Abstract
SARS-CoV-2 contaminated items in the cold chain becomes a threat to public health, therefore the effective and safe sterilization method fit for the low temperature is needed. Ultraviolet is an effective sterilization method while its effect on SARS-CoV-2 under low-temperature environment is unclear. In this research, the sterilization effect of high-intensity ultraviolet-C (HIUVC) irradiation against SARS-CoV-2 and Staphylococcus aureus on different carriers at 4 °C and − 20 °C was investigated. The results showed that dose of 15.3 mJ/cm2 achieved more than 3 log reduction of SARS-CoV-2 on gauze at 4 °C and − 20 °C. The vulnerability of coronavirus to HIUVC under − 20 °C was not significantly different than those under 4 °C. Four models including Weibull, biphasic, log-linear tail and log linear were used to fit the survival curves of SARS-CoV-2 and Staphylococcus aureus. The biphasic model fitted best with R2 ranging from 0.9325 to 0.9878. Moreover, the HIUVC sterilization correlation between SARS-CoV-2 and Staphylococcus aureus was established. This paper provides data support for the employment of HIUVC under low-temperature environment. Also, it provides a method of using Staphylococcus aureus as a marker to evaluate the sterilization effect of cold chain sterilization equipment.
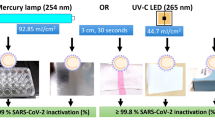
Graphical Abstract

Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) has spread worldwide since the outbreak in 2019, which causes 562,672,324 infections and 6,367,793 deaths globally according to the most recent data from the World Health Organization (WHO, 2022). Besides, the pandemic caused economic and social disruption, including employment and labor issues, trade restrictions, humanitarian crises and food security.
Cold chain plays a great role in maintaining the quality of food, extending the shelf life and cutting down the food waste (Zhao et al., 2018). While during the pandemic, the food cold chain system is at risk of becoming the medium of SARS-CoV-2 transmission and infection (He et al., 2022; Hu et al., 2021; Lu et al., 2021; Qian et al., 2022). The virus-contaminated items in cold processing, refrigeration and freezing, transportation and retailing put a risk to public health (Benkeblia, 2021). In the typical refrigeration and freezing temperature at − 20 °C, the SARS-CoV-2 on the surfaces of food packages might exist for 60 days (Liu et al., 2021). Additionally, relative humidity also affects the viability of the coronavirus (Chan et al., 2011). Over the past year, many imported cold chain products tested positive for COVID-19 at China customs. Besides, there were considerable reports of the outbreaks of COVID-19 in China traced back to the cold chain. For instance, the salmons in a sealed package in cold storage located outside Xinfadi Market in Beijing, China were tested positive for SARS-CoV-2 RNA in June, 2020 (Pang et al., 2020). Infectious SARS-CoV-2 was isolated from the outer surface of an imported frozen cod package in Qingdao, China for the first time during the outbreak in September, 2020. Therefore, Virus sterilization method for cold chain environment is needed to maintain the safety of the cold chain (Guo et al., 2022). In China, the Joint Prevention and Control Mechanism of the State Council of China issued a work plan on the preventive and comprehensive sterilization of imported cold chain food, aiming at effectively inactivating the SARS-CoV-2 during the port inspection, transportation, warehousing and retailing of imported cold chain food (National Health Commission of the People's Republic of China, 2020a). Besides, the State Council of China issued technical guidelines regulating that the inner wall of the container and the outer packaging of the goods should be disinfected (National Health Commission of the People's Republic of China, 2020b). Currently, chemical disinfects are majorly adopted as a sterilization method at customs. However, chemical disinfects are harmful to operators, have the risk of residues and food contamination, and require high intensity labor. Quick, effective and safe sterilization methods fit for the cold environment are urgently needed to establish a safe cold chain system (Chitrakar et al., 2021).
