Abstract
Purpose
Supraglottic airways are commonly used as conduits for fibreoptic bronchoscopy (FOB)-guided intubation in pediatric patients. We hypothesized that anesthesiology trainees with limited prior experience with FOB-guided intubation through a supraglottic airway in children would intubate the trachea faster through the air-Q™ supraglottic airway than through the i-gel™.
Methods
Ninety-six children aged one month to six years were randomized to receive either the i-gel or air-Q for FOB-guided tracheal intubation by anesthesiology trainees. Time for successful tracheal intubation was the primary endpoint. Secondary endpoints included: time for device insertion, number of attempts for successful device insertion, airway leak pressures, FOB grade of laryngeal view, total number of attempts for tracheal intubation, time for removal of the device after tracheal intubation, and associated complications.
Results
The median (interquartile range [IQR]) times to successful tracheal intubation for the air-Q (62.5 [47.9-77] sec) and the i-gel (55.9 [48.5-81.8] sec) were not significantly different (median difference 6.6 sec; 95% confidence interval [CI] -13.3 to 8.7; P = 0.53). The median (IQR) time to insertion for the air-Q (16.7 [14.4-20.0] sec) was shorter than for the i-gel (19.6 [16.7-23.0] sec) (median difference 2.9 sec; 95% CI 0.8 to 4.7; P = 0.005). There were no differences between devices with respect to airway leak pressures, success rates, and time to removal. Compared with the air-Q, the i-gel was associated with more problems during device removal after tracheal intubation, including breakage of the tracheal tube pilot balloon (n = 0 vs n = 13, respectively; P < 0.001), inadvertent extubation (n = 1 vs n = 5, respectively; P < 0.001), and difficulty controlling the tracheal tube (n = 0 vs n = 21, respectively; P < 0.001).
Conclusions
Contrary to our hypothesis, both the air-Q and i-gel supraglottic airways served as effective conduits for FOB-guided tracheal intubation in children when performed by trainees with limited prior experience. The i-gel, however, was associated with more problems during device removal following tracheal intubation. This study was registered at http://clinicaltrials.gov/show/NCT02189590.
Résumé
Objectif
Les voies aériennes supraglottiques sont fréquemment utilisées comme conduits pour l’intubation guidée par bronchoscopie à fibre optique (FOB) chez les patients pédiatriques. Nous avons formulé l’hypothèse que des résidents en anesthésiologie n’ayant qu’une expérience antérieure limitée de l’intubation guidée par FOB via une voie aérienne supraglottique chez des enfants, intuberaient la trachée plus rapidement avec la voie aérienne supraglottique air-Q™ qu’avec l’i-gel™.
Méthodes
Quatre-vingt-seize enfants âgées d’un mois à six ans ont été randomisés pour recevoir une intubation trachéale guidée par FOB avec l’i-gel ou l’air-Q par des rèsidents en anesthésiologie. Le critère d’évaluation principal était le temps nécessaire à la réussite de l’intubation trachéale. Les critères d’évaluation secondaires incluaient : le temps d’insertion du dispositif, le nombre de tentatives nécessaires à une insertion réussie du dispositif, les pressions de fuite de la voie aérienne, le grade FOB de la vue laryngée, le nombre total de tentatives d’intubation trachéale, le temps nécessaire au retrait du dispositif après l’intubation trachéale, et les complications associées.
