Tang Z, Kubler E, Song KS, Sanders MC, et al. Oligomeric structure of caveolin: implications for caveolae membrane organization. Proc Natl Acad Sci USA. 1995;92(20):9407–11.
Schlegel A, Schwab RB, Scherer PE, Lisanti MP. A role for the caveolin scaffolding domain in mediating the membrane attachment of caveolin-1. The caveolin scaffolding domain is both necessary and sufficient for membrane binding in vitro. J Biol Chem. 1999;274(32):22660–7.
Woodman SE, Schlegel A, Cohen AW, Lisanti MP. Mutational analysis identifies a short atypical membrane attachment sequence (KYWFYR) within caveolin-1. Biochemistry. 2002;41(11):3790–5.
Wong TH, Dickson FH, Timmins LR, Nabi IR. Tyrosine phosphorylation of tumor cell caveolin-1: impact on cancer progression. Cancer Metastasis Rev. 2020;39(2):455–69.
Bernatchez P. Endothelial caveolin and its scaffolding domain in cancer. Cancer Metastasis Rev. 2020;39(2):471–83.
Sotgia F, Martinez-Outschoorn UE, Howell A, Pestell RG, Pavlides S, Lisanti MP. Caveolin-1 and cancer metabolism in the tumor microenvironment: markers, models, and mechanisms. Annu Rev Pathol. 2012;7:423–67.
Ketteler J, Klein D. Caveolin-1, cancer and therapy resistance. Int J Cancer. 2018;143(9):2092–104.
Okamoto T, Schlegel A, Scherer PE, Lisanti MP. Caveolins, a family of scaffolding proteins for organizing “preassembled signaling complexes” at the plasma membrane. J Biol Chem. 1998;273(10):5419–22.
Kogo H, Aiba T, Fujimoto T. Cell type-specific occurrence of caveolin-1alpha and -1beta in the lung caused by expression of distinct mRNAs. J Biol Chem. 2004;279(24):25574–81.
Shajahan AN, Dobbin ZC, Hickman FE, Dakshanamurthy S, Clarke R. Tyrosine-phosphorylated caveolin-1 (Tyr-14) increases sensitivity to paclitaxel by inhibiting BCL2 and BCLxL proteins via c-Jun N-terminal kinase (JNK). J Biol Chem. 2012;287(21):17682–92.
Quest AF, Lobos-Gonzalez L, Nunez S, Sanhueza C, Fernandez JG, Aguirre A, et al. The caveolin-1 connection to cell death and survival. Curr Mol Med. 2013;13(2):266–81.
Chang CC, Chen CY, Wen HC, Huang CY, Hung MS, Lu HC, et al. Caveolin-1 secreted from adipose tissues and adipocytes functions as an adipogenesis enhancer. Obesity. 2017;25(11):1932–40.
Panic A, Ketteler J, Reis H, Sak A, Herskind C, Maier P, et al. Progression-related loss of stromal Caveolin 1 levels fosters the growth of human PC3 xenografts and mediates radiation resistance. Sci Rep. 2017;7:41138.
Sternberg PW, Schmid SL. Caveolin, cholesterol and Ras signalling. Nat Cell Biol. 1999;1(2):E35–7.
Sugie S, Tsukino H, Yamauchi T, Mukai S, Fujii M, Shibata N, et al. Functional polymorphism in the CAV1 T29107A gene and its association with prostate cancer risk among Japanese men. Anticancer Res. 2013;33(3):1023–7.
Corn PG, Thompson TC. Identification of a novel prostate cancer biomarker, caveolin-1: Implications and potential clinical benefit. Cancer Manag Res. 2010;2:111–22.
Yang G, Goltsov AA, Ren C, Kurosaka S, Edamura K, Logothetis R, et al. Caveolin-1 upregulation contributes to c-Myc–induced high-grade prostatic intraepithelial neoplasia and prostate cancer. Mol Cancer Res. 2012;10(2):218–29.
Carver LA, Schnitzer JE. Caveolae: mining little caves for new cancer targets. Nat Rev Cancer. 2003;3(8):571–81.
Massimino ML, Griffoni C, Spisni E, Toni M, Tomasi V. Involvement of caveolae and caveolae-like domains in signalling, cell survival and angiogenesis. Cell Signal. 2002;14(2):93–8.