High-intensity ultraviolet-C (HIUVC) sterilization is an effective technology for the sterilization of pathogens on surfaces. According to Terms of ultraviolet disinfection technology (GB/T 32092-2015) released by The Standardization Administration of China, low pressure high intensity ultraviolet-C lamp refers to the “mercury vapor lamp that the input electric power is about 0.5–1.5 W per centimeter of arc length, and the output power of germicidal ultraviolet light is about 0.15–0.45 W per centimeter of arc length”. At same dose, it can sterilize the virus at short time, which is beneficial to its application to sterilization scene such as custom, hospital and public transport. Ultraviolet photons damaged the nucleic acid and microorganismal proteins, thus preventing viruses from replicating (Raeiszadeh & Adeli, 2020). Ultraviolet is divided into UVA (320–400 nm), UVB (280–320 nm) and UVC (200–280 nm) according to the spectrum (Darnell et al., 2004). Ultraviolet has been experimentally demonstrated an effective sterilization method against bacteria (Kim & Hung, 2012), SARS-CoV-1 (Duan et al., 2003; Kariwa et al., 2006), HCoV-OC43 (Gerchman et al., 2020). After the outbreak of COVID-19, some studies have been conducted on ultraviolet sterilization of SARS-CoV-2. Generally, the dose required to reach the same effect of inactivation of SARS-CoV-2 increases with the increase of ultraviolet wavelength (Gerchman et al., 2020; Minamikawa et al., 2021; Trivellin et al., 2021b). Therefore, UVC is an efficient sterilization method against SARS-CoV-2. Research on the sterilization effect of UVC on suspension and different carriers has been conducted (Biasin et al., 2021; Bormann et al., 2021; Fischer et al., 2020; Gerchman et al., 2020; Sabino et al., 2020; Storm et al., 2020; Trivellin et al., 2021a). Although significant progress has been made on the sterilization effect of ultraviolet on SARS-CoV-2, the effect under low temperatures is rarely investigated. Also, the comparison of UVC sterilization effect on SARS-CoV-2 and bacteria under low temperatures is absent.
In this study, Staphylococcus aureus (S.aureus) was chosen as the bacteria to establish the correlation between SARS-CoV-2 and bacteria because it is easily accessed. Based on the established correlation, S. aureus can be used to evaluate the sterilization effect of sterilization equipment.
The study aimed to experimentally evaluate the inactivation effect of HIUVC against SARS-CoV-2 and S. aureus under 4 °C and − 20 °C, which are typical temperatures of the cold chain. The HIUVC sterilization correlation between S. aureus and SARS-CoV-2 was also established.
Materials and Methods
Instruments
The U-shape high-intensity low pressure high intensity ultraviolet-C lamp (GZW250D28W-Z810) with a peak spectrum of 254 nm, is provided by Foshan Comwin Light & Electricity Co., Ltd in Guangdong, China. Two lamps were put in a self-designed apparatus that controlled the exposure time of test samples, as shown in Fig. 1. The apparatus consists of an exposure part and a power supply. The power supply was separated from the lamp to avoid the generation of virus aerosol by the heat dissipation fan in the power supply. As shown in exploded view in Fig. 1, there were two U-type HIUVC lamps of 412 W in the exposure part. The test sample was placed below the light. The ultraviolet irradiance of the light is measured by an ultraviolet irradiance meter (ST 512, SENTRY, Taiwan, China) with the range of 0.01–40.00 mW/cm2 at a response spectrum of 220–275 nm. The sample was placed on the lifting platform. The height of the lift table was adjusted to make the irradiance reach 5.1 mW/cm2, which was evenly distributed in the 2 cm × 2 cm rectangular area with deviation of ± 0.1 mW/cm2. The shutter system was connected to the motor to control the exposure time to keep the lamp output stable. Ultraviolet protective clothes and face masks were worn to avoid the harm of ultraviolet to the skin and eyes of the operators.
Virus and Cell Preparation
SARS-CoV-2 isolate (nCoV-2019BetaCoV/Wuhan/WIV04/2019) was obtained from Wuhan Institute of Virology, Chinese Academy of Sciences. The virus sterilization experiment was conducted in the biosafety level-3 (BSL-3) laboratory at National Biosafety Laboratory, Wuhan. The relative humidity in laboratory was in the range of 40–60%. The virus was propagated in Vero E6 cells cultured in Dulbecco’s modified Eagle’s medium (DMEM, Gibco, USA) supplemented with 10% fetal bovine serum (FBS, Gibco, USA). On day 2 post-infection, the culture supernatant was harvested and filtered for virus stocks and tittered through plaque assay. Medical gauze was selected as carrier for microorganism contamination. The size of the carrier is 2.0 × 2.0 cm with one layer, which was sterilized by 121 °C steam and dried before it was inoculated with the microorganism.
