Abstract
Background
All operative procedures for simple or complicated diverticulitis, including primary resection and anastomosis (PRA) with or without a diverting stoma, Hartmann procedure (HP), or stoma reversal, whether done in an elective setting or as an emergency, can be performed laparoscopically. However, owing to low incidence of the disease and complexity of the procedure, there are very few studies on outcomes of laparoscopic surgery for sigmoid diverticulitis from India.
Aim
The present study was undertaken to evaluate outcomes of laparoscopically treated patients of sigmoid diverticulitis.
Methods
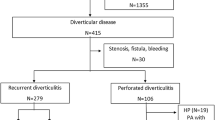
Prospective observational study enrolled 37 patients with sigmoid diverticulitis managed laparoscopically from March 2015 to March 2017. Demographic, clinical, operative, postoperative, and complication data were entered into a patient proforma and analyzed.
Results
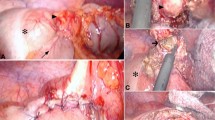
Eleven simple and 26 complicated diverticulitis patients were operated laparoscopically, 22 in emergency setting and 15 in elective setting. Only three patients required conversion to open surgery—two due to dense adhesions and one due to chronic obstructive pulmonary disease (COPD). No patients had ureteric or bowel injury. Eighteen patients underwent laparoscopic PRA without stoma, 11 patients had PRA with stoma, 6 had HP, and 2 had laparoscopic lavage. Results showed lesser blood loss, shorter hospital stay, and fewer complications in the elective group and simple diverticulitis patients. None of the patients had anastomosis-related complications. Two patients had stoma-related complications.
Conclusion
Laparoscopic management of diverticulitis is feasible, safe, provides the benefits of less wound-related complications, and shorter hospital stay and should be the surgical procedure of choice in elective or emergency setting for simple/complicated diverticulitis.
Similar content being viewed by others
References
Floch MH. Colonic diverticulosis and diverticulitis: National Diverticulitis Study Group, 2008 update. J Clin Gastroenterol. 2008;42:1123–4.
Daher R, Barouki E, Chouillard E. Laparoscopic treatment of complicated colonic diverticular disease: a review. World J Gastrointest Surg. 2016;8:134–42.
Rodkey GV, Welch CE. Changing patterns in the surgical treatment of diverticular disease. Ann Surg. 1984;200:466–78.
Kurumboor P, Kamalesh NP, Pramil K, et al. Laparoscopic management of colonic diverticular disease and its complications: an analysis. Indian J Surg. 2017;79:380–3.
Angenete E, Thornell A, Burcharth J, et al. Laparoscopic lavage is feasible and safe for the treatment of perforated diverticulitis with purulent peritonitis: the first results from the randomized controlled trial DILALA. Ann Surg. 2016;263:117–22.
Afshar S, Kurer MA. Laparoscopic peritoneal lavage for perforated sigmoid diverticulitis. Color Dis. 2012;14:135–42.
Cirocchi R, Afshar S, Di Saverio S, et al. A historical review of surgery for peritonitis secondary to acute colonic diverticulitis: from Lockhart-Mummery to evidence-based medicine. World J Emerg Surg. 2017;12:14.
Letarte F, Hallet J, Drolet S, et al. Laparoscopic emergency surgery for diverticular disease that failed medical treatment: a valuable option? Results of a retrospective comparative cohort study. Dis Colon Rectum. 2013;56:1395–402.
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13:606–8.
Strate LL, Modi R, Cohen E, Spiegel BMR. Diverticular disease as a chronic illness: evolving epidemiologic and clinical insights. Am J Gastroenterol. 2012;107:1486–93.
Weizman AV, Nguyen GC. Diverticular disease: epidemiology and management. Can J Gastroenterol. 2011;25:385–9.
Tursi A, Papagrigoriadis S. Review article: the current and evolving treatment of colonic diverticular disease. Aliment Pharmacol Ther. 2009;30:532–46.
Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57:284–94.
Khalil HA, Yoo J. Colorectal emergencies: perforated diverticulitis (operative and nonoperative management). J Gastrointest Surg. 2014;18:865–8.