Résultats
Les temps médians (intervalle interquartile [IQR]) de réussite de l’intubation trachéale avec l’air-Q (62,5 [47,9-77] sec) ou l’i-gel (55,9 [48,5-81,8] sec) n’ont pas été significativement différents (différence médiane : 6,6 sec; intervalle de confiance [IC] à 95 %: -13,3 à -8,7; P < 0,53). Le temps médian (IQR) d’insertion a été plus court avec l’air-Q (16,7 [14,4-20,0] sec) qu’avec l’i-gel (19,6 [16,7-23,0] sec) (différence médiane 2,9 sec; IC à 95 %: 0,8 à 4,7; P < 0,005). Il n’y a pas eu de différences entre les dispositifs sur les plans des pressions de fuite de la voie aérienne, des taux de succès et des temps de retrait. Comparativement à l’air-Q, l’i-gel a été associé à davantage de problèmes au cours du retrait du dispositif après l’intubation trachéale, incluant le bris du ballonnet du tube trachéal (respectivement, n = 0 contre n = 13; P < 0,001), l’extubation accidentelle (respectivement, n = 1 contre n = 5; P < 0,001), et la difficulté à contrôler le tube trachéal (respectivement, n = 0 contre n = 21; P < 0,001).
Conclusions
Contrairement à notre hypothèse, les voies aériennes supraglottiques air-Q et i-gel ont toutes les deux servi de conduits efficaces pour l’intubation trachéale guidée par FOB chez des enfants quand l’intubation était pratiquée par des résidents ayant une expérience antérieure limitée. L’i-gel a toutefois été associé à davantage de problèmes au cours du retrait du dispositif après intubation trachéale. Cette étude a été enregistrée sur le site http://clinicaltrials.gov/show/NCT02189590.
Similar content being viewed by others
Fibreoptic bronchoscopy (FOB) is an essential skill in the field of anesthesia. In the pediatric population, acquisition of this skill can be more challenging as the smaller diameter of the bronchoscope requires a different technique than that used for adult-sized bronchoscopes.1 Additionally, as the incidence of a difficult airway is fairly low in the pediatric population,2 practice of these skills on normal airways would allow a better transfer of skills when a difficult airway is encountered.
The use of FOB to guide tracheal intubation through a supraglottic airway (SGA) is an established technique for securing the airway in children when conventional laryngoscopy is unsuccessful.3 , 4 Advantages of using an SGA for this purpose include the ability to overcome upper airway obstruction5 , 6 and provision of a hands-free airway7 with a relatively straightforward path to the larynx. For these reasons, SGA-guided intubations are preferred by many pediatric anesthesiologists for the management of the difficult pediatric airway.8
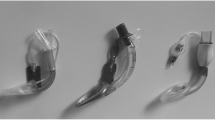
The air-Q™ SGA (Mercury Medical; Clearwater, FL, USA) is designed for tracheal intubation and has been shown to be an effective conduit for FOB-guided tracheal intubation in children.9 – 13 The i-gel™ (Intersurgical; Wokingham, UK) is a newer SGA that has been shown to be effective for primary anesthetic maintenance, exhibiting higher airway leak pressures compared with other commonly utilized SGAs in children.14 , 15 Additionally, some studies have also found similarly favourable fibreoptic views of the larynx through the i-gel when compared with other SGAs,16 , 17 making it potentially useful for facilitating tracheal intubations. To date, there is a lack of formal studies assessing the i-gel’s suitability as a conduit for FOB-guided tracheal intubation in children. We therefore sought to compare the use of these two SGAs as conduits for tracheal intubation in the hands of clinicians who may not have extensive experience with pediatric bronchoscopes in their practice.
The primary aim of this study was to compare the i-gel with the air-Q in terms of the time to successful FOB-guided tracheal intubation performed by anesthesia trainees. We hypothesized that the use of the air-Q SGA would result in faster FOB-guided tracheal intubation times than would result with the use of the i-gel. We also assessed secondary outcomes, including the time and success of SGA placement, airway leak pressure, FOB grade of laryngeal view, and the time for removal of the device after successful tracheal intubation.
Methods
The Institutional Review Board of the Stanley Manne Children’s Research Institute approved this study in June 2014. Written informed consent was obtained from the guardians of all patients. Ninety-six children (American Society of Anesthesiologists physical status I-III, aged one month to six years) scheduled for elective surgery under general endotracheal anesthesia were enrolled in this study. Children with active upper respiratory infections, significant pulmonary disease, a known history of and/or suspicion of a difficult airway, or airway abnormalities were not enrolled in the study.