A drip of 200 μL SARS-CoV-2 was dropped on the gauze in a 35 mm dish (Thermo Fisher Scientific, USA). The inoculum was absorbed into the gauze as it was absorbent. The samples were kept in refrigerator (Haier, China) of 4 °C and − 20 °C for 30 min before HIUVC exposure, separately. Then, the 4 °C and − 20 °C samples were put on precooled ice storage plate. Immediately, the samples were exposed to HIUVC at the irradiance of 5.1 mW/cm2 for 1 s, 3 s and 5 s, respectively. The control group was put in dark place. The control group went through same time with the HIUVC treated group under same temperature. Subsequently, virus samples were transferred aseptically to a centrifuge tube of 50 mL (Corning Life Science, USA). Remaining virus in the dish was eluted with 2 mL DMEM, and transferred to the centrifuge tube mentioned above. The tube was whirled in a vortex mixer with the maximum speed of 5 s/time five times. The virus titer was determined by plaque assay. The experiments were conducted in triplicates.
The virus titer was determined by plaque assay as described previously (Lin et al, 2022). Briefly, virus samples were tenfold serial diluted with DMEM. Then, 200 μL of each dilution was incubated with Vero E6 cells. For HIUVC treated samples in which virus titer may be very low, 600 μL of non-diluted samples were directly used for cell infection. After one hour, cells were washed and incubated in an overlay medium containing DMEM supplemented with 2% FBS and 0.9% carboxymethyl cellulose (Calbiochem, USA). Cells were further cultured for 96 h and then fixed with paraformaldehyde (4% in PBS) and stained with crystal violet solution (1% in water. Sigma-aldrich, Germany) for visualizing plaques. Virus titer was calculated in plaque-forming units (PFU) per milliliter. Ideally, the method could detect at least one plaque in 600 μL of the non-diluted sample, the detection limit in this study is 1.67 pfu/ml. That is, 3.33 pfu in the gauze.
The S. aureus sterilization experiment was conducted in the Test Center of Antimicrobial Materials, Technical Institute of Physics and Chemistry. The relative humidity in laboratory was in the range of 40–60%. The S. aureus was inoculated from tryptic soy agar plate medium (Beijing Land Bridge Technology Co,. LTD, Beijing, China) stored in 4 °C to a new tryptic soy agar plate medium and was incubated at 37 °C for 24 h for activation. S. aureus suspension was made by inoculating S. aureus from activated tryptic soy agar plate medium into a solution made of 25 mL nutrient broth (Beijing Land Bridge Technology Co,. LTD, Beijing, China), 97.5 mL saline and 2 g Tween (GF, Hong Kong, China). Then the suspension was serially diluted. Then bovine serum albumin (Beijing Solarbio Science & Technology Co., Ltd., Beijing, China) was added to the S. aureus solution to reach concentration of 3%. A drip of 75 μL prepared S. aureus (ATCC 6538) was dropped on the gauze. Subsequently, the samples were treated with the same temperature and HIUVC irradiation condition as those contaminated with SARS-CoV-2. After irradiation, samples of S. aureus were assayed by standard pour plate procedures. The samples were massaged with 10 mL 0.03 M phosphate-buffered saline (pH 7.4, Beijing chemistry industry group Co., Ltd., Beijing, China) and serially diluted with sterile saline solution. Molten plate count agar was poured into petri dish containing 1 mL of diluted sample. The solid medium was incubated at 37 °C for 24 h for plate count.
Each experiment with different conditions was repeated 3 times to assure the repeatability. The single-factor analysis of variance and Scheffe’s test were used to test the significant differences among means at p < 0.05.
