Abstract
Background
Previous research has demonstrated that both sleep and physical activity (PA) are independently associated with various indicators of mental health among adults. However, their joint contribution to mental health has received limited attention. The present study used cross-sectional data from the Mental Health Million Project to examine the independent and joint effects of sleep and PA on mental health among a global sample of adults, and whether these effects differ among individuals receiving mental health treatment.
Method
The sample included 200,743 participants (33.1% young adults, 45.6% middle-aged adults, 21.3% older adults; 57.6% females, 0.9% other) from 213 countries, territories, and archipelagos worldwide that completed a comprehensive 47-item assessment of mental health including both problems (i.e., ill-being) and assets (i.e., well-being): the Mental Health Quotient. Participants also reported their weekly frequency of PA and adequate sleep, and mental health treatment status. A series of generalized linear mixed models were computed.
Results
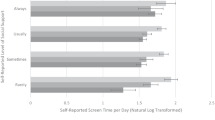
Independent dose-response associations were observed, whereby greater amounts of PA and adequate sleep were each associated with better mental health. In addition, a synergistic interaction was observed in which the positive correlation of PA with mental health was strengthened with greater frequency of adequate sleep. These benefits were less pronounced among adults receiving mental health treatment.
Conclusion
While findings suggest sleep can help to offset the negative influence of a physically inactive lifestyle (and vice versa), our results point to a “more is better” approach for both behaviors when it comes to promoting mental health.






Similar content being viewed by others
Notes
For analytic purposes, we included responses up until the release of the Arabic version of the MHQ in November 2021 as not all Arabic responses were translated into English. Pilot data collected prior to April 9, 2020, was collected using prior versions of the MHQ (versions 1.1, 1.2, 1.3) and therefore excluded. Additionally, a new version of the MHQ was launched in January 2022; and therefore, only responses on versions 2.0 through 2.8 of the MHQ were included.
A small proportion of MHQ scores fall below - 100 due to the way that the MHQ score algorithm is calculated. This procedure ensures that the negative MHQ scores are more evenly distributed across the negative score window.
References
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–50.
Santomauro DF, Herrera AMM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–12.
Bloom DE, Cafiero E, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, Fathima S, et al. The global economic burden of noncommunicable diseases. PGDA Working Papers. 2012 [cited 2022 Dec 29]. Available from: https://ideas.repec.org//p/gdm/wpaper/8712.html.
Trautmann S, Rehm J, Wittchen HU. The economic costs of mental disorders. EMBO Rep. 2016;17(9):1245–9.
Mahomed F. Addressing the problem of severe underinvestment in mental health and well-being from a human rights perspective. Health Hum Rights. 2020;22(1):35–49.
National Institutes of Health. Estimates of funding for various research, condition, and disease categories. 2022 [cited 2022 Dec 29]. Available from: https://report.nih.gov/funding/categorical-spending#/.
Firth J, Ward PB, Stubbs B. Editorial: lifestyle psychiatry. Front Psych. 2019;10:597.
World Health Organization. Investing in mental health: evidence for action. Geneva: World Health Organization; 2013 [cited 2022 Dec 29]. 32 p. Available from: https://apps.who.int/iris/handle/10665/87232.
Keyes CLM. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. 2005;73(3):539–48.
Westerhof GJ, Keyes CLM. Mental illness and mental health: the two continua model across the lifespan. J Adult Dev. 2010;17(2):110–9.
Keyes CLM. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43(2):207–22.
Walsh R. Lifestyle and mental health. Am Psychol. 2011;66:579–92.
Firth J, Solmi M, Wootton RE, Vancampfort D, Schuch FB, Hoare E, et al. A meta-review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry. 2020;19(3):360–80.
Ross R, Chaput JP, Giangregorio LM, Janssen I, Saunders TJ, Kho ME, et al. Canadian 24-Hour Movement Guidelines for Adults aged 18–64 years and Adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45(10):S57-102.
Guo Z, Li R, Lu S. Leisure-time physical activity and risk of depression: a dose-response meta-analysis of prospective cohort studies. Med (Baltimore). 2022;101(30):e29971.
Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, et al. Association between physical activity and risk of depression: a systematic review and meta-analysis. JAMA Psychiat. 2022;79(6):550–9.
Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta- analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. 2015;9(3):366–78.
Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward PB. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry. 2014;75(9):14465.
White RL, Babic MJ, Parker PD, Lubans DR, Astell-Burt T, Lonsdale C. Domain-specific physical activity and mental health: a meta-analysis. Am J Prev Med. 2017;52(5):653–66.
Wiese CW, Kuykendall L, Tay L. Get active? A meta-analysis of leisure-time physical activity and subjective well-being. J Posit Psychol. 2018;13(1):57–66.
Netz Y, Wu MJ, Becker BJ, Tenenbaum G. Physical activity and psychological well-being in advanced age: a meta-analysis of intervention studies. Psychol Aging. 2005;20(2):272–84.
Santos AC, Willumsen J, Meheus F, Ilbawi A, Bull FC. The cost of inaction on physical inactivity to public health-care systems: a population-attributable fraction analysis. Lancet Glob Health. 2023;11(1):e32–9.
Dunn AL, Jewell JS. The effect of exercise on mental health. Curr Sports Med Rep. 2010;9(4):202.
Tremblay MS, Ross R. How should we move for health? The case for the 24-hour movement paradigm. CMAJ. 2020;192(49):E1728–9.
Rosenberger ME, Fulton JE, Buman MP, Troiano RP, Grandner MA, Buchner DM, et al. The 24-hour activity cycle: a new paradigm for physical activity. Med Sci Sports Exerc. 2019;51(3):454–64.
Groves CI, Huong C, Porter CD, Summerville B, Swafford I, Witham B, Brown DM (2024) Associations between 24-h movement behaviors and indicators of mental health and well-being across the lifespan: a systematic review. J Activity Sedentary Sleep Behav. 2024;3(1):1–51.
Merlo G, Vela A. Mental health in lifestyle medicine: a call to action. Am J Lifestyle Med. 2022;16(1):7–20.
Chaput JP, Dutil C, Featherstone R, Ross R, Giangregorio L, Saunders TJ, et al. Sleep timing, sleep consistency, and health in adults: a systematic review. Appl Physiol Nutr Metab. 2020;45(10):S232-47.
Faulkner S, Bee P. Perspectives on sleep, sleep problems, and their treatment, in people with serious mental illnesses: a systematic review. PLoS One. 2016;11(9):e0163486.
Grandner MA. The cost of sleep lost: implications for health, performance, and the bottom line. Am J Health Promot. 2018;32(7):1629–34.
Bacaro V, Miletic K, Crocetti E. A meta-analysis of longitudinal studies on the interplay between sleep, mental health, and positive well-being in adolescents. Int J Clin Health Psychol. 2024;24(1): 100424.
Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev. 2021;60: 101556.
Kobayashi I, Boarts JM, Delahanty DL. Polysomnographically measured sleep abnormalities in PTSD: a meta-analytic review. Psychophysiol. 2007;44(4):660–9.
Hafner M, Stepanek M, Taylor J, Troxel WM, van Stolk C. Why sleep matters—the economic costs of insufficient sleep. Rand Health Q. 2017;6(4):11.
Ernstsen L, Havnen A. Mental health and sleep disturbances in physically active adults during the COVID-19 lockdown in Norway: does change in physical activity level matter? Sleep Med. 2021;77:309–12.
Gillis BT, El-Sheikh M. Sleep and adjustment in adolescence: physical activity as a moderator of risk. Sleep Health. 2019;5(3):266–72.
Ogawa S, Kitagawa Y, Fukushima M, Yonehara H, Nishida A, Togo F, et al. Interactive effect of sleep duration and physical activity on anxiety/depression in adolescents. Psychiatry Res. 2019;273:456–60.
Wang X, Di J, Zhao G, Wang L, Zhang X. Association of nighttime sleep duration with depressive symptoms and its interaction with regular physical activity among Chinese adolescent girls. Int J Environ Res Public Health. 2021;18:11199.