Frank PG, Woodman SE, Park DS, Lisanti MP. Caveolin, caveolae, and endothelial cell function. Arterioscler Thromb Vasc Biol. 2003;23(7):1161–8.
Ng L, Wong SK, Huang Z, Lam CS, Chow AK, Foo DC, et al. CD26 induces colorectal cancer angiogenesis and metastasis through CAV1/MMP1 signaling. Int J Mol Sci. 2022;23(3):1181.
Shi F, Chen X, Wang Y, Xie Y, Zhong J, Su K, et al. HOTAIR/miR-203/CAV1 crosstalk influences proliferation, migration, and invasion in the breast cancer cell. Int J Mol Sci. 2022;23(19):11755.
Linge A, Weinhold K, Blasche R, Kasper M, Barth K. Downregulation of caveolin-1 affects bleomycin-induced growth arrest and cellular senescence in A549 cells. Int J Biochem Cell Biol. 2007;39(10):1964–74.
Yu Q. Restoring p53-mediated apoptosis in cancer cells: new opportunities for cancer therapy. Drug Resist Updat. 2006;9(1–2):19–25.
Zou H, Volonte D, Galbiati F. Interaction of caveolin-1 with Ku70 inhibits Bax-mediated apoptosis. PLoS ONE. 2012;7(6): e39379.
Zhou W, He L, Dai Y, Zhang Y, Wang J, Liu B. MicroRNA-124 inhibits cell proliferation, invasion and migration by targeting CAV1 in bladder cancer. Exp Ther Med. 2022;23(4):312.
Raja SA, Shah STA, Tariq A, Bibi N, Sughra K, Yousuf A, et al. Caveolin-1 and dynamin-2 overexpression is associated with the progression of bladder cancer. Oncol Lett. 2019;18(1):219–26.
Liu B, Zhang J, Yang D. miR-96-5p promotes the proliferation and migration of ovarian cancer cells by suppressing Caveolae1. J Ovarian Res. 2019;12(1):57.
Yang L, Wu H, Zhu Y, Chen X, Chen Y. Plasma exosomal caveolin-1 predicts Poor Prognosis in Ovarian Cancer. J Cancer. 2021;12(16):5005–12.
Leiser D, Samanta S, Eley J, Strauss J, Creed M, Kingsbury T, et al. Role of caveolin-1 as a biomarker for radiation resistance and tumor aggression in lung cancer. PLoS ONE. 2021;16(11): e0258951.
Shi YB, Li J, Lai XN, Jiang R, Zhao RC, Xiong LX. Multifaceted roles of Caveolin-1 in lung cancer: a new investigation focused on tumor occurrence, development and therapy. Cancers. 2020;12(2):291.
Ariotti N, Wu Y, Okano S, Gambin Y, Follett J, Rae J, et al. An inverted CAV1 (caveolin 1) topology defines novel autophagy-dependent exosome secretion from prostate cancer cells. Autophagy. 2021;17(9):2200–16.
Gould ML. The intertwining roles of caveolin, oxytocin receptor, and the associated signalling pathways in prostate cancer progression. Reprod Fertil Dev. 2023;35(9):493–503.
Tahir SA, Yang G, Ebara S, Timme TL, Satoh T, Li L, et al. Secreted caveolin-1 stimulates cell survival/clonal growth and contributes to metastasis in androgen-insensitive prostate cancer. Cancer Res. 2001;61(10):3882–5.
Aliyari M, Elieh Ali Komi D, Kiani A, Moradi M, Tanhapour M, Rahimi Z, et al. The role of caveolin-1 and endothelial nitric oxide synthase polymorphisms in susceptibility to prostate cancer. Int J Exp Pathol. 2021;102(6):260–7.
Basourakos SP, Davis JW, Chapin BF, Ward JF, Pettaway CA, Pisters LL, et al. Baseline and longitudinal plasma caveolin-1 level as a biomarker in active surveillance for early-stage prostate cancer. BJU Int. 2018;121(1):69–76.
Gumulec J, Sochor J, Hlavna M, Sztalmachova M, Krizkova S, Babula P, et al. Caveolin-1 as a potential high-risk prostate cancer biomarker. Oncol Rep. 2012;27(3):831–41.