Modelling of Survival Curves
The survival curves of SARS-CoV-2 and S. aureus were fitted with four typical models via least-squares regression using GInaFit, a freeware capable of modelling microbial survival (Geeraerd et al., 2005). Four typical models are (1) Weibull model, (2) Biphasic model, (3) log linear-tail model, and (4) log linear model.
The Weibull model is described by equation. (Mafart et al., 2002)
where N is the number of surviving microorganism, cfu/pfu, N0 is the initial number of microorganism, t is ultraviolet exposure time, minute. And α is the time when the microorganism reduces from N0 to N0/10, and β is a shape parameter. The survival curve is downward concave when β > 1 and upward concave when β < 1.
The biphasic model (Kowalski, 2009) is described as:
where f is UV resistant fraction. And kmax1 and kmax2 are slopes of the biphasic curves, respectively. They are the rate constant of stage 1 and stage 2, respectively.
The log linear model (Kowalski, 2009) is described by equation
where kmax is the inactivation rate.
The log linear-tail model (Geeraerd et al., 2000) is described as:
where Nres refers to subpopulation. And kmax means the inactivation rate of the linear part of the survival curve.
The mean square error (MSE) and regression coefficient (R2) and were analyzed to evaluate the goodness of the fit of the 4 model. Besides, dose of achieving 3 log reduction of microorganism (D3d) by HIUVC treatment of 4 models were computed by the Goal Seek function in Microsoft Excel 365.
Results and Discussion
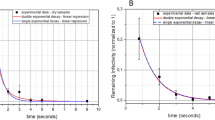
The recovery rate of SARS-CoV-2 based was 18.5% under 4 °C and 8.0% under − 20 °C, respectively. The freeze–thaw cycle might cause the reduction of virus titre, resulting in relatively low recovery rate. The recovery rate of S. aureus was approximate 100% for both 4 °C and − 20 °C. Nevertheless, in both the SARS-CoV-2 and the S. aureus experiment, HIUVC showed a high sterilization effect when comparing the treated samples with the non-treated control. The sterilization effect of HIUVC on SARS-CoV-2 under 4 °C and − 20 °C is shown in Fig. 2. Limit of detection was recorded was 3.33 pfu. Degree of 4 °C is the typical storage temperature for chilled foods and − 20 °C for frozen foods. It is shown that the pfu of SARS-CoV-2 decreased with the increase of exposure time under HIUVC. The dose of HIUVC required at least 15.3 mJ/cm2 to reach 3 log reduction. The dose was larger than the liquid virus reported by Sabino et al. (2020) (6.556 mJ/cm2) and Biasin et al. (2021) (5.4 mJ/cm2), which were conducted in room temperature. The larger dose in this study might attribute to the shadowing effects of the gauze compared to the aqueous results. For 4 °C, when exposure time increased from 3 to 5 s, there was no significant reduction (p < 0.05) of SARS-CoV-2 due to the shadow effects of the gauze. In the survival curve fitted by biphasic model showed in Fig. 4b, this trend is clearer. This trend was in accordance with the research conducted by Darnell et al. (2004). They investigated the UVC on SARS-CoV-1, and the results showed that when the UVC dose exceeded a certain value, no additional inactivation was observed. The dose required to achieve 3 log reduction based on biphasic model was 8.9 mJ/cm2 for 4 °C and − 20 °C, which was smaller than those reported by Bormann et al. conducted at room temperature (Bormann et al., 2021). Their results showed that more than 14.7 mJ/cm2 was needed under irradiance of 0.245 mW/cm2 for carriers of glass, metal, and plastic. This difference might attribute to the lower intensity of the LED lamp or the difference of carrier material or temperature between their research and this study.
The comparison of the sterilization effect of HIUVC on S. aureus and SARS-CoV-2 is shown in Fig. 3. The detection limit of S. aureus was 10 cfu. Data group with shared superscript letter indicated the there is no statistical significance between these two groups, otherwise they show statistical significance (p < 0.05). The temperature did not have a significant effect on the HIUVC sterilization of SARS-CoV-2 and S. aureus between − 20 °C and 4 °C (p < 0.05), which is similar to the research on other microbes (Severin et al., 1983). As coronavirus has a simpler structure than bacteria, it might be more vulnerable to HIUVC compared to S. aureus (Khan et al., 2022). The effect is significant when the HIUVC doses were 15.3 mJ/cm2 at 3 s and 25.5 mJ/cm2 at 5 s (p < 0.05).
