Abstract
Background
Home pain remains the most common complication in outpatient surgery. Optimal management requires good information and early availability of analgesics. The main objective of this randomized controlled trial was to compare the effects of pre- vs postoperative analgesic instruction and prescription on postoperative home pain.
Methods
Patients were randomized into an anesthesia consultation group (AC group) and a standard postoperative group (POP group). The AC group and the POP group received analgesic prescription and instruction during the anesthesia consultation and after surgery, respectively. The primary outcome was the incidence of home pain on postopertive day one (D1). Home pain was defined by at least one episode with a numeric rating scale score > 3/10 at rest. Treatment compliance and postoperative nausea and vomiting (PONV) were also assessed on D1 and postoperative day 7 (D7).
Results
One hundred and eighty-six patients were included between May 2017 and May 2018 at Rouen University Hospital, France. Ninety-four patients were randomized to the AC group and 92 to the POP group. On D1, the incidence of pain was 23/94 (24%) in the AC group and 44/92 (48%) in the POP group (P < 0.001). On D1, the rate of treatment compliance was significantly higher in the AC group than in the POP group (85% vs 69%; P = 0.02). There was no statistically significant difference in the incidence of pain or treatment compliance between groups on D7 or in PONV on D1 and on D7.
Conclusions
Preoperative analgesic instruction and prescription during anesthesia consultation reduces the incidence of early postoperative home pain in outpatient surgery.
Trial registration
www.clinicaltrialsgov (NCT03205189); registered 2 July 2017.
Résumé
Contexte
La douleur à la maison demeure la complication la plus fréquente après une chirurgie ambulatoire. Une prise en charge optimale nécessite de bonnes informations et la disponibilité précoce d’analgésiques. L’objectif principal de cette étude randomisée contrôlée était de comparer les effets d’instructions et d’une prescription pré- vs postopératoires d’analgésiques sur la douleur postopératoire à la maison.
Méthode
Les patients ont été randomisés dans un groupe de consultation pré-anesthésique (groupe pré) et un groupe postopératoire standard (groupe post). Le groupe pré et le groupe post ont reçu une prescription d’analgésiques ainsi que les instructions s’y rattachant pendant la consultation en anesthésie préopératoire et après la chirurgie, respectivement. Le critère d’évaluation principal était l’incidence de douleur à la maison au premier jour postopératoire (post-op 1). La douleur à domicile était définie par un épisode de douleur ou plus avec un score > 3/10 au repos sur l’échelle d’évaluation numérique. L’observance du traitement et les nausées et vomissements postopératoires (NVPO) ont également été évalués les jours post-op 1 et 7.
Résultats
Cent quatre-vingt-six patients ont été inclus entre mai 2017 et mai 2018 au Centre hospitalier universitaire de Rouen. Quatre-vingt-quatorze patients ont été randomisés au groupe pré et 92 au groupe post. Au jour post-op 1, l’incidence de la douleur était de 23/94 (24 %) dans le groupe pré et de 44/92 (48 %) dans le groupe post (P < 0,001). Au jour post-op 1, le taux d’observance du traitement était significativement plus élevé dans le groupe pré que dans le groupe post (85 % vs 69 %; P = 0,02). Il n’y avait aucune différence statistiquement significative dans l’incidence de douleur ou d’observance du traitement entre les groupes au jour post-op 7 ou dans les NVPO aux jours post-op 1 et 7.
Conclusion
L’instruction et la prescription préopératoires d’analgésiques pendant la consultation anesthésique préopératoire réduisent l’incidence de la douleur postopératoire précoce à domicile en chirurgie ambulatoire.
Enregistrement de l’étude
www.clinicaltrials.gov (NCT03205189); enregistrée le 2 juillet 2017.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative home pain remains the most common complication encountered in outpatient surgery, with an incidence of around 30% for moderate to severe pain.1,2,3,4 The consequences of home pain are multiple and can lead to the development or aggravation of postoperative nausea and vomiting (PONV), chronic pain, significant functional impact, sleep disorders, disabling functional impotence and outpatient consultation or even re-hospitalization.5,6 The objective of outpatient analgesia is to reduce pain using a multimodal pharmacologic and non-pharmacologic approach to facilitate movement and recovery after return home. Pain management at home is a challenge for the anesthesiologist, who must anticipate the optimal analgesic treatment for the patient at home, depending on the surgery and the type of anesthesia. Patient information and instruction are essential for the management of postoperative pain both in anesthesia consultation and after surgery. Previous studies have already shown that the postoperative period is not appropriate for providing information on postoperative prescriptions to patients.7,8 In a previous study of 638 patients scheduled for orthopedic outpatient surgery, we observed that analgesic prescription during anesthesia consultation reduced home pain.9 However, this study was not randomized and therefore did not provide a high level of evidence on the effects of this early prescription. The main objective of the present study was to fill this void and conduct a randomized controlled comparison of the effects on postoperative home pain of preoperative analgesic prescription during anesthesia consultation vs standard postoperative analgesic prescription.