Karam JA, Lotan Y, Roehrborn CG, Ashfaq R, Karakiewicz PI, Shariat SF. Caveolin-1 overexpression is associated with aggressive prostate cancer recurrence. Prostate. 2007;67(6):614–22.
Di Vizio D, Morello M, Sotgia F, Pestell RG, Freeman MR, Lisanti MP. An absence of stromal caveolin-1 is associated with advanced prostate cancer, metastatic disease and epithelial Akt activation. Cell Cycle. 2009;8(15):2420–4.
Steiner I, Jung K, Miller K, Stephan C, Erbersdobler A. Expression of endothelial factors in prostate cancer: a possible role of caveolin-1 for tumour progression. Oncol Rep. 2012;27(2):389–95.
Yang G, Timme TL, Frolov A, Wheeler TM, Thompson TC. Combined c-Myc and caveolin-1 expression in human prostate carcinoma predicts prostate carcinoma progression. Cancer. 2005;103(6):1186–94.
Hammarsten P, Dahl Scherdin T, Hagglof C, Andersson P, Wikstrom P, Stattin P, et al. High Caveolin-1 expression in tumor stroma is associated with a favourable outcome in prostate cancer patients managed by watchful waiting. PLoS ONE. 2016;11(10): e0164016.
Yang G, Truong LD, Wheeler TM, Thompson TC. Caveolin-1 expression in clinically confined human prostate cancer: a novel prognostic marker. Cancer Res. 1999;59(22):5719–23.
Mathieu R, Klatte T, Lucca I, Mbeutcha A, Seitz C, Karakiewicz PI, et al. Prognostic value of Caveolin-1 in patients treated with radical prostatectomy: a multicentric validation study. BJU Int. 2016;118(2):243–9.
Shephard AP, Giles P, Mbengue M, Alraies A, Spary LK, Kynaston H, et al. Stroma-derived extracellular vesicle mRNA signatures inform histological nature of prostate cancer. J Extracell Vesicles. 2021;10(12): e12150.
Sugie S, Mukai S, Yamasaki K, Kamibeppu T, Tsukino H, Kamoto T. Significant association of Caveolin-1 and Caveolin-2 with prostate cancer progression. Cancer Genom Proteom. 2015;12(6):391–6.
Skara L, Vodopic T, Pezelj I, Abramovic I, Vrhovec B, Vrtaric A, et al. Methylation pattern of caveolin-1 in prostate cancer as potential cfDNA biomarker. Biomol Biomed. 2023;23(1):176–86.
Tahir SA, Frolov A, Hayes TG, Mims MP, Miles BJ, Lerner SP, et al. Preoperative serum caveolin-1 as a prognostic marker for recurrence in a radical prostatectomy cohort. Clin Cancer Res. 2006;12(16):4872–5.
Sugie S, Mukai S, Tsukino H, Toda Y, Yamauchi T, Nishikata I, et al. Increased plasma caveolin-1 levels are associated with progression of prostate cancer among Japanese men. Anticancer Res. 2013;33(5):1893–7.
Yang B, Etheridge T, McCormick J, Schultz A, Khemees TA, Damaschke N, et al. Validation of an epigenetic field of susceptibility to detect significant prostate cancer from non-tumor biopsies. Clin Epigenetics. 2019;11(1):168.
Yang G, Addai J, Ittmann M, Wheeler TM, Thompson TC. Elevated caveolin-1 levels in African-American versus white-American prostate cancer. Clin Cancer Res. 2000;6(9):3430–3.
Yang G, Park S, Cao G, Goltsov A, Ren C, Truong LD, et al. MMTV promoter-regulated caveolin-1 overexpression yields defective parenchymal epithelia in multiple exocrine organs of transgenic mice. Exp Mol Pathol. 2010;89(1):9–19.
Bryant KG, Camacho J, Jasmin JF, Wang C, Addya S, Casimiro MC, et al. Caveolin-1 overexpression enhances androgen-dependent growth and proliferation in the mouse prostate. Int J Biochem Cell Biol. 2011;43(9):1318–29.
Zhang X, Ling MT, Wang Q, Lau CK, Leung SCL, Lee TK, et al. Identification of a novel inhibitor of differentiation-1 (ID-1) binding partner, caveolin-1, and its role in epithelial-mesenchymal transition and resistance to apoptosis in prostate cancer cells. J Biol Chem. 2007;282(46):33284–94.
