Abstract
Purpose
The prone position can lead to anatomical compression of the thoracic cavity resulting in reduced cardiac output, especially in the context of chest wall deformities commonly present in patients with scoliosis. There are no protocols for using transesophageal echocardiography (TEE) to optimize prone positioning and for safe use of TEE during cases requiring neuromonitoring.
Clinical features
We present a case of a 23-yr-old male with Cornelia de Lange syndrome undergoing elective posterior spinal fusion for syndromic scoliosis who developed severe refractory hypotension and cardiac arrest in the prone position. After hemodynamic stabilization in the intensive care unit, the patient returned to the operating room on postoperative day 2 for completion of his spinal fusion. Transesophageal echocardiography determined the optimal position of longitudinal bolster placements associated with minimal left ventricular compression in the supine position. The patient was then proned and intraoperative hemodynamics during the second surgery remained stable. Owing to the special considerations of using TEE in the prone position with neuromonitoring, we describe technical aspects to consider to protect the equipment and patient.
Conclusion
Patients with compliant chest walls or thoracic deformities are at risk of hemodynamic instability in the prone position. Intraoperative TEE can be used in the supine patient prior to proning to determine optimal longitudinal bolster positioning to minimize cardiac compression. Transesophageal echocardiography used during spine surgery in the prone position with neuromonitoring and motor-evoked potentials requires special considerations for patient safety.
Résumé
Objectif
La position ventrale peut entraîner une compression anatomique de la cavité thoracique provoquant une réduction du débit cardiaque, en particulier dans le contexte de déformations de la paroi thoracique, fréquentes chez les patients atteints de scoliose. Il n’existe aucun protocole guidant l’utilisation de l’échocardiographie transœsophagienne (ETO) pour optimiser le positionnement ventral et pour favoriser l’utilisation sécuritaire de l’ETO dans les cas nécessitant un neuro-monitorage.
Caractéristiques cliniques
Nous présentons le cas d’un homme de 23 ans atteint d’un syndrome de Cornelia de Lange bénéficiant d’une fusion spinale postérieure non urgente pour traiter une scoliose syndromique; le patient a manifesté une hypotension réfractaire sévère et un arrêt cardiaque en position ventrale. Après stabilisation hémodynamique à l’unité de soins intensifs, le patient est retourné en salle d’opération au jour postopératoire 2 pour terminer sa fusion spinale. L’échocardiographie transœsophagienne a permis de déterminer la position optimale des traversins longitudinaux qui était associée à une compression ventriculaire gauche minimale en décubitus dorsal. Le patient a ensuite été positionné sur le ventre, et les valeurs hémodynamiques peropératoires sont restées stables au cours de la deuxième chirurgie. En raison des considérations particulières de l’utilisation de l’ETO en position ventrale avec neuro-monitorage, nous décrivons les aspects techniques à prendre en compte pour protéger l’équipement et le patient.
Conclusion
Les patients présentant des parois thoraciques compliantes ou des déformations thoraciques sont à risque d’instabilité hémodynamique en position ventrale. L’ETO peropératoire peut être utilisée chez le patient en décubitus dorsal avant le positionnement ventral pour déterminer le positionnement optimal des traversins longitudinaux afin de minimiser la compression cardiaque. L’utilisation de l’échocardiographie transœsophagienne lors d’une chirurgie du rachis en position ventrale avec neuro-monitorage et potentiels évoqués moteurs nécessite des considérations particulières en ce qui a trait à la sécurité des patients.
Similar content being viewed by others
Physiologic cardiovascular changes are known to be associated with the prone position during scoliosis correction surgery because of the increased mechanical pressure on the thoracic cavity and heart.1 In healthy anesthetized patients, transesophageal echocardiography (TEE) has shown a 10–20% reduction in cardiac index despite optimal prone positioning.2 Potential causes for this are a reduction in preload due to decreased left ventricle (LV) compliance or inferior vena cava compression from the increased intrathoracic pressures.2
In pediatric patients undergoing scoliosis correction surgery, cases of profound obstructive hypotension caused by mechanical stress of the prone position have been described.3,4 These patients might have associated increased chest wall compliance or deformities. While pectus excavatum is commonly thought of as a primarily cosmetic concern, there are reports of patients with this chest wall deformity undergoing cardiac compromise when in the prone position for spine surgery.5,6,7
We present an adult patient with Cornelia de Lange syndrome, pectus excavatum, and rapidly progressive scoliosis who developed unanticipated severe hypotension and cardiac arrest in the prone position during an elective posterior spinal fusion. We describe a unique approach to using TEE to guide bolster positioning during the secondary surgery, as well as our safety considerations when using TEE in a case of neuromonitoring with motor-evoked potentials.