Methods
Population selection
This prospective randomized controlled trial was conducted from 27 May 2017 to 28 May 2018 in the outpatient surgery unit of a tertiary care hospital in Rouen, France. The study protocol was reviewed and approved by the institutional review board (Comité de Protection des Personnes Nord Ouest; study number 2015-A01088-41) on 18 November 2016 and on ClinicalTrials.gov (NCT03205189, principal investigator: Prof. Vincent Compere, 2 July 2017). All patients who had outpatient surgery with general anesthesia were eligible for the study. Written consent was obtained from all patients. Exclusion criteria were pregnancy, age < 18 yr old, American Society of Anesthesiology (ASA) Physical Status score ≥ III, no general anesthesia, general anesthesia combined with loco-regional anesthesia, chronic pain (> three months), chronic analgesic consumption (> three months), contraindication to non-steroidal anti-inflammatory drugs, preoperative consumption of acetaminophen with codeine or preoperative consumption of morphine, active or past drug addiction, cognitive disorders or dementia, serious psychiatric disorders, and absence of proficiency in French.
Study procedure
Consultation group and postoperative group
Participants were randomized into two groups at the end of the anesthesia consultation (ten days before surgery): an anesthesia consultation group (AC group) and a standard postoperative group (POP group). The investigator received an envelope prior to each consultation indicating the group in which the patient should be included. Group allocation was carried out using a centralized computer system. Before the beginning of the study, all anesthesiologists of the outpatient surgery unit were told what information should be given to the patient. The two groups of patients were given the same standardized information by the same team of anesthesiologists. The choice of different treatments and their duration for this study were determined from analysis of the published data.10,11
The AC group received an analgesic prescription at the end of the anesthesia consultation and information concerning the use of analgesics during the same consultation. The anesthesiologist insisted that the patient collect their treatment at the pharmacy at the end of the anesthesia consultation and stressed the importance of systematically taking the prescribed treatment postoperatively, even in the absence of pain. The POP group received the same prescription and information but in the postoperative period in the outpatient surgery unit before return home (three hours after general anesthesia, just before discharge). In both groups, information concerning the systematic administration of analgesics was written on the prescription (Fig. 1).
Prescriptions
Two types of prescription were available depending on the expected postoperative pain (Electronic Supplementary Material [ESM]; eAppendix A). The anesthesiologist filled either prescription A for moderate pain (expected numeric rating scale [NRS] > 3; range, 0–10) or prescription B for severe pain (expected NRS > 6; range, 0–10). To guide anesthesiologists in this choice, a list of surgical procedures (type A or B surgery) (ESM, eAppendix A) was available based on published data.12 Prescription A combined acetaminophen-codeine (500 mg/30 mg) regularly every six hours during the first two days and was continued up to five days if the pain persisted more than two days (the quantity dispensed by the pharmacy was sufficient for five days); and ketoprofen (100 mg) regularly every 12 hr during the first two days. Prescription B combined acetaminophen-codeine (500 mg/30 mg) regularly every six hours during the first two days and continued up to five days if the pain persisted more than two days (the quantity dispensed by the pharmacy was sufficient for five days); ketoprofen (100 mg) regularly every 12 hr during the first two days; and morphine sulfate (10 mg) regularly every six hours during the first two days if the NRS > 6 (ESM, eAppendix B). In our outpatient surgery unit, the following surgeries are done under general anesthesia alone: dental surgery (wisdom teeth and multiple dental avulsion); abdominal surgery (inguinal and umbilical hernia, laparoscopic cholecystectomy); gynecological surgery (hysteroscopy, breast lumpectomy); orthopedic surgery (meniscectomy and anterior cruciate ligament repair); and ear, nose, and throat surgery (stapedectomy, scialendoscopy, sphenoidectomy, meatotomy, ethmoidectomy, myringoplasty, adenoidectomy, rhinoplasty, septoplasty, polyendoscopy, laser laryngeal microsurgery, and surgical removal of skin lesions on the face with or without a flap).