Li L, Yang G, Ebara S, Satoh T, Nasu Y, Timme TL, et al. Caveolin-1 mediates testosterone-stimulated survival/clonal growth and promotes metastatic activities in prostate cancer cells. Cancer Res. 2001;61(11):4386–92.
Nasu Y, Timme TL, Yang G, Bangma CH, Li L, Ren C, et al. Suppression of caveolin expression induces androgen sensitivity in metastatic androgen-insensitive mouse prostate cancer cells. Nat Med. 1998;4(9):1062–4.
Daniel EE, El-Yazbi A, Cho WJ. Caveolae and calcium handling, a review and a hypothesis. J Cell Mol Med. 2006;10(2):529–44.
Parton RG, Hanzal-Bayer M, Hancock JF. Biogenesis of caveolae: a structural model for caveolin-induced domain formation. J Cell Sci. 2006;119(Pt 5):787–96.
Razani B, Woodman SE, Lisanti MP. Caveolae: from cell biology to animal physiology. Pharmacol Rev. 2002;54(3):431–67.
Couet J, Belanger MM, Roussel E, Drolet MC. Cell biology of caveolae and caveolin. Adv Drug Deliv Rev. 2001;49(3):223–35.
Wodarz A, Nusse R. Mechanisms of Wnt signaling in development. Annu Rev Cell Dev Biol. 1998;14:59–88.
Yamamoto H, Komekado H, Kikuchi A. Caveolin is necessary for Wnt-3a-dependent internalization of LRP6 and accumulation of beta-catenin. Dev Cell. 2006;11(2):213–23.
Tahir SA, Yang G, Goltsov A, Song KD, Ren C, Wang J, et al. Caveolin-1-LRP6 signaling module stimulates aerobic glycolysis in prostate cancer. Cancer Res. 2013;73(6):1900–11.
Rupert JE, Kolonin MG. Fatty acid translocase: a culprit of lipid metabolism dysfunction in disease. Immunometabolism. 2022;4(3): e00001.
Smart EJ, Graf GA, McNiven MA, Sessa WC, Engelman JA, Scherer PE, et al. Caveolins, liquid-ordered domains, and signal transduction. Mol Cell Biol. 1999;19(11):7289–304.
Ferrara N. VEGF and the quest for tumour angiogenesis factors. Nat Rev Cancer. 2002;2(10):795–803.
Breen EC. VEGF in biological control. J Cell Biochem. 2007;102(6):1358–67.
Michell BJ, Chen Z, Tiganis T, Stapleton D, Katsis F, Power DA, et al. Coordinated control of endothelial nitric-oxide synthase phosphorylation by protein kinase C and the cAMP-dependent protein kinase. J Biol Chem. 2001;276(21):17625–8.
Li L, Ren CH, Tahir SA, Ren C, Thompson TC. Caveolin-1 maintains activated Akt in prostate cancer cells through scaffolding domain binding site interactions with and inhibition of serine/threonine protein phosphatases PP1 and PP2A. Mol Cell Biol. 2003;23(24):9389–404.
Gao W, Wang Y, Yu S, Wang Z, Ma T, Chan AM, et al. Endothelial nitric oxide synthase (eNOS)-NO signaling axis functions to promote the growth of prostate cancer stem-like cells. Stem Cell Res Ther. 2022;13(1):188.
Fernandez-Real JM, Catalan V, Moreno-Navarrete JM, Gomez-Ambrosi J, Ortega FJ, Rodriguez-Hermosa JI, et al. Study of caveolin-1 gene expression in whole adipose tissue and its subfractions and during differentiation of human adipocytes. Nutr Metab. 2010;7:20.
Massie CE, Lynch A, Ramos-Montoya A, Boren J, Stark R, Fazli L, et al. The androgen receptor fuels prostate cancer by regulating central metabolism and biosynthesis. EMBO J. 2011;30(13):2719–33.
Moon JS, Jin WJ, Kwak JH, Kim HJ, Yun MJ, Kim JW, et al. Androgen stimulates glycolysis for de novo lipid synthesis by increasing the activities of hexokinase 2 and 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase 2 in prostate cancer cells. Biochem J. 2011;433(1):225–33.