Xiang S, Dong J, Li X, Li L. Association between sleep duration, physical activity, and mental health disorders: a secondary analysis of the National Survey of Children’s Health 2017–2018. Biomed Res Int. 2021;2021: e5585678.
Zhang Y, Liu J, Zhang Y, Ke L, Liu R. Interactive compensation effects of physical activity and sleep on mental health: a longitudinal panel study among Chinese college students during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19:12323.
Wickham SR, Amarasekara NA, Bartonicek A, Conner TS. The big three health behaviors and mental health and well-being among young adults: a cross-sectional investigation of sleep, exercise, and diet. Front Psychol. 2020 [cited 2023 Dec 11];11. Available from: https://www.frontiersin.org/articles/10.3389/fpsyg.2020.579205.
Cheval B, Maltagliati S, Sieber S, Cullati S, Sander D, Boisgontier MP. Physical inactivity amplifies the negative association between sleep quality and depressive symptoms. Prev Med. 2022;164: 107233.
Shannon S, Carlin A, Woods C, Nevill AM, Murphy N, Murphy MH. Adherence to aerobic and muscle-strengthening components of the physical activity guidelines and mental health. Health Promot Int. 2022;37(5):daac083.
De Cocker K, Teychenne M, White RL, Bennie JA. Adherence to aerobic and muscle-strengthening exercise guidelines and associations with psychological distress: a cross-sectional study of 14,050 English adults. Prev Med. 2020;139: 106192.
Patte KA, Faulkner G, Qian W, Duncan M, Leatherdale ST. Are one-year changes in adherence to the 24-hour movement guidelines associated with depressive symptoms among youth? BMC Public Health. 2020;20(1):793.
van den Berg JF, van den, Luijendijk HJ, Tulen JHM, Hofman A, Neven AK, Tiemeier H. Sleep in depression and anxiety disorders: a population-based study of elderly persons. J Clin Psychiatry. 2009;70(8):19689.
Sun X, Zheng B, Lv J, Guo Y, Bian Z, Yang L, et al. Sleep behavior and depression: findings from the China Kadoorie Biobank of 0.5 million Chinese adults. J Affect Disord. 2018;229:120–4.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fifth Edition. American Psychiatric Association; 2013 [cited 2021 Apr 28]. Available from: http://psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596.
International Classification of Diseases (ICD). [cited 2023 Dec 12]. Available from: https://www.who.int/standards/classifications/classification-of-diseases.
Borsboom D, Cramer AOJ, Schmittmann VD, Epskamp S, Waldorp LJ. The small world of psychopathology. PLoS One. 2011;6(11):e27407.
Newson JJ, Pastukh V, Thiagarajan TC. Poor separation of clinical symptom profiles by DSM-5 disorder criteria. Front Psychiatry. 2021;12:775762.
Wakefield JC. Diagnostic issues and controversies in DSM-5: return of the false positives problem. Annu Rev Clin Psychol. 2016;12:105–32.
Wakefield JC, First MB. Clarifying the boundary between normality and disorder: a fundamental conceptual challenge for psychiatry. Can J Psychiatry. 2013;58(11):603–5.
Cooper RV. Avoiding false positives: zones of rarity, the threshold problem, and the DSM clinical significance criterion. Can J Psychiatry. 2013;58(11):606–11.
Rössler W. What is normal? The impact of psychiatric classification on mental health practice and research. Front Public Health. 2013;1:68.
Schuch F, Vancampfort D, Firth J, Rosenbaum S, Ward P, Reichert T, et al. Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta-analysis. J Affect Disord. 2017;210:139–50.
Chekroud SR, Gueorguieva R, Zheutlin AB, Paulus M, Krumholz HM, Krystal JH, et al. Association between physical exercise and mental health in 1·2 million individuals in the USA between 2011 and 2015: a cross-sectional study. The Lancet Psychiatry. 2018;5(9):739–46.
Newson JJ, Thiagarajan TC. Assessment of population well-being with the Mental Health Quotient (MHQ): development and usability study. JMIR Mental Health. 2020;7(7):e17935.