Anesthesia procedure
General anesthesia was standardized in the operating theatre with the routine use of propofol for induction (2 mg·kg−1), total intravenous anesthesia (TIVA) with propofol (target plasma concentration, between 2 and 6 µg·mL−1) or sevoflurane (end-tidal concentration, 2%) for the maintenance of hypnosis, and TIVA with remifentanil (target plasma concentration, between 3 and 6 ng·mL−1). Hyperalgesia was managed using ketamine (0.15 mg·kg−1) during general anesthesia. In the absence of respective contraindications, intraoperative analgesia was managed with the routine administration of acetaminophen (1 g), nefopam (20 mg), and ketoprofen (100 mg). Tramadol (50 mg) or morphine (0.1 mg·kg−1) administration was permissible at the end of the surgery at the anesthesiologist’s discretion. During the patient’s hospitalization in the postanesthesia care unit (PACU) and in the outpatient surgery unit, pain was assessed using an NRS of 0–10. Morphine titration was done in the PACU if necessary (NRS > 3/10). Postoperative nausea and vomiting was managed according to Apfel’s score with intraoperative dexamethasone (4 mg) and droperidol (1.25 mg). The outpatient surgery and anesthesia teams in the operating theatre and PACU were blind to group allocation. The investigator collected data blindly, always at the same time in the afternoon, by telephone questionnaire on the first postoperative day (D1) and seven days after surgery (D7; ESM, eAppendix C). All patients were informed that they would receive a telephone call 24 hr after the surgery, in the afternoon. However, they were not aware of the type of questions they would be asked during the telephone call.
Outcome measures
The primary outcome was the incidence of home pain at rest on D1 after outpatient surgery. Home pain was defined by at least one episode of pain at rest > 3/10 on a NRS, range 0–10, within the first 24 hr.
Secondary outcomes were the incidence of pain during hospitalization on the day of surgery (D0) and of home pain on D7. Pain during hospitalization on D0 and home pain on D7 were measured using an NRS of 0–10; pain at rest was defined by at least one episode of NRS scores > 3/10. The following secondary outcomes were also measured:
-
The incidence of PONV on D0, D1, and D7. The incidence of PONV was defined by at least one episode of nausea or vomiting in the postoperative period.
-
Morphine consumption, if prescribed, on D0, D1, and D7. Morphine consumption was defined by at least one titration of intravenous morphine in the PACU or in the outpatient surgery unit on D0, by administration of at least one tablet of morphine sulfate on D1, and by administration of morphine between D3 and D7 as assessed on D7.
-
Analgesic treatment compliance on D1 and D7. Treatment compliance on D1 was defined as the patient’s systematic adherence to the prescription even in the absence of pain during the first 24 hr. Treatment compliance on D7 was defined as the patient’s still systematic use of analgesics on D7 (acetaminophen-codeine or ketoprofen or morphine).
-
The patient’s satisfaction with prescribed treatment on D1 and D7. Patient satisfaction was evaluated using a scale of 0–10; satisfaction was defined by a score ≥ 8/10.
Statistical analysis
Statistical analyses were performed with R 3.1.4 (the R Foundation for Statistical Computing, http://www.r-project.org) and Prism Version 6 (GraphPad Software, LLC; San Diego, CA, USA). Data are presented as means (standard deviation [SD]) for continuous measurements and as n (%) for categorical variables. Previous reports described a percentage of patients with pain > 3/10 between 25 and 60%.9,13,14,15,16 As we included different types of surgery, to estimate the number of patients, we set at 45% the percentage of patients without experimental intervention with a pain intensity of > 3/10. We expected a decrease of 50% of pain, i.e., a percentage of patients with pain > 3/10 of 22.5%. To demonstrate a decrease from 45% to 22.5%, with 5% alpha, 90% power, and taking into account a 10% loss of follow-up, the required sample size was 200 patients. The Gaussian distribution of the data was explored using the Shapiro-Wilk test. Following these explorations, the quantitative variables were compared with a non-parametric Mann-Whitney test. Comparison of the percentage of the primary outcome was assessed using a Chi square test. We also calculated 95% confidence intervals (95% CIs) of percentages, using the Exact Clopper Person’s method via the PropCIs R package (shearer/PropCIs). The number needed to treat to benefit (NNTB) was estimated as 1/absolute risk difference. The absolute risk reduction (ARR) was defined as ARR= ppop-pAc and the 95% CI of NNTB was estimated as described.13 The percentages of secondary outcomes were compared using the Chi square test or Fisher’s exact test depending on the group size. For continuous measurements, data are presented as mean (SD) and for qualitative parameters, data are presented as n (%). P values were two-tailed, with statistical significance indicated by a value of P < 0.05 for the primary outcome. To avoid false discovery, P < 0.01 was considered significant for secondary outcomes.