Maier T, Jenni S, Ban N. Architecture of mammalian fatty acid synthase at 4.5 a resolution. Science. 2006;311(5765):1258–62.
Di Vizio D, Adam RM, Kim J, Kim R, Sotgia F, Williams T, et al. Caveolin-1 interacts with a lipid raft-associated population of fatty acid synthase. Cell Cycle. 2008;7(14):2257–67.
Karantanos T, Karanika S, Wang J, Yang G, Dobashi M, Park S, et al. Caveolin-1 regulates hormone resistance through lipid synthesis, creating novel therapeutic opportunities for castration-resistant prostate cancer. Oncotarget. 2016;7(29):46321–34.
Niaudet C, Bonnaud S, Guillonneau M, Gouard S, Gaugler MH, Dutoit S, et al. Plasma membrane reorganization links acid sphingomyelinase/ceramide to p38 MAPK pathways in endothelial cells apoptosis. Cell Signal. 2017;33:10–21.
Haimovitz-Friedman A, Kan CC, Ehleiter D, Persaud RS, McLoughlin M, Fuks Z, et al. Ionizing radiation acts on cellular membranes to generate ceramide and initiate apoptosis. J Exp Med. 1994;180(2):525–35.
Ketteler J, Wittka A, Leonetti D, Roy VV, Estephan H, Maier P, et al. Caveolin-1 regulates the ASMase/ceramide-mediated radiation response of endothelial cells in the context of tumor-stroma interactions. Cell Death Dis. 2020;11(4):228.
Pouget JP, Georgakilas AG, Ravanat JL. Targeted and off-target (Bystander and Abscopal) effects of radiation therapy: redox mechanisms and risk/benefit analysis. Antioxid Redox Signal. 2018;29(15):1447–87.
Stancevic B, Kolesnick R. Ceramide-rich platforms in transmembrane signaling. FEBS Lett. 2010;584(9):1728–40.
Corre I, Paris F, Huot J. The p38 pathway, a major pleiotropic cascade that transduces stress and metastatic signals in endothelial cells. Oncotarget. 2017;8(33):55684–714.
Aberg M, Eden D, Siegbahn A. Activation of beta1 integrins and caveolin-1 by TF/FVIIa promotes IGF-1R signaling and cell survival. Apoptosis. 2020;25(7–8):519–34.
Osher E, Macaulay VM. Therapeutic targeting of the IGF Axis. Cells. 2019;8(8):895.
Huo H, Guo X, Hong S, Jiang M, Liu X, Liao K. Lipid rafts/caveolae are essential for insulin-like growth factor-1 receptor signaling during 3T3-L1 preadipocyte differentiation induction. J Biol Chem. 2003;278(13):11561–9.
Smrcka AV, Brown JH, Holz GG. Role of phospholipase Cepsilon in physiological phosphoinositide signaling networks. Cell Signal. 2012;24(6):1333–43.
Wang Y, Wu X, Ou L, Yang X, Wang X, Tang M, et al. PLCepsilon knockdown inhibits prostate cancer cell proliferation via suppression of Notch signalling and nuclear translocation of the androgen receptor. Cancer Lett. 2015;362(1):61–9.
Jiang J, Eliaz I, Sliva D. Suppression of growth and invasive behavior of human prostate cancer cells by ProstaCaid: mechanism of activity. Int J Oncol. 2011;38(6):1675–82.
Tahir SA, Kurosaka S, Tanimoto R, Goltsov AA, Park S, Thompson TC. Serum caveolin-1, a biomarker of drug response and therapeutic target in prostate cancer models. Cancer Biol Ther. 2013;14(2):117–26.
Li-Weber M. New therapeutic aspects of flavones: the anticancer properties of Scutellaria and its main active constituents Wogonin, Baicalein and Baicalin. Cancer Treat Rev. 2009;35(1):57–68.
Wang L, Ling Y, Chen Y, Li CL, Feng F, You QD, et al. Flavonoid baicalein suppresses adhesion, migration and invasion of MDA-MB-231 human breast cancer cells. Cancer Lett. 2010;297(1):42–8.