A computer-generated randomization was utilized for SGA assignment (i-gel or air-Q) and was revealed to the study investigator just prior to device placement. Only cuffed endotracheal tubes (ETT) were utilized in this study (Mallinckrodt Inc.; St Louis, MO, USA). All SGA placements, FOB-guided tracheal intubations, and removal of the SGA after intubation were performed by anesthesia trainees. An anesthesia trainee was defined as a resident or fellow from clinical anesthesia (CA) years 2, 3, or 4 who had not previously performed FOB-guided tracheal intubation through an SGA in children. All trainees participating in the study were volunteers and their prior experience with FOB-guided tracheal intubation was verified through their case logs. Before participating, the trainees received a brief lecture and viewed a video outlining the steps for FOB-guided tracheal intubation through an SGA. Two expert study investigators were involved with each patient: one to ensure standardization of methodology between patients, and the other to supervise the anesthesia trainee closely and to offer verbal cues and airway maneuvers if needed.
All patients received general anesthesia with inhalation induction using nitrous oxide 70% in 30% oxygen and 8% sevoflurane. An intravenous cannula was placed, and rocuronium 0.6 mg·kg−1 iv was administered. Nitrous oxide was then discontinued, and sevoflurane was maintained with an end-tidal concentration of 3% and an end-tidal oxygen concentration greater than 90% prior to SGA insertion.
Supraglottic airway insertion
Both devices were placed using a standard midline insertion technique. Device size was chosen based on the manufacturer’s guidelines. The time for device insertion started with the removal of the facemask and ended when end-tidal carbon dioxide was observed. For the air-Q, intracuff pressure was standardized to 40 cm H2O using a cuff pressure gauge. Successful placement was confirmed with the ability to achieve tidal volumes of at least 7 mL·kg−1 and a square-wave capnogram. The airway leak pressure was measured with the expiratory valve closed and a fresh gas flow of 3 L·min−1 until equilibrium was seen on the pressure gauge.18 The trainees were allowed a maximum of three attempts to place the SGA successfully. The number of attempts for placement and problems during placement (changing device size, downward traction, and spontaneous dislodgement) were also recorded.
Tracheal intubation through the SGA
All FOB-guided tracheal intubations through the SGA were performed with a video tower to visualize the intubation process on an external monitor. Three separate times were then measured by a study investigator, all beginning with the removal of the facemask: (1) Time to first glottic view: defined as the duration of time ending with the first view of the glottic opening. (2) Time to carinal view: defined as the duration of time ending with visualization of the carina. (3) Time to successful tracheal intubation: defined as the duration of time ending with the confirmation of end-tidal carbon dioxide after successful tracheal intubation. One of the study investigators used a previously published scale to grade the FOB view of the larynx through the SGA just proximal to the ventilating orifice.19
The trainee was allowed a total of three attempts for successful FOB-guided tracheal intubation. The patient’s lungs were ventilated through the SGA between attempts, and the time was restarted between each attempt. A failed attempt was defined as any evidence of oxygen desaturation (SpO2 < 90%), any time the bronchoscope had to be withdrawn completely from the SGA, (i.e., secretions, disorientation, or oxygen desaturation), or requiring more than three minutes per attempt.1
Airway maneuvers, such as jaw thrust, neck extension/flexion, or anterior laryngeal pressure, were allowed to improve the laryngeal grade of view and/or to facilitate passage of the tracheal tube. These maneuvers were performed only by the study investigators if indicated (suboptimal laryngeal view/resistance to tracheal tube passage), and the total number of maneuvers needed was recorded. The number of cues needed was also recorded. Verbal cues were offered when prompted by the trainee if disorientation occurred (i.e., if the attending anesthesiologist viewed the red opaque screen and observed that the trainee made no purposeful movement with the bronchoscope) or if there was difficulty in tracheal tube passage. The verbal cues offered by the attending anesthesiologist were standardized.