Newson JJ, Pastukh V, Thiagarajan TC. Assessment of population well-being with the Mental Health Quotient: validation study. JMIR Mental Health. 2022;9(4):e34105.
Newson JJ, Hunter D, Thiagarajan TC. The heterogeneity of mental health assessment. Front Psych. 2020;11:76.
Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the National Comorbidity Survey-Adolescent Supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. 2015;54(1):37-44.e2.
Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380(9838):258–71.
Oftedal S, Vandelanotte C, Duncan MJ. Patterns of diet, physical activity, sitting and sleep are associated with socio-demographic, behavioural, and health-risk indicators in adults. Int J Environ Res Public Health. 2019;16(13):E2375.
Reading Turchioe M, Grossman LV, Myers AC, Pathak J, Creber RM. Correlates of mental health symptoms among US adults during COVID-19, March–April 2020. Public Health Rep. 2021;136(1):97–106.
Jacobi F, Höfler M, Siegert J, Mack S, Gerschler A, Scholl L, et al. Twelve-month prevalence, comorbidity and correlates of mental disorders in Germany: the Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH). Int J Methods Psychiatr Res. 2014;23(3):304–19.
van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67.
Woods AD, Gerasimova D, Van Dusen B, Nissen J, Bainter S, Uzdavines A, et al. Best practices for addressing missing data through multiple imputation. Infant Child Dev. 2024;33(1):e2407.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–99.
Lumley T. Analysis of complex survey samples. J Stat Softw. 2004;9:1–19.
Tabachnick BG, Fidell LS. Using multivariate statistics. 7th ed. Boston, MA: Pearson; 2019.
Bellavia A, Åkerstedt T, Bottai M, Wolk A, Orsini N. Sleep duration and survival percentiles across categories of physical activity. Am J Epidemiol. 2014;179(4):484–91.
Chen LJ, Hamer M, Lai YJ, Huang BH, Ku PW, Stamatakis E. Can physical activity eliminate the mortality risk associated with poor sleep? A 15-year follow-up of 341,248 MJ Cohort participants. J Sport Health Sci. 2022;11(5):596–604.
Huang BH, Duncan MJ, Cistulli PA, Nassar N, Hamer M, Stamatakis E. Sleep and physical activity in relation to all-cause, cardiovascular disease and cancer mortality risk. Br J Sports Med. 2021;56:718–24.
Wennman H, Kronholm E, Heinonen OJ, Kujala UM, Kaprio J, Partonen T, et al. Leisure time physical activity and sleep predict mortality in men irrespective of background in competitive sports. Prog Prev Med. 2017;2(6):e0009.
Cassidy S, Chau JY, Catt M, Bauman A, Trenell MI. Cross-sectional study of diet, physical activity, television viewing and sleep duration in 233,110 adults from the UK Biobank; the behavioural phenotype of cardiovascular disease and type 2 diabetes. BMJ Open. 2016;6(3): e010038.
Oftedal S, Holliday EG, Reynolds AC, Bennie JA, Kline CE, Duncan MJ. Prevalence, trends, and correlates of joint patterns of aerobic and muscle-strengthening activity and sleep duration: a pooled analysis of 359,019 adults in the National Health Interview Survey 2004–2018. J Phys Act Health. 2022;19(4):246–55.
Valenzuela PL, Santos-Lozano A, Morales JS, Castillo-García A, Lucia A. Association between self-reported sleep characteristics and cardiovascular risk factors: weight status and physical activity matter. Eur J Sport Sci. 2023;23(6):1028–35.
Brown DMY, Porter C, Hamilton F, Almanza F, Narvid C, Pish M, et al. Interactive associations between physical activity and sleep duration in relation to adolescent academic achievement. Int J Environ Res Public Health. 2022;19:15604.
Cairney J, Veldhuizen S, Vigod S, Streiner DL, Wade TJ, Kurdyak P. Exploring the social determinants of mental health service use using intersectionality theory and CART analysis. J Epidemiol Community Health. 2014;68(2):145–50.