Results
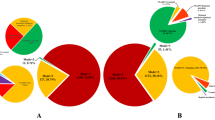
Two hundred patients were recruited and randomized, 102 in the AC group and 98 in the POP group. Fourteen patients were excluded; three because they did not present on the day of surgery, two were unable to return home after surgery, two had a contraindication to surgery or to anesthesia on the day of surgery, and four patients randomized in AC and three in POP could not be contacted on D1. Twenty patients could not be contacted on D7. Consequently, on D1, 94 patients in the AC group and 92 in the POP group, and on D7, 86 and 80 patients respectively were considered for the analysis (Fig. 2). Patient characteristics and type of anesthesia or surgery are summarized in Table 1.
Study flow chart. AC group = anesthesia consultation group; POP group = postoperative group. Prescription A = prescription for moderate postoperative pain (expected numeric rating scale [NRS] >3; range 0–10 on D1); prescription B = prescription for severe postoperative pain (expected NRS >6; range, 0–10 on D1). D0 = day of surgery; D1 = postoperative day 1; D7 = postoperative day 7; NRS = numeric rating scale.
Incidence of postoperative home pain on postoperative days 1 and 7
On D1 (Table 2), 67 patients (36%; 95% CI, 30 to 44) had at least one episode of pain at home during the first 24 hr postoperatively: 23 of 94 (24%) in the AC group vs 44 of 92 (48%) in the POP group (ARR, -23%; 95% CI, –10 to -37; P < 0.001). The NNTB was 4.2 (95% CI, 2.7 to 9.4). On D7 (Table 3), 20 patients (12%; 95% CI, 8 to 18) had at least one episode of pain: 7 of 86 (8%) in the AC group vs 13 of 80 (16%) in the POP group (ARR, -8%;95% CI, 2 to –18; P = 0.11).
The rate of regular analgesic consumption at home on the evening after surgery was 85% in the AC group vs 70% in the POP group (P = 0.01); 85% vs 69% (P = 0.02) on D1, respectively, and 46% vs 52% (P = 0.44) on D7, respectively. The incidence of PONV for all patients was 16% on D1 and 16% on D7 and was comparable between the two groups. On D1, no patient required re-hospitalization or medical assistance. On D7, 27 patients required medical assistance for persistent pain or medication intolerance. Sixteen of these patients were in the AC group (12 patients had acetaminophen-codeine intolerance, two patients had ketoprofen intolerance, and two patients had persistent pain) and 11 were in the POP group (seven patients had acetaminophen-codeine intolerance, two patients had ketoprofen intolerance and two patients had persistent pain) (P = 0.24). Global patient satisfaction (NRS ≥ 8/10) was comparable between groups on D1 (94% in the AC group and 94% in the POP group, P = 1).
Discussion
Preoperative instruction and prescription of analgesics significantly reduced the incidence of postoperative home pain during the first 24 hr after surgery and produced a decrease in pain intensity. Our results are concordant with our previous non-randomized prospective study that found a significant decrease in pain in the first 24 hr after orthopedic outpatient surgery (18% in the AC group compared with 30% in the POP group, P < 0.01).9 In our work, analgesic prescription and information on analgesia management were provided at the end of the anesthesia consultation, which is a much more favourable context than during the immediate postoperative period. Indeed, Watt-Watson et al. showed, in a cohort of 180 outpatients, that a significant proportion of patients felt that they had not received clear instructions on how to take painkillers and that 56% said they had not been informed on what to do in the event of treatment failure or adverse reactions. Finally, patients reported that this information was often provided in the postoperative period, when their attention level was diminished.7 Moreover, on a practical level, the simple fact that patients were able to obtain analgesic drugs before their surgery probably made it possible not only to avoid painful movements during the immediate postoperative period but also to improve drug intake because of the immediate availability of their analgesic treatments. These hypotheses are supported by the improvement in treatment compliance with prescribed analgesics on D1 between the two groups (85% vs 69%). This result has already been reported in studies that included patients who received their analgesics when leaving the hospital.8
These results may suggest a placebo effect associated with the early analgesic prescription, as patients feel more prepared for surgery and postoperative pain. Recent studies focused on the beneficial effect of placebo induced by the physician’s oral explanations.14,15 The analgesic effect of the placebo can be triggered by verbal instructions; in fact, the neurobiological effects of placebo analgesia are known to be related to neuromodulators released into the brain.16 These results suggest that simply knowing that a patient is being treated by a medical doctor increases the analgesic effect. Information and instruction, positive expectations, and communication with the patient could, therefore, trigger a neurobiological cascade that enhances self-confidence, reducing the stress and anxiety that cause the placebo effect.