Köhler L, Sauerland S, Neugebauer E. Diagnosis and treatment of diverticular disease: results of a consensus development conference. The Scientific Committee of the European Association for Endoscopic Surgery. Surg Endosc. 1999;13:430–6.
Anaya DA, Flum DR. Risk of emergency colectomy and colostomy in patients with diverticular disease. Arch Surg. 2005;140:681–5.
Faria GR, Almeida AB, Moreira H, Pinto-de-Sousa J, Correia-da-Silva P, Pimenta AP. Acute diverticulitis in younger patients: any rationale for a different approach? World J Gastroenterol. 2011;17:207–12.
Smadja C, Sbai Idrissi M, Tahrat M, et al. Elective laparoscopic sigmoid colectomy for diverticulitis. Results of a prospective study. Surg Endosc. 1999;13:645–8.
Bhakta A, Tafen M, Glotzer O, et al. Laparoscopic sigmoid colectomy for complicated diverticulitis is safe: review of 576 consecutive colectomies. Surg Endosc. 2016;30:1629–34.
Pittet O, Kotzampassakis N, Schmidt S, Denys A, Demartines N, Calmes JM. Recurrent left colonic diverticulitis episodes: more severe than the initial diverticulitis? World J Surg. 2009;33:547–52.
Biondo S, Parés D, Martí Ragué J, Kreisler E, Fraccalvieri D, Jaurrieta E. Acute colonic diverticulitis in patients under 50 years of age. Br J Surg. 2002;89:1137–41.
Ambrosetti P, Gervaz P. Management of sigmoid diverticulitis: an update. Updat Surg. 2016;68:25–35.
Vennix S, Musters GD, Mulder IM, et al. Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: a multicentre, parallel-group, randomised, open-label trial. Lancet. 2015;386:1269–77.
Sorrentino M, Brizzolari M, Scarpa E, et al. Laparoscopic peritoneal lavage for perforated colonic diverticulitis: a definitive treatment? Retrospective analysis of 63 cases. Tech Coloproctol. 2015;19:105–10.
Winter DC. LapLAND, Laparoscopic lavage for acute non-faeculant diverticulitis.
Schultz JK, Wallon C, Blecic L, et al. One-year results of the SCANDIV randomized clinical trial of laparoscopic lavage versus primary resection for acute perforated diverticulitis. Br J Sur. 2017;104:1382–92.
Köckerling F, Schneider C, Reymond MA, et al. Laparoscopic resection of sigmoid diverticulitis. Results of a multicenter study. Laparoscopic Colorectal Surgery Study Group. Surg Endosc. 1999;13:567–71.
Carbajo Caballero MA, Martin del Olmo JC, Blanco Alvarez JI, et al. Acute diverticulitis and diverticular disease of the colon: a safe indication for laparoscopic surgery. Rev Esp Enferm Dig. 2000;92:718–25.
Kirchhoff P, Clavien PA, Hahnloser D. Complications in colorectal surgery: risk factors and preventive strategies. Patient Saf Surg. 2010;4:5.
Vermeulen J, Coene PP, Van Hout NM, et al. Restoration of bowel continuity after surgery for acute perforated diverticulitis: should Hartmann’s procedure be considered a one-stage procedure? Color Dis. 2009;11:619–24.
Author information
Authors and Affiliations
Contributions
All authors have contributed to the formulation of the paper, data collection, and literature review. Overall guidance by the consultant Dr. Hitesh Mehta and drafting and figure acquisition by the residents.
Corresponding author
Ethics declarations
Conflict of interest
GSD, RN, PP, BB, PV, and HM declare that they have no conflict of interest.
Ethics statement
The study was performed in a manner to conform to the Helsinki Declaration of 1975, as revised in 2000 and 2008, concerning human and animal rights, and the authors followed the policy concerning informed consent as shown in springer.com.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Disclaimer
The authors are solely responsible for the data and the content of the paper. In no way the Honorary Editor-in-Chief, Editorial Board Members, or the printer/publishers are responsible for the results/findings and content of this article.
Rights and permissions
About this article
Cite this article
Desai, G.S., Narkhede, R., Pande, P. et al. An outcome analysis of laparoscopic management of diverticulitis. Indian J Gastroenterol 37, 430–438 (2018). https://doi.org/10.1007/s12664-018-0907-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-018-0907-0