Case presentation
Written consent from the patient’s power of attorney was obtained to publish this case. A 23-yr-old male with known Cornelia de Lange Syndrome presented with severe progressing syndromic thoracolumbar scoliosis (Cobb angle, 80 degrees). Preoperatively, the patient required assistance for short distance ambulation and needed a wheelchair for long distances. Due to his rapid and symptomatic curve progression, the patient was scheduled for an eight-hour elective T2 to pelvis scoliosis correction. The patient was otherwise healthy, had a normal body mass index (height, 171 cm; weight, 61 kg), and had no known cardiac history. On physical examination, it was noted that the patient had a narrow anteroposterior thoracic diameter with pectus excavatum. The patient was optimized for surgery and no preoperative cardiac investigations were warranted.
Following an uneventful induction of general anesthesia and maintenance using total intravenous anesthesia with propofol, the patient was placed in the prone position on a Jackson table with a transverse chest bolster and iliac pads for support. He maintained hemodynamic stability for the first three hours of the surgery but during insertion of the pedicle screws in the thoracic region, the patient became persistently hypotensive despite fluid boluses and initiation of norepinephrine vasopressor support. Owing to the refractory hypotension, the decision was made to stop the surgery and close the incision emergently after placement of the T8 pedicle screws. The differential diagnosis at this time was presumed to include vascular injury leading to bleeding; myocardial injury; or obstructive causes such as pulmonary embolism, venous air embolism, or tension pneumothorax. While repositioning the patient from prone to supine, he went into a pulseless electrical activity arrest that required two minutes of cardiopulmonary resuscitation and 1 mg of epinephrine prior to regaining return of spontaneous circulation. An urgent computed tomography angiogram did not reveal any source of bleeding or obstruction but showed a compressed left atrium between the thoracic spine and sternum. The patient had a significant rise in troponin-I levels postoperatively with a peak of 6,483 ng·L-1. On postoperative day (POD) 1, a transthoracic echocardiogram (TTE) showed that the LV was normal in size with a moderately reduced ejection fraction of 35–40%, that the left atrial anteroposterior dimension was small with cavity compression, and that there was regional wall motion abnormality with findings of Takotsubo cardiomyopathy.
After hemodynamic stabilization and weaning of vasopressor support, our multidisciplinary team ultimately decided that proceeding with prompt surgical management was best for the patient because of the high risk of infection from the expedited superficial incision closure as well as the risks associated with spinal instability.
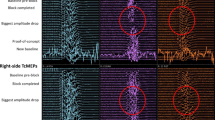
The patient returned to the operating room on POD 2 with a plan to use longitudinal bolsters on either side of his chest instead of a transverse chest bolster to minimize cardiac chamber compression. Following induction and endotracheal intubation, intraoperative TEE was used to guide bolster placement in the supine position prior to placing the patient prone. The bolsters were placed in various configurations in the supine position (Fig. 1) with gentle body weight provided to mimic the weight of the patient. Transgastric long and short axis views were obtained dynamically as the bolsters were moved up and down the chest wall to determine the optimal positioning. The TEE showed that placing the most proximal part of the bolsters in the higher thoracic region at the level of the axilla caused significant dynamic LV compression. In contrast, bolster position was optimal when positioned most proximally in the lower thoracic region at the level of the nipple line with minimal compression of the LV (Fig. 1). The patient was then transferred to the prone position, maintaining the optimized bolster position. To facilitate TEE access, the patient was placed in Mayfield head pins as opposed to the standard face cushion. Intraoperative TEE monitoring was used to guide volume resuscitation and vasopressor support during the surgery. Throughout the operation, minimal LV compression was noted on imaging, and the patient remained hemodynamically stable on norepinephrine infusion 2–20 µg·min-1 at maximum. The patient received 3 L of blood products and 6 L of fluid resuscitation with a total estimated blood loss of 3.5 L.