Our work shows that the incidence of early moderate to severe pain was around 36% in the whole cohort. This result is higher than that found in the literature, with a range between 20 and 30%.3,7 The inclusion of a significant proportion (30%) of patients who had surgery and with moderate to severe pain outcomes was probably one of the reasons for this result. Also, outpatient surgery studies have shown that performing procedures such as orthopedic surgery under regional anesthesia can significantly reduce moderate to severe postoperative pain on D1.17,18 It should also be noted that the difference between the two groups on the pain scale was small. Typically, an NRS difference of 1.3 is used to show a clinically meaningful outcome, and we only found a difference of 0.8 between the two groups in our study.19,20 The fact that patient satisfaction with overall and anesthetic management was similar between the two groups reinforces the argument that the absolute pain difference between the two groups is not clinically important.
It is also interesting to observe that, among the 30% of surgeries defined as painful, only 19% benefited from the prescription of morphine as a rescue treatment. Even if morphine prescription is now recommended by French guidelines, our results suggest that emergency morphine is insufficiently prescribed in outpatients by anesthesiologists, probably because of apprehension of side effects at home or even the risk of causing opiate addiction in patients.21 In addition, morphine consumption may be limited directly by patients themselves; only 5% of patients consumed morphine on D1 and 16% on D7, probably for fear of inducing opioid dependence.22,23 Nevertheless, this study was not designed to evaluate the choice of anesthesiologists with regard to morphine prescription or to assess patients’ attitudes in relation to morphine prescription. A further study to evaluate these attitudes would be interesting. Fifty percent of our patients systematically took painkillers at D7, and 20% had a pain intensity > 3/10 at D7. Our initial prescriptions, which varied between two and five days, were probably inappropriate for these surgeries and should be reassessed and extended to seven days. Two hypotheses come to mind; either the patients stopped taking their treatment after 48 hr and there was a painful rebound or we had underestimated the duration of the pain for the surgery concerned.
Our study has some limitations. First, this work could not be carried out with double-blinding because of the study design. Nevertheless, the investigator evaluating the primary endpoint was blinded to group allocation. Second, the fact that this study was conducted in a single centre does not allow our results to be generalized to other outpatient surgery units. Thirdly, based on the results of our preliminary study, we excluded patients with loco-regional anesthesia and chronic opioid consuming patients who represent a significant number of patients. Our population is, therefore, not completely representative of a significant proportion of patients managed in outpatient surgery.
Conclusions
This work shows that early preoperative instruction and analgesic prescription at the end of anesthesia consultations reduced the incidence of home pain more effectively than standard late postoperative analgesic prescription in outpatient surgery.
References
Jafra A, Mitra S. Pain relief after ambulatory surgery: progress over the last decade. Saudi J Anaesth 2018; 12: 618-25.
Schug SA, Chong C. Pain management after ambulatory surgery. Curr Opin Anaesthesiol 2009; 22: 738-43.
McGrath B, Elgendy H, Chung F, Kamming D, Curti B, King S. Thirty percent of patients have moderate to severe pain 24 hr after ambulatory surgery: a survey of 5,703 patients. Can J Anesth 2004; 51: 886-91.
Kaye AD, Urman RD, Rappaport Y, et al. Multimodal analgesia as an essential part of enhanced recovery protocols in the ambulatory settings. J Anaesthesiol Clin Pharmacol 2019; 35(Suppl 1): S40-5.
Thomas DA, Chang D, Zhu R, Rayaz H, Vadivelu N. Concept of the ambulatory pain physician. Curr Pain Headache Rep 2017; . https://doi.org/10.1007/s11916-017-0611-2.
Vadivelu N, Kai AM, Kodumudi V, Berger JM. Challenges of pain control and the role of the ambulatory pain specialist in the outpatient surgery setting. J Pain Res 2016; 9: 425-35.
