Abstract
Background
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is responsible for an important mortality rate worldwide. We aimed to evaluate the actual imputability of SARS-CoV-2 on the mortality rate associated with SARS-CoV-2-related illnesses in the pediatric intensive care unit (PICU). Secondary objectives were to identify risk factors for death.
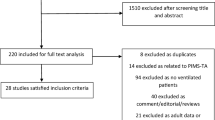
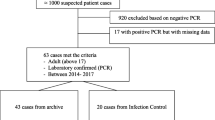
Methods
This national multicenter comparative study comprised all patients under 18 years old with positive SARS-CoV-2 polymerase chain reactions (PCRs) [acute corona virus disease 2019 (COVID-19) or incidental SARS-CoV-2 infection] and/or pediatric inflammatory multisystem syndrome (PIMS) recorded in the French PICU registry (PICURe) between September 1, 2021, and August 31, 2022. Included patients were classified and compared according to their living status at the end of their PICU stay. Deceased patients were evaluated by four experts in the field of pediatric infectiology and/or pediatric intensive care. The imputability of SARS-CoV-2 as the cause of death was classified into four categories: certain, very probable, possible, or unlikely, and was defined by any of the first three categories.
Results
There were 948 patients included of which 43 died (4.5%). From this, 26 deaths (67%) could be attributed to SARS-CoV-2 infection, with an overall mortality rate of 2.8%. The imputability of death to SARS-CoV-2 was considered certain in only one case (0.1%). Deceased patients suffered more often from comorbidities, especially heart disease, neurological disorders, hematological disease, cancer, and obesity. None of the deceased patients were admitted for pediatric inflammatory multisystem syndrome (PIMS). Mortality risk factors were male gender, cardiac comorbidities, cancer, and acute respiratory distress syndrome.
Conclusions
SARS-CoV-2 mortality in the French pediatric population was low. Even though the imputability of SARS-CoV-2 on mortality was considered in almost two-thirds of cases, this imputability was considered certain in only one case.
Graphical Abstract


Similar content being viewed by others
Data availability
All data that support the findings of this study will be available from the corresponding author upon reasonable request.
References
Salzberger B, Buder F, Lampl B, Ehrenstein B, Hitzenbichler F, Holzmann T, et al. Epidemiology of SARS-CoV-2. Infection. 2021;49:233–9.
COVID-19 Excess Mortality Collaborators. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet. 2022;399:1513–6.
Marwali EM, Kekalih A, Yuliarto S, Wati DK, Rayhan M, Valerie IC, et al. Paediatric COVID-19 mortality: a database analysis of the impact of health resource disparity. BMJ Paediatr Open. 2022;6:e001657.
Nachega JB, Sam-Agudu NA, Budhram S, Taha TE, Vannevel V, Somapillay P, et al. Effect of SARS-CoV-2 Infection in pregnancy on maternal and neonatal outcomes in Africa: an AFREhealth call for evidence through multicountry research collaboration. Am J Trop Med Hyg. 2020;104:461–5.
Liguoro I, Pilotto C, Bonanni M, Ferrari ME, Pusiol A, Nocerino A, et al. SARS-COV-2 infection in children and newborns: a systematic review. Eur J Pediatr. 2020;179:1029–46.
Tsankov BK, Allaire JM, Irvine MA, Lopez AA, Sauvé LJ, Vallance BA, et al. Severe COVID-19 infection and pediatric comorbidities: a systematic review and meta-analysis. Int J Infect Dis. 2021;103:246–56.
Harman K, Verma A, Cook J, Radia T, Zuckerman M, Deep A, et al. Ethnicity and COVID-19 in children with comorbidities. The Lancet Child Adolesc Health. 2020;4:e24–5.
Bixler D, Miller AD, Mattison CP, Taylor B, Komatsu K, Peterson Pompa X, et al. SARS-CoV-2–associated deaths among persons aged 21 years—United States. MMWR Morb Mortal Wkly Rep. 2020;69:1324–9.
Alsohime F, Temsah MH, Al-Nemri AM, Somily AM, Al-Subaie S. COVID-19 infection prevalence in pediatric population: etiology, clinical presentation, and outcome. J Infect Public Health. 2020;13:1791–6.
World Health Organization. Multisystem inflammatory syndrome in children and adolescents with COVID-19. https://www.who.int/publications-detail-redirect/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19. Accessed 20 June 2023.