Removal of the SGA
Following successful tracheal intubation, the SGA was removed using a second ETT as a stabilizing rod. The time for removal of the device started with the disconnection of the breathing circuit and ended when end-tidal carbon dioxide was observed. The number of verbal cues needed during the removal process was recorded. Each trainee then scored the process of removing the SGA after tracheal intubation on a subjective scale of 1-4 (1 = no difficulty; 2 = mild difficulty; 3 = moderate difficulty; 4 = severe difficulty). Problems encountered during SGA removal were recorded, including difficulty in controlling the tracheal tube, pilot balloon breakage, or inadvertent extubation. If needed, broken pilot balloons would be repaired using a 22G angiocatheter attached to a one-way valve inserted into the inflation line.20
The trachea would be intubated by direct laryngoscopy if correct SGA placement was not achieved within three attempts, FOB intubation through the device was not successful after three attempts, or the ETT was dislodged during SGA removal. At the end of the surgical procedure, the ETT was removed after standard extubation criteria were met. Perioperative complications such as oxygen desaturation, laryngospasm, and bronchospasm were also recorded.
The primary outcome measure of this study was the time to successful tracheal intubation. Group sample sizes of 48 each would achieve 90% power to reject the null hypothesis of equal means when the mean difference between SGAs is 20.0 sec (minimum clinically accepted difference), with a standard deviation of 30.0 sec and an alpha of 0.05 using a two-sided two-sample equal-variance Student’s t test. Power analysis was performed using PASS version 12 (NCSS, LLC; Kaysville, UT, USA).
Intraoperative data were recorded using a standardized data collection sheet, entered into a database using Microsoft® Excel® 2010, and then imported into Stata® 12 software (StataCorp LP, College Station, TX, USA) for statistical analysis. The median [IQR] was calculated for demographic data and for non-normally distributed continuous and ordinal variables, including time for SGA placement, time to intubation, number of attempts, number of airway maneuvers, and time for SGA removal. Comparisons of times to intubation were performed using the Mann-Whitney U test. Frequencies and percentages were calculated for categorical variables and compared between groups using Fisher’s exact test. All reported P values are two sided.
Results
Twenty-four trainees participated in this study (CA-2 = 12, CA-3 = 6, CA-4 = 6) from July to August 2014. Demographics are presented in Table 1. A CONSORT diagram representing the flow of patients is shown in the Figure.
All SGAs were placed on the first attempt. The median [IQR] time for successful placement with the air-Q was faster than with the i-gel (16.7 [14.4-20.0] sec vs 19.6 [16.7-23.0] sec, respectively; median difference 2.9 sec; 95% CI 0.8 to 4.7; P = 0.005). The i-gel was associated with more problems during placement (Table 2). No differences were found in the times to the first glottic view or the carinal view. Similarly, for our primary endpoint, the overall median [IQR] time to tracheal intubation was not different between the devices (air-Q, 62.5 [47.9-77] sec vs i-gel, 55.9 [46.5-81.8] sec; median difference 6.6 sec; 95% confidence CI -13.3 to 8.7; P = 0.53). Also, no differences were found in the number of attempts, fibreoptic grades of view, maneuvers for passage of the tracheal tube, or verbal cues offered (Table 3).
Time for removal of the SGA did not differ between devices, but the i-gel was associated with more problems during removal (Table 4). Outright failure of FOB-guided tracheal intubation occurred in two children in the air-Q group (inability to intubate the trachea within three attempts). In both cases, direct laryngoscopy was used to intubate the trachea without difficulty. Direct laryngoscopy was used to intubate the trachea without difficulty in six patients where the ETT was dislodged during SGA removal (n = 2, i-gel size 1.5; n = 3, i-gel size 2.0; and n = 1, air-Q size 1.5).
There was no significant difference in the complication rates between the two devices. Transient oxygen desaturation (SpO2 < 90%) occurred during FOB tracheal intubation in five patients (n = 1, i-gel; n = 4, air-Q). During removal of the SGA, transient desaturation occurred in two patients in the air-Q group. There were no instances of regurgitation, laryngospasm, or bronchospasm.