Watt-Watson J, Chung F, Chan VW, McGillion M. Pain management following discharge after ambulatory same-day surgery. J Nurs Manag 2004; 12: 153-61.
Marquardt HM, Razis PA. Prepacked take-home analgesia for day case surgery. Br J Nurs 1996; 5: 1114-8.
Lemarie M, Compère V, Fourdrinier V, et al. Evaluation of the impact of prescription analgesic during the anaesthesia consultation on the incidence of postoperative pain at home in ambulatory orthopaedic surgery (French). Ann Fr Anesth Reanim 2011; 30: 883-7.
Pavlin DJ, Chen C, Penaloza DA, Buckley FP. A survey of pain and other symptoms that affect the recovery process after discharge from an ambulatory surgery unit. J Clin Anesth 2004; 16: 200-6.
Mitchell A, McCrea P, Inglis K, Porter G. A randomized, controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine (Tylenol 3) after outpatient breast surgery. Ann Surg Oncol 2012; 9: 3792-800.
Rawal N, Hylander J, Nydahl PA, Olofsson I, Gupta A. Survey of postoperative analgesia following ambulatory surgery. Acta Anaesthesiol Scand 1997; 41: 1017-22.
Altman DG, Andersen PK. Calculating the number needed to treat for trials where the outcome is time to an event. BMJ 1999; 319: 1492-5.
Vase L, Wartolowska K. Pain, placebo, and test of treatment efficacy: a narrative review. Br J Anaesth 2019; 123: e254-62.
Klinger R, Stuhlreyer J, Schwartz M, Schmitz J, Colloca L. Clinical use of placebo effects in patients with pain disorders. Int Rev Neurobiol 2018; 139: 107-28.
Forsberg JT, Martinussen M, Flaten MA. The placebo analgesic effect in healthy individuals and patients: a meta-analysis. Psychosom Med 2017; 79: 388-94.
Kamming D, Chung F, Williams D, McGrath B, Curti B. Pain management in ambulatory surgery. J Perianesth Nurs 2004; 19: 174-82.
Shnaider I, Chung F. Outcomes in day surgery. Curr Opin Anaesthesiol 2006; 19: 622-9.
Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med 2001; 38: 633-8.
Kendrick DB, Strout TD. The minimum clinically significant difference in patient-assigned numeric scores for pain. Am J Emerg Med 2005; 23: 828-32.
Aubrun F, Nouette Gaulain K, Fletcher D, et al. Réactulaisation de la recommandation sur la douleur postopératoire. Anesth Réanim 2016; 2: 3421-30.
Fishbain DA, Cole B, Lewis J, Rosomoff HL, Rosomoff RS. What percentage of chronic nonmalignant pain patients exposed to chronic opioid analgesic therapy develop abuse/addiction and/or aberrant drug-related behaviors? A structured evidence-based review. Pain Med 2008; 9: 444-59.
Salsitz EA. Chronic pain, chronic opioid addiction: a complex nexus. J Med Toxicol 2016; 12: 54-7.
Author contributions
Jean Selim was involved in the study conception and design, in the acquisition of data, in statistical analysis, in analysis and interpretation of data, and in drafting the manuscript. Céline Chaventre and Zoubir Djerada were involved in the study conception and design, in the acquisition of data, in analysis and interpretation of data and in drafting the manuscript. Bertrand Dureuil was involved in resident recruitment and in manuscript revision. Emmanuel Besnier and Thomas Clavier were involved in the study conception and design, in resident recruitment, and in manuscript revision. Vincent Compere was involved in the study conception and design, in resident recruitment, in study coordination, in the interpretation of data, and in manuscript revision. All authors read and approved the final manuscript.
Acknowledgements
The authors are grateful to Nikki Sabourin-Gibbs, Rouen University Hospital, for her help in editing the manuscript to all the senior anesthesiologists from Caen and Rouen University Hospitals who agreed to be experts to read this work and to all the anesthesiologists of Rouen University Hospital who participated in this work.
Disclosures
None.
Funding statement
Support was provided solely from departmental sources.
Editorial responsibility
This submission was handled by Dr. Gregory L. Bryson, former Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Selim, J., Djerada, Z., Chaventre, C. et al. Preoperative analgesic instruction and prescription reduces early home pain after outpatient surgery: a randomized controlled trial. Can J Anesth/J Can Anesth 69, 1033–1041 (2022). https://doi.org/10.1007/s12630-021-02023-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-021-02023-0