Recher M, Leteurtre S, Javouhey E, Morin L, Baudin F, Rambaud J, et al. Risk of admission to the pediatric intensive care unit for SARS-CoV-2 delta and omicron infections. J Pediatric Infect Dis Soc. 2023;12:189–97.
Burns KE, Duffett M, Kho ME, Meade MO, Adhikari NK, Sinuff T, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179:245–52.
Lecoeur C, Thibon P, Prime L, Mercier PY, Balouet P, Durin L, et al. Frequency, causes and avoidability of outborn births in a French regional perinatal network. Eur J Obstet Gynecol Reprod Biol. 2014;179:22–6.
Martinet Y. Expertise médicale en pneumologie; question de l’imputabilité du décès. Rev Mal Respir. 2011;28:594–601 (in French).
Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021;21:855.
Manti S, Licari A, Montagna L, Votto M, Leonardi S, Brambilla I, et al. SARS-CoV-2 infection in pediatric population. Acta Biomed. 2020;91(Suppl 11): e2020003.
CDC COVID-19 Response Team. Coronavirus Disease. in Children — United States, February 12–April 2, 2020. MMWR Morb Mortal Wkly Rep. 2019;2020(69):422–6.
Zimmermann P, Curtis N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. 2020;39:355–68.
European Centre for Disease Prevention and Control. COVID-19. https://www.ecdc.europa.eu/en/covid-19. Accessed July 5, 2023.
Mehta NS, Mytton OT, Mullins EWS, Fowler TA, Falconer CL, Murphy OB, et al. SARS-CoV-2 (COVID-19): What do we know about children? a systematic review. Clin Infect Dis. 2020;71:2469–79.
Rodriguez Velásquez S, Jacques L, Dalal J, Sestito P, Habibi Z, Venkatasubramanian A, et al. The toll of COVID-19 on African children: a descriptive analysis on COVID-19-related morbidity and mortality among the pediatric population in Sub-Saharan Africa. Int J Infect Dis. 2021;110:457–65.
van der Zalm MM, Dona’ D, Rabie H. Pediatric coronavirus disease 2019 in Africa. Curr Opin Pediatr. 2023;35:176–83.
Nachega JB, Sam-Agudu NA, Machekano RN, Rabie H, van der Zalm MM, Redfern A, et al. African Forum for Research and Education in Health (AFREhealth) COVID-19 Research Collaboration on Children and Adolescents. Assessment of clinical outcomes among children and adolescents hospitalized with COVID-19 in 6 sub-Saharan African countries. JAMA Pediatr. 2022;176:e216436.
Mosalli RM, Kobeisy SAN, Al-Dajani NM, Ateeg MA, Ahmed MA, Meer WM, et al. Coronavirus disease in children: a single-center study from western Saudi Arabia. Int J Pediatr. 2021;2021:9918056.
Alshengeti A, Alahmadi H, Barnawi A, Alfuraydi N, Alawfi A, Al-Ahmadi A, et al. Epidemiology, clinical features, and outcomes of coronavirus disease among children in Al-Madinah, Saudi Arabia: a retrospective study. Int J Pediatr Adolesc Med. 2022;9:136–42.
Kitano T, Kitano M, Krueger C, Jamal H, Al Rawahi H, Lee-Krueger R, et al. The differential impact of pediatric COVID-19 between high-income countries and low- and middle-income countries: a systematic review of fatality and ICU admission in children worldwide. PLoS One. 2021;16:e0246326.
Heneghan JA, Rogerson C, Goodman DM, Hall M, Kohne JG, Kane JM. Epidemiology of pediatric critical care admissions in 43 united states children’s hospitals, 2014–2019. Pediatr Crit Care Med. 2022;23:484–92.
PICANet – Paediatric Intensive Care Audit Network for the UK and Ireland. Annual Report 2021. https://www.picanet.org.uk/wp-content/uploads/sites/25/2022/04/PICANet-2021-Annual-Report_v1.1-22Apr2022.pdf. Accessed 3 May 2023.
COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47:60–73.
Shapira G, de Walque D, Friedman J. How many infants may have died in low-income and middle-income countries in 2020 due to the economic contraction accompanying the COVID-19 pandemic? Mortality projections based on forecasted declines in economic growth. BMJ Open. 2021;11:e050551.
Coker M, Folayan MO, Michelow IC, Oladokun RE, Torbunde N, Sam-Agudu NA. Things must not fall apart: the ripple effects of the COVID-19 pandemic on children in sub-Saharan Africa. Pediatr Res. 2021;89:1078–86.