A) Computed tomography chest imaging showing reduced anteroposterior diameter between the sternum and anterior vertebrae over the right heart. B) Initial configuration of the horizontal bolster placement prior to proning with echocardiographic evidence of cardiac compression. C) Fourth variation in bolster placement with two bolsters placed vertically below the nipple line prior to proning without any echocardiographic evidence. D) Transgastric short axis view by echo without any bolster placement. E) Transgastric short axis view with high bolster placement in image d. F) Transgastric short axis view with low bolster placement in image c.
A protective bite block configuration was developed to facilitate the safe use of both the TEE and transcranial motor-evoked potentials (tcMEPs). The TEE probe was placed through a rigid TEE bite block (Bitestrong™ B4; Batrick Medical Manufacturing, Surgmed Group, Montreal, QC, Canada), which was wrapped in gauze and placed in the center of the patient’s mouth. The endotracheal tube was then taped next to the rigid bite block. This design protected the TEE, while allowing the probe to be manipulated without risking displacement of the endotracheal tube. Next, to prevent the tongue from slipping in-between the teeth, two round cylindrical bite blocks made from gauze were placed on each side of the mouth, in-between the patient’s teeth. During placement of these bite blocks, the tongue was inspected to ensure that it did not fold over and remained in the midline. Finally, to ensure that the bite blocks could not fall out of the mouth in the prone position, two Tegaderm™ IV dressings (3.5 × 4.5 inches; 3M™, Maplewood, MN, USA) were placed on top of the mouth (Fig. 2). The TEE probe was secured to the side of the operating room table at the level of the patient’s head when not in use to minimize compression injury and prevent movement.
Overall, the patient tolerated the revision surgery well. He was returned to the intensive care unit following surgery and was extubated on POD 1 without complications. At two-year follow-up, the patient was most satisfied with his improved upright posture and ability to ambulate long distances independently without assistance.
Discussion
This case is unique for a number of reasons. First, we describe an adult patient with advanced syndromic scoliosis and pectus excavatum presenting for spine surgery, a presentation more common in the pediatric population. Second, the bolster positioning was optimized to minimize LV compression first in the supine and then in the prone position using TEE guidance. Third, profound hypotension only occurred during placement of the pedicle screws after three hours of prone positioning. This suggests that the application of compressive surgical forces, which are unavoidable in scoliosis repair, in addition to bolster placement should be considered as contributing to hemodynamic compromise. Finally, this is a unique case of using TEE with concurrent tcMEPs throughout a prone procedure.
In healthy anesthetized patients, the decrease in cardiac index with prone position is thought to be caused by a reduction in ventricular preload.2 Pectus excavatum is an anterior chest wall deformity that involves depression of the sternum over the manubrium that progresses inwards toward the xiphoid process.8 As in our case, the depressed sternum of pectus excavatum patients may cause mechanical compression of the heart and lead to cardiovascular collapse when in prone position. The etiology for this hemodynamic instability, based on TEE imaging, is compression on the sternum leading to right-sided cardiac compression4,5,7 or a collapsed left atrium and biventricular failure.3 Reports of patients with compliant chest walls4 or pectus excavatum3,5 who experienced hemodynamic instability following surgery in prone position with a transverse bolster describe the benefit of using longitudinal bolsters leading to less compression to the thoracic cage and ability to complete prone surgery successfully. A study of 51 healthy adult patients who underwent TEE evaluation of five different prone positioning systems used in spine surgery concluded that the Jackson table or properly placed longitudinal bolsters had the least hemodynamic impact.9 Bafus et al.6 and Gala et al.7 report two separate cases of 15-yr-old males with pectus excavatum and thoracolumbar scoliosis that experienced severe hypotension in the prone position supported with a transverse chest bolster for their elective posterior spinal fusion. Gala et al. used TEE to show that the transverse chest bolster was causing the patient’s sternum to compress the right side of the heart.7 Bafus et al. showed an inflow obstruction caused by stress on the sternum on TEE.6 Both patients underwent pectus excavatum repairs and then returned to the operating room at a later date for posterior spinal fusions, which were well tolerated.