Discussion
The main finding in this study was that both the air-Q and i-gel supraglottic airways served as effective conduits for FOB-guided tracheal intubation in children when performed by trainees with limited prior experience. The i-gel, however, was associated with more problems during placement and device removal following tracheal intubation.
The three tracheal intubation time points observed in this study did not differ between the two devices in the hands of the trainees. Although the overall times for successful tracheal intubation in this study were slower than previous trials with the air-Q and other SGAs by experts,10 , 12 they are still within acceptable clinical limits for FOB-guided tracheal intubation times in children. It has been shown in previous studies that the i-gel is associated with better FOB grades of view in children when compared with the LMA-Classic™16 and LMA-ProSeal™.17 In this study, we did not show a difference between the two devices in regard to FOB grades of view. The overall successful rates of tracheal intubation suggest that tracheal intubation through an SGA is a relatively straightforward process, even with limited prior experience.
Although the time for successful placement of the device was faster with the air-Q, this difference may not be clinically significant. Additionally, this difference may be related to the greater number of issues associated with the i-gel, as evidenced by spontaneous dislodgement and the need for continuous downward traction on the device, a finding also reported by other investigators.21 – 24 Despite these concerns, both devices had high insertion success rates. The insertion success rates are encouraging given the limited clinical experience of the anesthesia trainees with either device in children prior to this study. The leak pressures with the air-Q in this study are consistent with those in other studies using this device in children.10 , 12 , 25 , 26 The leak pressures of the i-gel appear to be lower than what has been reported in systematic reviews and meta-analyses in children.14 , 15 It is possible that operator inexperience may have contributed to the lower airway leak pressures associated with the i-gel.
Compared with the air-Q, the longer airway tube of the i-gel can be a disadvantage for purposes of tracheal intubation. If the airway tube of the SGA is nearly the same length as the ETT being utilized (i.e., size 1.5 i-gel with a 3.5 ETT), the ETT may or may not be adequately past the vocal cords during tracheal intubation, and this may also cause difficulties during removal of the device, including inadvertent tracheal extubation. The use of an airway exchange catheter or a double-tube assembly to create a “longer ETT” may help to overcome this challenge and decrease the risk of tracheal extubation.27 Another reasonable option may be to leave both the ETT and the i-gel in place until the conclusion of the procedure. The increased potential for tracheal extubation or pilot balloon breakage associated with SGAs that have relatively long/narrow airway tubes should be a consideration when choosing a device to facilitate tracheal intubation in patients with a difficult airway. Therefore, the pilot balloon of the ETT should perhaps be electively removed (sizes 1 and 1.5 i-gel) when using cuffed tracheal tubes, especially if removal of the SGA is planned after tracheal intubation. This was also shown in a trial with the smaller-sized Ambu™ and Aura–i™ (Ambu USA Glen Burnie, MD USA) due to their narrower proximal airway tube.12 Also, the pediatric-sized LMA-Classic/ProSeal will not accommodate passage of the pilot balloon during removal.28 The wider airway tube of the air-Q allows passage of cuffed ETTs, including their pilot balloons, and its shorter length may decrease the risk of ETT dislodgment during the device removal process.10 , 12 Although it was not tested in this study, a theoretical advantage of the i-gel would be the ability to evacuate gastric contents (except size 1 devices), a feature that is not available with the air-Q. This feature may be useful if airway rescue is required in a patient with a “full stomach” with subsequent need for tracheal intubation.
There were several limitations to this study. First, we studied children with only normal airways, and our results may not apply to children with difficult airways. Second, the clinical performance of these devices was tested in the hands of trainees, and these results may differ in the hands of experts. Third, the expert study investigators were allowed to offer verbal cues to aid the trainees; therefore, the results may not truly represent novices performing FOB-guided tracheal intubations on their own without instructive assistance. Finally, data collection was not blinded to the outcome assessors.