The HIUVC sterilization relation between S. aureus and SARS-CoV-2 was established. Four typical mathematical model were used to fit the microbial survival curves after HIUVC treatment, as shown in Fig. 4. The range of HIUVC treating time was 0–5 s (0–15.5 mJ/cm2). The fit goodness is shown in Table 1. The results showed that biphasic model fitted the survival of S. aureus and SARS-CoV-2 better with larger R2 and lower MSE.
Biphasic model was used to establish the correlation between HIUVC sterilization effect against SARS-CoV-2 and S. aureus on gauze. At the same dose, the log reduction of SARS-CoV-2 and S. aureus were computed based on 101 evenly distributed points between 5.1 and 15.3 mJ/cm2. These data were plotted in Fig. 5. The reduction ranges of S. aureus and SARS-CoV-2 in Fig. 5 were within the range of experimental data. According to the graph, once the sterilization effect of the known HIUVC dose ranging from 5.1 to 15.3 mJ/cm2 against S. aureus on gauze is known, the sterilization effect of the same HIUVC dose against the SARS-CoV-2 on gauze with BSA added under the same temperature can be derived. Therefore, with the help of the sterilization relationship between S. aureus and SARS-CoV-2, S. aureus can be used to detect the sterilization effect of large-scale ultraviolet sterilization equipment at the sterilization site, avoiding the complicated operation of the SARS-CoV-2 and the need for specialized laboratories. It is worth noted that the correlation may not be applicable under the different surface conditions, however, UVC manufacturers could use this method to quantify dose–response curves for SARS-CoV-2 on various surfaces. That is, they could use bacteria to test the UVC sterilization effect based on the correlation with SARS-CoV-2 on various surfaces established in laboratory. The current study chose gauze as microorganism carriers, which can provide a reference to SARS-CoV-2 sterilization on food packages such as plastic, glass, paper, board, and metal under 4 °C and − 20 °C. Porous surfaces required higher doses of ultraviolet than non-porous surfaces to reach same log reduction of SARS-CoV-2 (Tomás et al., 2022). Gauze was a porous carrier, which was more difficult to sterilize than non-porous food packages such as plastic, glass and metal.
Conclusion
This study acquired the sterilization data of HIUVC against the SARS-CoV-2 virus under low-temperature conditions for the first time. The dose of 15.3 mJ/cm2 of HIUVC achieved 3 log reduction of SARS-CoV-2 on gauze under 4 °C and − 20 °C with 3 s. The HIUVC sterilization effect of SARS-CoV-2 did not vary significantly with the change in temperature. HIUVC rapidly sterilized SARS-CoV-2 on gauze under typical cold chain temperature. Also, the sterilization effect of HIUVC on SARS-CoV-2 was compared with S. aureus under low temperatures. Weibull, biphasic, log-linear tail and log linear models were used to fit the survival curves of SARS-CoV-2 and S. aureus. The biphasic model fitted best with R2 of 0.9325–0.9878. The corresponding relation between HIUVC sterilization effect against them was established. These data provide evidence support for the application of HIUVC in cold chain. Moreover, the proposed correlation could provide a method for using bacteria as a substitute to test the sterilization effect of sterilization equipment against SARS-CoV-2, cutting off the spread of COVID-19 through the cold chain.