While the use of TEE during spine surgery has been previously reported,3,4,5,6,7,9 this is a rare description of using TEE to guide bolster placement in the supine position prior to proning and its continuous use with tcMEPs. Transesophageal echocardiogram use in conjunction with intraoperative monitoring and tcMEPs can cause injury to the patient’s teeth and oral cavity, and to the TEE probe because of repeated provoked movements of the jaw.10 There is also concern for pressure-related injury to the tongue and other oral structures from the weight of the TEE probe during a prolonged surgery in the prone position.11 Therefore, we had to develop a bite block described in the case presentation that facilitated the safe use of the equipment and successfully protected the patient. In addition, Mayfield head pins were used instead of a face cushion to facilitate access and visualization of this setup. Nevertheless, we acknowledge that a limitation of this setup is that it requires sufficient space in the oral cavity to accommodate the TEE probe and the bite blocks. A patient with a small oral cavity or a large tongue would be at higher risk of soft tissue injury or ischemia. In that scenario, the risks of using a TEE probe concurrently with MEPs should be carefully considered. Further research and commercial development of bite blocks intended specifically for this purpose might be an important next step to improve safety and reduce variability associated with handmade devices.
Limitations of this case report include the description of a single patient as well as the lack of direct visualization and cardiac monitoring during the episode of hemodynamic collapse. Nonetheless, the successful completion of the surgery with adjustment of bolster positioning leads us to believe that the cardiac compression from the transverse chest bolster was responsible for the event. The cause of the arrest in the initial surgery, along with the significant troponin elevation after cardiopulmonary resuscitation, was thought to be the severely reduced preload causing reduced cardiac output and myocardial perfusion. Although we did not have intraoperative TEE in this case, the TTE performed postoperatively revealed a depressed LV with regional wall motion abnormalities, supporting this differential. One must consider the potential for air embolism as a cause of arrest in the prone position as well. In our case, although TEE guidance was not used in the original surgery to rule out air embolism, the right ventricular function was normal on the postoperative TTE and no intracardiac shunt or patent foramen ovale was detected. An anesthesiologist with cardiac subspecialty training and certification in advanced perioperative TEE performed and analyzed the TEE intraoperatively. This may be a limitation for some centers performing spine surgeries and may be a reason to refer higher risk cardiac patients requiring scoliosis repair to centers where intraoperative TEE is available.
Conclusion
Patients with compliant chest walls or thoracic deformities are at risk of hemodynamic instability from spinal surgery in the prone position. From this case report and the studies enumerated above, a cautious approach is warranted for patients at risk of hemodynamic instability from mechanical cardiac compression in the prone position. Preoperatively, some patients might benefit from pectus excavatum repair. Intraoperatively, continuous TEE can be used as a diagnostic and prognostic monitor to help manage and avoid acute emergencies.12 In this case, TEE was used to guide bolster placement in the supine position after positioning the patient prone, and then throughout the surgical repair to optimize cardiac filling and function. The most useful views in our case were the deep transgastric short axis and long axis views, which qualitatively showed very clear changes in cardiac filling, seen as severe LV compression with high longitudinal bolster placement that was minimized when the bolsters were moved caudad. We also used the midesophageal right ventricle (RV) inflow–outflow view to examine the right ventricular outflow tract (RVOT), and were able to rule out RV and RVOT compression in the different positions. Other important views during spine surgery in the prone position include the midesophageal bicaval view for assessment of the interatrial septum, particularly if air embolism was a concern. Deep transgastric assessment of the left ventricular outflow tract velocity time integral by pulsed wave doppler can provide stroke volume information that is useful to detect subtle changes in cardiac output with positioning or in response to therapies. During surgery, TEE use in the prone position with neuromonitoring and motor-evoked potentials requires special considerations for patient safety. To prevent injury to the patient and damage to the TEE, we suggest using a protective bite block configuration and Mayfield head pins as described here.