Urbanoski KA, Cairney J, Bassani DG, Rush BR. Perceived unmet need for mental health care for Canadians with co-occurring mental and substance use disorders. Psychiatr Serv. 2008;59(3):283–9.
Roberts T, Miguel Esponda G, Krupchanka D, Shidhaye R, Patel V, Rathod S. Factors associated with health service utilisation for common mental disorders: a systematic review. BMC Psychiatry. 2018;18(1):262.
Malhi GS, Bassett D, Boyce P, Bryant R, Fitzgerald PB, Fritz K, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry. 2015;49(12):1087–206.
National Institute for Health and Care Excellence. Depression in adults: treatment and management. NICE; 2022 [cited 2023 Jan 4]. Available from: https://www.nice.org.uk/guidance/ng222.
Ravindran AV, Balneaves LG, Faulkner G, Ortiz A, McIntosh D, Morehouse RL, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 5. Complementary and alternative medicine treatments. Can J Psychiatry. 2016;61(9):576–87.
Stubbs B, Vancampfort D, Hallgren M, Firth J, Veronese N, Solmi M, et al. EPA guidance on physical activity as a treatment for severe mental illness: a meta-review of the evidence and Position Statement from the European Psychiatric Association (EPA), supported by the International Organization of Physical Therapists in Mental Health (IOPTMH). Eur Psychiatry. 2018;54:124–44.
Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32(5):541–56.
Brunner DP, Dijk DJ, Tobler I, Borbély AA. Effect of partial sleep deprivation on sleep stages and EEG power spectra: evidence for non-REM and REM sleep homeostasis. Electroencephalogr Clin Neurophysiol. 1990;75(6):492–9.
Pace-Schott EF, Germain A, Milad MR. Sleep and REM sleep disturbance in the pathophysiology of PTSD: the role of extinction memory. Biol Mood Anxiety Disord. 2015;5:3.
Pace-Schott EF, Germain A, Milad MR. Effects of sleep on memory for conditioned fear and fear extinction. Psychol Bull. 2015;141(4):835–57.
Atoui S, Chevance G, Romain AJ, Kingsbury C, Lachance JP, Bernard P. Daily associations between sleep and physical activity: a systematic review and meta-analysis. Sleep Med Rev. 2021;57: 101426.
Borsboom D, Deserno MK, Rhemtulla M, Epskamp S, Fried EI, McNally RJ, et al. Network analysis of multivariate data in psychological science. Nat Rev Methods Primers. 2021;1(1):1–18.
Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71:1–14.
Teychenne M, Ball K, Salmon J. Sedentary behavior and depression among adults: a review. IntJ Behav Med. 2010;17(4):246–54.
Hoare E, Milton K, Foster C, Allender S. The associations between sedentary behaviour and mental health among adolescents: a systematic review. Int J Behav Nutr Phys Act. 2016;13(1):108.
Smith L, Hamer M, Gardner B. Sedentary behavior and mental health. In: Stubbs B, Rosenbaum S, editors. Exercise-based interventions for mental illness. Academic Press; 2018 [cited 2023 Dec 8]. p. 107–19. Available from: https://www.sciencedirect.com/science/article/pii/B978012812605900006X.
Wainberg ML, Scorza P, Shultz JM, Helpman L, Mootz JJ, Johnson KA, et al. Challenges and opportunities in global mental health: a research-to-practice perspective. Curr Psychiatry Rep. 2017;19(5):28.
Lee JH, Huber JC. Evaluation of multiple imputation with large proportions of missing data: how much is too much? Iran J Public Health. 2021;50(7):1372–80.
Author information
Authors and Affiliations
Contributions
Conceptualization (DB), methodology (DB), formal analysis (DB), data curation (DB), writing–original draft (DB), writing–review and editing (IL, JC, MK).
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brown, D.M.Y., Lerner, I., Cairney, J. et al. Independent and Joint Associations of Physical Activity and Sleep on Mental Health Among a Global Sample of 200,743 Adults. Int.J. Behav. Med. (2024). https://doi.org/10.1007/s12529-024-10280-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s12529-024-10280-8