Data Availability
The datasets generated during the current study are available in the Science Data Bank repository, http://doi.org/10.57760/sciencedb.01917
References
Benkeblia, N. (2021). In the landscape of SARS-CoV-2 and fresh fruits and vegetables: The fake and hidden transmission risks. Journal of Food Safety, 41(4), e12898. https://doi.org/10.1111/jfs.12898
Biasin, M., Bianco, A., Pareschi, G., Cavalleri, A., Cavatorta, C., Fenizia, C., Galli, P., Lessio, L., Lualdi, M., Tombetti, E., Ambrosi, A., Redaelli, E. M. A., Saulle, I., Trabattoni, D., Zanutta, A., & Clerici, M. (2021). UV-C irradiation is highly effective in inactivating SARS-CoV-2 replication. Scientific Reports, 11(1), 6260. https://doi.org/10.1038/s41598-021-85425-w
Bormann, M., Alt, M., Schipper, L., van de Sand, L., Otte, M., Meister, T. L., Dittmer, U., Witzke, O., Steinmann, E., & Krawczyk, A. (2021). Disinfection of SARS-CoV-2 contaminated surfaces of personal items with UVC-LED disinfection boxes. Viruses, 13(4), 598. https://doi.org/10.3390/v13040598
Chan, K. H., Peiris, J. S. M., Lam, S. Y., Poon, L. L. M., Yuen, K. Y., & Seto, W. H. (2011). The effects of temperature and relative humidity on the viability of the SARS coronavirus. Advances in Virology, 2011, e734690. https://doi.org/10.1155/2011/734690
Chitrakar, B., Zhang, M., & Bhandari, B. (2021). Improvement strategies of food supply chain through novel food processing technologies during COVID-19 pandemic. Food Control, 125, 108010. https://doi.org/10.1016/j.foodcont.2021.108010
Darnell, M. E. R., Subbarao, K., Feinstone, S. M., & Taylor, D. R. (2004). Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. Journal of Virological Methods, 121(1), 85–91. https://doi.org/10.1016/j.jviromet.2004.06.006
Duan, S. M., Zhao, X., Wen, R. F., Huang, J. J., Pi, G. H., Zhang, S. X., Han, J., Bi, S. L., Ruan, L., Dong, X. P., Team SR. (2003). Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomedical and Environmental Sciences, 16(3), 246–255.
Fischer, R., Morris, D., van Doremalen, N., Sarchette, S., Matson, M. J., Bushmaker, T., Yinda, C. K., Seifert, S., Gamble, A., Williamson, B., Judson, S., de Wit, E., Lloyd-Smith, J., & Munster, V. (2020). Effectiveness of N95 respirator decontamination and reuse against SARS-CoV-2 virus. Emerging Infectious Disease Journal, 26(9), 2253. https://doi.org/10.3201/eid2609.201524
Geeraerd, A. H., Herremans, C. H., & Van Impe, J. F. (2000). Structural model requirements to describe microbial inactivation during a mild heat treatment. International Journal of Food Microbiology, 59(3), 185–209. https://doi.org/10.1016/S0168-1605(00)00362-7
Geeraerd, A. H., Valdramidis, V. P., & Van Impe, J. F. (2005). GInaFiT, a freeware tool to assess non-log-linear microbial survivor curves. International Journal of Food Microbiology, 102(1), 95–105. https://doi.org/10.1016/j.ijfoodmicro.2004.11.038
Gerchman, Y., Mamane, H., Friedman, N., & Mandelboim, M. (2020). UV-LED disinfection of coronavirus: Wavelength effect. Journal of Photochemistry and Photobiology b: Biology, 212, 112044. https://doi.org/10.1016/j.jphotobiol.2020.112044
Guo, M., Yan, J., Hu, Y., Xu, L., Song, J., Yuan, K., Cheng, X., Ma, S., Liu, J., Wu, X., Liu, L., Rong, S., & Wang, D. (2022). Transmission of SARS-CoV-2 on cold-chain food: Precautions can effectively reduce the risk. Food and Environmental Virology. https://doi.org/10.1007/s12560-022-09521-4
He, X., Liu, X., Li, P., Wang, P., Cheng, H., Li, W., Li, B., Liu, T., & Ma, J. (2022). A multi-stage green barrier strategy for the control of global SARS-CoV-2 transmission via cold chain goods. Engineering, 9, 13–16. https://doi.org/10.1016/j.eng.2021.08.013
