Abstract
Background and Objectives
Acute liver failure (ALF) is an uncommon but potentially dramatic syndrome characterized by massive hepatic necrosis and has a very high mortality rate of 50% to 75% without liver transplantation. This study is aimed at analyzing the etiological spectrum of ALF patients and compare these with ALF mimics such as malaria, dengue fever and other tropical infectious diseases.
Methods
The study population included patients who presented with ALF and ALF mimics in a tertiary care center over two years. We retrospectively analyzed the patient case files and a comparison was made concerning the baseline demographic details, clinical profile, laboratory values and outcomes.
Results
Sixty-three patients were assessed, with 32 in ALF and 31 in ALF mimics group. The most common cause for ALF was hepatitis A virus (25%), followed by hepatitis B virus (18.7%), drug-induced liver injury (12.7%), autoimmune hepatitis (12.5%), hepatitis E virus (9.3%) and Wilson’s disease (6.25%). In the ALF mimics group, malaria (58.06%) was the most common cause, followed by dengue fever (16.1%), leptospirosis (12.9%) and scrub typhus (12.9%). Patients in the ALF mimics group had significantly higher incidence of fever (p = 0.001), hepatosplenomegaly (p = 0.01), anemia (p = 0.02) and shorter jaundice to encephalopathy duration (p = 0.032) as compared to the ALF group, while higher transaminase levels (p = 0.03), bilirubin (p = 0.01), prothrombin time (p = 0.01), serum ammonia (p = 0.02) and mortality (p = 0.02) were observed in ALF patients.
Conclusions
The most common cause for ALF was hepatitis A virus, followed by hepatitis B virus, while in ALF mimics it was malaria followed by dengue fever, in our study. Patients of ALF mimics can have similar presentation, but a high index of suspicion and awareness is required to identify the common infectious ALF mimics for early diagnosis.
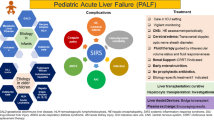
Graphical Abstract


Similar content being viewed by others
Data availability
Department of Gastroenterology, SMS Hospital, Jaipur, India.
References
Acharya SK. Acute liver failure: Indian perspective. Clin Liver Dis (Hoboken). 2021;18:143–9.
Anand AC, Nandi B, Acharya SK, et al. Indian National Association for the Study of the Liver consensus statement on acute liver failure (Part 1): epidemiology, pathogenesis, presentation and prognosis. J Clin Exp Hepatol. 2020;10:339–76.
Shalimar, Acharya SK, Lee W. Worldwide differences in acute liver failure. In: Williams R, Wendon J, editors. Future Medicine Ltd. Critical Care in Acute Liver Failure. 2013;2013:32–46. https://doi.org/10.2217/ebo.12.326.
Devarbhavi H, Joseph T, Sunil Kumar N, et al. The Indian network of drug-induced liver injury: etiology, clinical features, outcome and prognostic markers in 1288 patients. J Clin Exp Hepatol. 2021;11:288–98.
Marudanayagam R, Shanmugam V, Gunson B, et al. Aetiology and outcome of acute liver failure. HPB (Oxford). 2009;11:429–34.
Mehrotra S, Mehta N, Rao PS, et al. Live donor liver transplantation for acute liver failure: a single center experience. Indian J Gastroenterol. 2018;37:25–30.
Murthy GL, Sahay RK, Sreenivas DV, Sundaram C, Shantaram V. Hepatitis in falciparum malaria. Trop Gastroenterol. 1998;19:152–4.
Joshi YK, Tandon BN, Acharya SK, Babu S, Tandon M. Acute hepatic failure due to Plasmodium falciparum liver injury. Liver. 1986;6:357–60.
Anand AC, Garg HK. Approach to clinical syndrome of jaundice and encephalopathy in tropics. J Clin Exp Hepatol. 2015;5:S116–30.
Deepak NA, Patel ND. Differential diagnosis of acute liver failure in India. Ann Hepatol. 2006;5:150–6.
Kumar R, Shalimar, Bhatia V, et al. Antituberculosis therapy induced acute liver failure: magnitude, profile, prognosis, and predictors of outcome. Hepatology. 2010;51:1665–74.
Bernal W, Auzinger G, Wendon J. Prognostic utility of the bilirubin lactate and etiology score. Clin Gastroenterol Hepatol. 2009;7:249–53.
Anand AC, Ramji C, Narula AS, Singh W. Malarial hepatitis: a heterogeneous syndrome? Natl Med J India. 1992;5:59–62.
Kochar DK, Agarwal P, Kochar SK, et al. Hepatocyte dysfunction and hepatic encephalopathy in Plasmodium falciparum malaria. QJM. 2003;96:505–12.
Viswanathan S, Iqbal N, Anemon PP, Kumar GS. Fatal fulminant hepatic failure in a diabetic with primary dengue. J Trop Med. 2010;2010:41356.
Ramachandran S, Godfrey JJ, Perera MVF. Typhoid typhoid fever hepatitis. JAMA. 1974;230:236–40.
Kumar R, Anand U, Priyadarshi RN. Liver transplantation in acute liver failure: Dilemmas and challenges. World J Transplant. 2021;11:187–202.
Acknowledgements
Jaya Maharshi – For typing, formatting and grammar corrections. Shalini Singh- For Statistical Analysis.
Funding
None.
Author information
Authors and Affiliations
Contributions
Saksham Seth, Kamlesh Kumar Sharma: Acquisition, analysis or interpretation of the data. Sudhir Maharshi, Rupesh Pokharna, Sandeep Nijhawan, Shyam Sunder Sharma : Study conception, design and supervision, drafting of article and critical revision for import ant intellectual content, final approval of the version to be published. Sudhir Maharshi: Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
SS, SM, KKS, RP, SN and SSS declare no conflict of interest for this article.
Ethics statement
The study was performed conforming to the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Ethical approval
The institutional ethics committee approved the study protocol, which was conducted in accordance with the Declaration of Helinski. Patient gave their written consent.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Seth, S., Maharshi, S., Sharma, K.K. et al. Changing etiological spectrum of acute liver failure. Indian J Gastroenterol 43, 452–458 (2024). https://doi.org/10.1007/s12664-024-01578-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-024-01578-2