The i-gel may be an acceptable alternative to the air-Q as a conduit for FOB-guided tracheal intubation in children in terms of timing outcomes. Nevertheless, when using a cuffed ETT through the i-gel, appropriate precautions for i-gel removal must be considered because of its longer and relatively narrower airway tube. When compared with the i-gel, the air-Q permits the passage of a cuffed ETT and provides a relatively easy process for removal of the device after tracheal intubation. For these practical advantages, the air-Q may be preferred over the i-gel as a conduit for tracheal intubation in children.
References
Wheeler M, Roth AG, Dsida RM, et al. Teaching residents pediatric fiberoptic intubation of the trachea: traditional fiberscope with an eyepiece versus a video-assisted technique using a fiberscope with an integrated camera. Anesthesiology 2004; 101: 842-6.
Heinrich S, Birkholz T, Ihmsen H, Irouschek A, Ackermann A, Schmidt J. Incidence and predictors of difficult laryngoscopy in 11,219 pediatric anesthesia procedures. Paediatr Anaesth 2012; 22: 729-36.
Law JA, Broemling N, Cooper RM, et al. The difficult airway with recommendations for management—part 1—difficult tracheal intubation encountered in an unconscious/induced patient. Can J Anesth 2013; 60: 1089-118.
Engelhardt T, Weiss M. A child with a difficult airway: what do I do next? Curr Opin Anaesthesiol 2012; 25: 326-32.
Asai T, Nagata A, Shingu K. Awake tracheal intubation through the laryngeal mask in neonates with upper airway obstruction. Paediatr Anaesth 2008; 18: 77-80.
Jagannathan N, Sequera-Ramos L, Sohn L, Wallis B, Shertzer A, Schaldenbrand K. Elective use of supraglottic airway devices for primary airway management in children with difficult airways. Br J Anaesth 2014; 112: 742-8.
Sohn LE, Jagannathan N, Sequera-Ramos L, Sawardekar A, Schaldenbrand K, De Oliveira GS. A randomised comparison of free-handed vs air-Q assisted fibreoptic-guided tracheal intubation in children < 2 years of age. Anaesthesia 2014; 69: 723-8.
Brooks P, Ree R, Rosen D, Ansermino M. Canadian pediatric anesthesiologists prefer inhalational anesthesia to manage difficult airways. Can J Anesth 2005; 52: 285-90.
Jagannathan N, Kho MF, Kozlowski RJ, Sohn LE, Siddiqui A, Wong DT. Retrospective audit of the air-Q intubating laryngeal airway as a conduit for tracheal intubation in pediatric patients with a difficult airway. Paediatr Anaesth 2011; 21: 422-7.
Jagannathan N, Kozlowski RJ, Sohn LE, et al. A clinical evaluation of the intubating laryngeal airway as a conduit for tracheal intubation in children. Anesth Analg 2011; 112: 176-82.
Jagannathan N, Roth AG, Sohn LE, Pak TY, Amin S, Suresh S. The new air-Q intubating laryngeal airway for tracheal intubation in children with anticipated difficult airway: a case series. Paediatr Anaesth 2009; 19: 618-22.
Jagannathan N, Sohn LE, Sawardekar A, et al. A randomized trial comparing the Ambu® Aura-i™ with the air-Q™ intubating laryngeal airway as conduits for tracheal intubation in children. Paediatr Anaesth 2012; 22: 1197-204.
Fiadjoe JE, Stricker PA. The air-Q intubating laryngeal airway in neonates with difficult airways. Paediatr Anaesth 2011; 21: 702-3.
Maitra S, Baidya DK, Bhattacharjee S, Khanna P. Evaluation of i-gel™ airway in children: a meta-analysis. Paediatr Anaesth 2014; 24: 1072-9.
Choi GJ, Kang H, Baek CW, Jung YH, Woo YC, Cha YJ. A systematic review and meta-analysis of the i-gel® vs laryngeal mask airway in children. Anaesthesia 2014; 69: 1258-65.