Hu, L., Gao, J., Yao, L., Zeng, L., Liu, Q., Zhou, Q., Zhang, H., Lu, D., Fu, J., Liu, Q. S., Li, M., Zhao, X., Hou, X., Shi, J., Liu, L., Guo, Y., Wang, Y., Ying, G.-G., Cai, Y., & Jiang, G. (2021). Evidence of foodborne transmission of the coronavirus (COVID-19) through the animal products food supply chain. Environmental Science & Technology, 55(5), 2713–2716. https://doi.org/10.1021/acs.est.0c06822
Kariwa, H., Fujii, N., & Takashima, I. (2006). Inactivation of SARS coronavirus by means of povidone-iodine, physical conditions and chemical reagents. Dermatology, 212(Suppl. 1), 119–123. https://doi.org/10.1159/000089211
Khan, M., McDonald, M., Mundada, K., & Willcox, M. (2022). Efficacy of ultraviolet radiations against coronavirus, bacteria, fungi, fungal spores and biofilm. Hygiene, 2(3), 120–131. https://doi.org/10.3390/hygiene2030010
Kim, C., & Hung, Y.-C. (2012). Inactivation of E. coli O157:H7 on blueberries by electrolyzed water, ultraviolet light, and ozone. Journal of Food Science, 77(4), M206–M211. https://doi.org/10.1111/j.1750-3841.2011.02595.x
Kowalski, W. (2009). Ultraviolet germicidal irradiation handbook: UVGI for air and surface disinfection. Springer. https://doi.org/10.1007/978-3-642-01999-9
Lin, X., Ke, X., Jian, X., Xia, L., Yang, Y., Zhang, T., Xiong, H., Zhao, B., Liu, W., Chen, Q., & Tang, C. (2022). Azacytidine targeting SARS-CoV-2 viral RNA as a potential treatment for COVID-19. Science Bulletin, 67(10), 1022–1025. https://doi.org/10.1016/j.scib.2022.02.002
Liu, H., Fei, C., Chen, Y., Luo, S., Yang, T., Yang, L., Liu, J., Ji, X., Wu, W., & Song, J. (2021). Investigating SARS-CoV-2 persistent contamination in different indoor environments. Environmental Research, 202, 111763. https://doi.org/10.1016/j.envres.2021.111763
Lu, L.-C., Quintela, I., Lin, C.-H., Lin, T.-C., Lin, C.-H., Wu, V. C. H., & Lin, C.-S. (2021). A review of epidemic investigation on cold-chain food-mediated SARS-CoV-2 transmission and food safety consideration during COVID-19 pandemic. Journal of Food Safety, 41(6), e12932. https://doi.org/10.1111/jfs.12932
Mafart, P., Couvert, O., Gaillard, S., & Leguerinel, I. (2002). On calculating sterility in thermal preservation methods: Application of the Weibull frequency distribution model. International Journal of Food Microbiology, 72(1), 107–113. https://doi.org/10.1016/S0168-1605(01)00624-9
Minamikawa, T., Koma, T., Suzuki, A., Mizuno, T., Nagamatsu, K., Arimochi, H., Tsuchiya, K., Matsuoka, K., Yasui, T., Yasutomo, K., & Nomaguchi, M. (2021). Quantitative evaluation of SARS-CoV-2 inactivation using a deep ultraviolet light-emitting diode. Scientific Reports, 11(1), 5070. https://doi.org/10.1038/s41598-021-84592-0
National Health Commission of the People's Republic of China. (2020a). Work Plan on the Preventive Comprehensive Sterilization of Imported Cold Chain Food. http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=26b2fafc696b48e3b2dab5cdb2fd50d9
National Health Commission of the People's Republic of China. (2020b). Technical Guidelines for Prevention, Control and Sterilization on of Coronavirus in the Production and Operation Process of Cold Chain Food. http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=ff228979f1534c3abca56559f14ea115
Pang, X., Ren, L., Wu, S., Ma, W., Yang, J., Di, L., Li, J., Xiao, Y., Kang, L., Du, S., Du, J., Wang, J., Li, G., Zhai, S., Chen, L., Zhou, W., Lai, S., Gao, L., Pan, Y., COVID-19 Laboratory Testing Group. (2020). Cold-chain food contamination as the possible origin of COVID-19 resurgence in Beijing. National Science Review, 7(12), 1861–1864. https://doi.org/10.1093/nsr/nwaa264