Bonham M, Posakony J, Coleman I, Montgomery B, Simon J, Nelson PS. Characterization of chemical constituents in Scutellaria baicalensis with antiandrogenic and growth-inhibitory activities toward prostate carcinoma. Clin Cancer Res. 2005;11(10):3905–14.
Kim JK, Jung Y, Wang J, Joseph J, Mishra A, Hill EE, et al. TBK1 regulates prostate cancer dormancy through mTOR inhibition. Neoplasia. 2013;15(9):1064–74.
Pedersen TR, Tobert JA. Simvastatin: a review. Expert Opin Pharmacother. 2004;5(12):2583–96.
Murata M, Peranen J, Schreiner R, Wieland F, Kurzchalia TV, Simons K. VIP21/caveolin is a cholesterol-binding protein. Proc Natl Acad Sci U S A. 1995;92(22):10339–43.
Hong H, Zhang Y, Sun J, Cai W. Positron emission tomography imaging of prostate cancer. Amino Acids. 2010;39(1):11–27.
Jia L, Wei W, Cao J, Xu H, Miao X, Zhang J. Silencing CD147 inhibits tumor progression and increases chemosensitivity in murine lymphoid neoplasm P388D1 cells. Ann Hematol. 2009;88(8):753–60.
Langeberg WJ, Tahir SA, Feng Z, Kwon EM, Ostrander EA, Thompson TC, et al. Association of caveolin-1 and -2 genetic variants and post-treatment serum caveolin-1 with prostate cancer risk and outcomes. Prostate. 2010;70(9):1020–35.
Lombardo LJ, Lee FY, Chen P, Norris D, Barrish JC, Behnia K, et al. Discovery of N- (2-chloro-6-methyl- phenyl)-2- (6- (4- (2-hydroxyethyl)- piperazin-1-yl)-2-methylpyrimidin-4- ylamino)thiazole-5-carboxamide (BMS-354825), a dual Src/Abl kinase inhibitor with potent antitumor activity in preclinical assays. J Med Chem. 2004;47(27):6658–61.
Nam S, Kim D, Cheng JQ, Zhang S, Lee JH, Buettner R, et al. Action of the Src family kinase inhibitor, dasatinib (BMS-354825), on human prostate cancer cells. Cancer Res. 2005;65(20):9185–9.
Mendel DB, Laird AD, Xin X, Louie SG, Christensen JG, Li G, et al. In vivo antitumor activity of SU11248, a novel tyrosine kinase inhibitor targeting vascular endothelial growth factor and platelet-derived growth factor receptors: determination of a pharmacokinetic/pharmacodynamic relationship. Clin Cancer Res. 2003;9(1):327–37.
Faivre S, Demetri G, Sargent W, Raymond E. Molecular basis for sunitinib efficacy and future clinical development. Nat Rev Drug Discov. 2007;6(9):734–45.
Carducci MA, Nelson JB, Chan-Tack KM, Ayyagari SR, Sweatt WH, Campbell PA, et al. Phenylbutyrate induces apoptosis in human prostate cancer and is more potent than phenylacetate. Clin Cancer Res. 1996;2(2):379–87.
Melchior SW, Brown LG, Figg WD, Quinn JE, Santucci RA, Brunner J, et al. Effects of phenylbutyrate on proliferation and apoptosis in human prostate cancer cells in vitro and in vivo. Int J Oncol. 1999;14(3):501–8.
Acknowledgements
We made Fig. 2 by figdraw platform. Thanks for the support of figdraw platform.
Funding
Funding support for this study was mainly funded by Shandong Provincial Natural Science Foundation (Grant number: ZR2020MH078), China Postdoctoral Science Foundation (Grant number: 2023M731308), Postdoctoral program of Affiliated Hospital of Jining Medical University.
Author information
Authors and Affiliations
Contributions
YD and HY contributed to the conception and design of the study; QB wrote the first draft of the manuscript; YS and LZ modified the grammar; BL analyzed the data; QB and HY drew figures; HY and ZZ revised the manuscript critically; HY wrote parts of the manuscript. All the authors contributed to the manuscript writing, read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bian, Q., Li, B., Zhang, L. et al. Molecular pathogenesis, mechanism and therapy of Cav1 in prostate cancer. Discov Onc 14, 196 (2023). https://doi.org/10.1007/s12672-023-00813-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-023-00813-0