Lee JR, Kim MS, Kim JT, et al. A randomised trial comparing the i-gel™ with the LMA Classic™ in children. Anaesthesia 2012; 67: 606-11.
Fukuhara A, Okutani R, Oda Y. A randomized comparison of the i-gel and the ProSeal laryngeal mask airway in pediatric patients: performance and fiberoptic findings. J Anesth 2013; 27: 1-6.
Lopez-Gil M, Brimacombe J, Keller C. A comparison of four methods for assessing oropharyngeal leak pressure with the laryngeal mask airway (LMA) in paediatric patients. Paediatr Anaesth 2001; 11: 319-21.
Park C, Bahk JH, Ahn WS, Do SH, Lee KH. The laryngeal mask airway in infants and children. Can J Anesth 2001; 48: 413-7.
Kovatsis PG, Fiadjoe JE, Stricker PA. Simple, reliable replacement of pilot balloons for a variety of clinical situations. Paediatr Anaesth 2010; 20: 490-4.
Lee JH, Cho HS, Shin WJ, Yang HS. A comparison of supraglottic airway i-gel™ vs. classic laryngeal mask airway in small children. Korean J Anesthesiol 2014; 66: 127-30.
Hughes C, Place K, Berg S, Mason D. A clinical evaluation of the I-gel™ supraglottic airway device in children. Paediatr Anaesth 2012; 22: 765-71.
Theiler LG, Kleine-Brueggeney M, Luepold B, et al. Performance of the pediatric-sized i-gel compared with the Ambu AuraOnce laryngeal mask in anesthetized and ventilated children. Anesthesiology 2011; 115: 102-10.
Jagannathan N, Sommers K, Sohn LE, et al. A randomized equivalence trial comparing the i-gel and laryngeal mask airway Supreme in children. Paediatr Anaesth 2013; 23: 127-33.
Jagannathan N, Sohn LE, Sawardekar A, et al. A randomised comparison of the self-pressurised air-Q™ intubating laryngeal airway with the LMA Unique™ in children. Anaesthesia 2012; 67: 973-9.
Whyte SD, Cooke E, Malherbe S. Usability and performance characteristics of the pediatric air-Q® intubating laryngeal airway. Can J Anesth 2013; 60: 557-63.
Chadd GD, Walford AJ, Crane DL. The 3.5/4.5 modification for fiberscope-guided tracheal intubation using the laryngeal mask airway. Anesth Analg 1992; 75: 307-8.
Weiss M, Goldmann K. Caution when using cuffed tracheal tubes for fibreoptic intubation through paediatric-sized laryngeal mask airways. Acta Anaesthesiol Scand 2004; 48: 523.
Disclosure
None of the authors have any affiliations that may be perceived to be conflicts of interest with the submitted material.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Narasimhan Jagannathan, Lisa Sohn, Andrea Huang, and Luis Sequera-Ramos participated in the conception and design of the study. Narasimhan Jagannathan, Lisa Sohn, Melissa Ramsey, Andrea Huang, Amod Sawardekar, and Loryn Kromrey participated in acquiring the data. Narasimhan Jagannathan, Andrea Huang, and Gildasio S. De Oliveira participated in the analysis of the data. Narasimhan Jagannathan, Lisa Sohn, Andrea Huang, and Gildasio S. De Oliveira participated in the interpretation of the data. Narasimhan Jagannathan, Lisa Sohn, Melissa Ramsey, Luis Sequera-Ramos, and Gildasio S. De Oliveira contributed to drafting the article.
Rights and permissions
About this article
Cite this article
Jagannathan, N., Sohn, L., Ramsey, M. et al. A randomized comparison between the i-gel™ and the air-Q™ supraglottic airways when used by anesthesiology trainees as conduits for tracheal intubation in children. Can J Anesth/J Can Anesth 62, 587–594 (2015). https://doi.org/10.1007/s12630-014-0304-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-014-0304-9