References
Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. Br J Anaesth 2008; 100: 165–83. https://doi.org/10.1093/bja/aem380
Chui J, Craen RA. An update on the prone position: continuing professional development. Can J Anesth 2016; 63: 737–67. https://doi.org/10.1007/s12630-016-0634-x
Abcejo AS, Diaz Soto J, Castoro C, Armour S, Long TR. Profound obstructive hypotension from prone positioning documented by transesophageal echocardiography in a patient with scoliosis: a case report. A A Case Rep 2017; 9: 87–9. https://doi.org/10.1213/xaa.0000000000000534
Neira VM, Gardin L, Ryan G, Jarvis J, Roy D, Splinter W. A transesophageal echocardiography examination clarifies the cause of cardiovascular collapse during scoliosis surgery in a child. Can J Anesth 2011; 58: 451–5. https://doi.org/10.1007/s12630-011-9461-2
Alexianu D, Skolnick ET, Pinto AC, et al. Severe hypotension in the prone position in a child with neurofibromatosis, scoliosis and pectus excavatum presenting for posterior spinal fusion. Anesth Analg 2004; 98: 334–5. https://doi.org/10.1213/01.ane.0000096187.58714.b6
Bafus BT, Chiravuri D, van der Velde ME, Chu BI, Hirshl R, Farley FA. Severe hypotension associated with the prone position in a child with scoliosis and pectus excavatum undergoing posterior spinal fusion. J Spinal Disord Tech 2008; 21: 451–4. https://doi.org/10.1097/bsd.0b013e31815725f2
Galas JM, van der Velde ME, Chiravuri SD, Farley F, Parra D, Ensing GJ. Echocardiographic diagnosis of right ventricular inflow compression associated with pectus excavatum during spinal fusion in prone position. Congenit Heart Dis 2009; 4: 193–5. https://doi.org/10.1111/j.1747-0803.2008.00231.x
Beltsios ET, Mitsos SL, Panagiotopoulos NT. Pectus excavatum and scoliosis: a review about the patient's surgical management. Gen Thorac Cardiovasc Surg 2020; 68: 1225–33. https://doi.org/10.1007/s11748-020-01496-y
Dharmavaram S, Jellish WS, Nockels RP, et al. Effect of prone positioning systems on hemodynamic and cardiac function during lumbar spine surgery: an echocardiographic study. Spine (Phila Pa 1976) 2006; 31: 1388–93. https://doi.org/10.1097/01.brs.0000218485.96713.44
Yata S, Ida M, Shimotsuji H, et al. Bite injuries caused by transcranial electrical stimulation motor-evoked potentials' monitoring: incidence, associated factors, and clinical course. J Anesth 2018; 32: 844–9. https://doi.org/10.1007/s00540-018-2562-0
Yoshida G, Imagama S, Kawabata S, et al. Adverse events related to transcranial electric stimulation for motor-evoked potential monitoring in high-risk spinal surgery. Spine (Phila Pa 1976) 2019; 44: 1435–40. https://doi.org/10.1097/brs.0000000000003115
Teran F, Prats MI, Nelson BP, et al. Focused transesophageal echocardiography during cardiac arrest resuscitation: JACC review topic of the week. J Am Coll Cardiol 2020; 76: 745–54. https://doi.org/10.1016/j.jacc.2020.05.074
Author contributions
Kim Phan, Adele Budiansky, Elizabeth Miller, and Philippe Phan contributed to the writing of the manuscript. Daniel Dubois contributed to the conception and writing of the manuscript.
Disclosures
None.
Funding statement
None.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Phan, K., Budiansky, A., Miller, E. et al. Novel use of transesophageal echocardiography to optimize hemodynamics and patient positioning during prone scoliosis surgery and safety considerations in the setting of intraoperative neuromonitoring: a case report. Can J Anesth/J Can Anesth 69, 1556–1561 (2022). https://doi.org/10.1007/s12630-022-02334-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02334-w