Qian, J., Yu, Q., Jiang, L., Yang, H., & Wu, W. (2022). Food cold chain management improvement: A conjoint analysis on COVID-19 and food cold chain systems. Food Control, 137, 108940. https://doi.org/10.1016/j.foodcont.2022.108940
Raeiszadeh, M., & Adeli, B. (2020). A critical review on ultraviolet disinfection systems against COVID-19 outbreak: Applicability, validation, and safety considerations. ACS Photonics, 7(11), 2941–2951. https://doi.org/10.1021/acsphotonics.0c01245
Sabino, C. P., Sellera, F. P., Sales-Medina, D. F., Machado, R. R. G., Durigon, E. L., Freitas-Junior, L. H., & Ribeiro, M. S. (2020). UV-C (254 nm) lethal doses for SARS-CoV-2. Photodiagnosis and Photodynamic Therapy, 32, 101995. https://doi.org/10.1016/j.pdpdt.2020.101995
Severin, B. F., Suidan, M. T., & Engelbrecht, R. S. (1983). Effect of temperature on ultraviolet light disinfection. Environmental Science & Technology, 17(12), 717–721. https://doi.org/10.1021/es00118a006
Storm, N., McKay, L. G. A., Downs, S. N., Johnson, R. I., Birru, D., de Samber, M., Willaert, W., Cennini, G., & Griffiths, A. (2020). Rapid and complete inactivation of SARS-CoV-2 by ultraviolet-C irradiation. Scientific Reports, 10(1), 22421. https://doi.org/10.1038/s41598-020-79600-8
Tomás, A. L., Reichel, A., Silva, P. M., Silva, P. G., Pinto, J., Calado, I., Campos, J., Silva, I., Machado, V., Laranjeira, R., Abreu, P., Mendes, P., Sedrine, N. B., & Santos, N. C. (2022). UV-C irradiation-based inactivation of SARS-CoV-2 in contaminated porous and non-porous surfaces. Journal of Photochemistry and Photobiology b: Biology. https://doi.org/10.1016/j.jphotobiol.2022.112531
Trivellin, N., Buffolo, M., Onelia, F., Pizzolato, A., Barbato, M., Orlandi, V. T., Del Vecchio, C., Dughiero, F., Zanoni, E., Meneghesso, G., Crisanti, A., & Meneghini, M. (2021a). Inactivating SARS-CoV-2 using 275 nm UV-C LEDs through a spherical irradiation box: Design, characterization and validation. Materials, 14(9), 2315. https://doi.org/10.3390/ma14092315
Trivellin, N., Piva, F., Fiorimonte, D., Buffolo, M., De Santi, C., Orlandi, V. T., Dughiero, F., Meneghesso, G., Zanoni, E., & Meneghini, M. (2021b). UV-based technologies for SARS-CoV2 inactivation: Status and perspectives. Electronics, 10(14), 1703. https://doi.org/10.3390/electronics10141703
WHO. (2022). World Health Organization. https://covid19.who.int/, Accessed 21 July 2022.
Zhao, H., Liu, S., Tian, C., Yan, G., & Wang, D. (2018). An overview of current status of cold chain in China. International Journal of Refrigeration, 88, 483–495. https://doi.org/10.1016/j.ijrefrig.2018.02.024
Acknowledgements
This study was supported by the National Natural Science Foundation of China (No. 51976232) and the Director's Fund of the Technical Institute of Physics and Chemistry, CAS.
Author information
Authors and Affiliations
Contributions
Conceptualization: CT; Methodology: HZ, QC; Formal analysis and investigation: PL, XK, DL, XL, WY, HZ; Writing-original draft preparation: PL; Writing-review and editing: XK, HZ; Funding acquisition: CT, HZ; Resources: HX; Supervision: HZ, CT, QC; Project administration: CT; Validation: HX.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, P., Ke, X., Leng, D. et al. High-Intensity Ultraviolet-C Irradiation Efficiently Inactivates SARS-CoV-2 Under Typical Cold Chain Temperature. Food Environ Virol 15, 123–130 (2023). https://doi.org/10.1007/s12560-023-09552-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12560-023-09552-5