Flood J, Shingleton J, Bennett E, Walker B, Amin-Chowdhury Z, Oligbu G, et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 (PIMS-TS): prospective, national surveillance, United Kingdom and Ireland, 2020. Lancet Reg Health Eur. 2021;3:100075.
Bowen A, Miller AD, Zambrano LD, Wu MJ, Oster ME, Godfred-Cato S, et al. Demographic and clinical factors associated with death among persons <21 years old with multisystem inflammatory syndrome in children—United States, February 2020–March 2021. Open Forum Infect Dis. 2021;8:ofab388.
Abdel-Mannan O, Sutcliffe AG. A national surveillance study of childhood epilepsy mortality in the UK and Ireland. Eur J Neurol. 2020;27:327–33.
Swann OV, Holden KA, Turtle L, Pollock L, Fairfield CJ, Drake TM, et al. Clinical characteristics of children and young people admitted to hospital with covid-19 in United Kingdom: prospective multicentre observational cohort study. BMJ. 2020;370:m3249.
Acknowledgements
We are grateful to Groupe Francophone de Réanimation et d’Urgences Pédiatriques, Santé Publique France. PICURe-GFRUP study group*: Mickael Afanetti, MD, (Nice), Julien Baleine, MD, (Montpellier), Sebastien Barthelemy, MD, (Nice), Jean Bergounioux, MD, PhD, (Garches), Renaud Blondé, MD, (Mamoudzou), Benoit Bœuf, MD, (Clermont-Ferrand), Noel Boussard, MD, (Nancy), Gerald Boussicault, MD, (Angers), Roselyne Brat, MD, (Orléans), Olivier Brissaud, MD, PhD, (Bordeaux), Julie Chantreuil, MD, (Tours), Camille Chavy, MD, (Dijon), Emmanuel Couadau, MD, (Nouméa), Thibaud Dabudyk, MD, (Besançon), Etienne Darrieux, MD, (Saint Pierre), Stéphane Dauger, MD, PhD (Paris Robert-Debré), Jean-Marie De Guillebon De Resnes, MD, (Nice), Émeline Gabilly-Benard, MD, (Poitiers), Sophie Galene Gromez, MD, (Rouen), Armelle Garenne, MD, (Brest), Ghida Ghostine, MD, (Amiens), Charlene Grabot, MD, (Fort de France), Anne-Sophie Guilbert, MD, (Strasbourg), Aurélie Hayotte, MD, (Paris Robert-Debré), Silvia Lacobelli, MD, (Saint-Pierre), Mikaël Jokic, MD, (Caen), Nicolas Joram, MD, (Nantes), Aurelie Labarre, MD, (Rouen), Marie Lampin, MD, (Lille), Pierre-Louis Leger, MD, PhD, (Paris Trousseau), Marc Lilot, MD, (Lyon), Gauthier Loron, MD, (Reims), Emilien Maisonneuve, MD, (Grenoble), Arielle Maroni, MD, (Paris Robert-Debré), Christophe Milési, MD, PhD, (Montpellier), Fabrice Michel, MD, PhD, (Marseille), Juliette Montmayeur, MD, (Paris Necker-Enfants-Malades), Jérôme Naudin, MD, (Paris Robert-Debré), Paul Nolent, MD, (Bordeaux), Karine Norbert, MD, (Pau), Gilles Orliaguet, MD, PhD, (Paris Necker-Enfants-Malades), Mehdi Oualha, MD, PhD, (Paris Necker-Enfants-Malades), Bruno Ozanne, MD, (Rennes), Hugues Patural, MD, PhD, (Saint-Etienne), Sonia Pelluau, MD, (Toulouse), Jérôme Pignol, MD, (Fort de France), Laure Ponthier, MD, (Limoges), Amandine Prenant, MD, (Angers), Sylvain Renolleau, MD, PhD, (Paris Necker-Enfants-Malades), Lila Robin, MD, (Orléans), Charlotte Roulland, MD, (Caen), Nicolas Roullet-Renoleau, MD, (Tours), Emilie Ruiz, MD, (Poitiers), Iona Sicard-Cras, MD, (Brest), Gerard Thiriez, MD, PhD, (Besançon), Fabrice Ughetto MD, (Marseille), Florence Villedieu, MD, (Caen), Arnaud Wiedemann, MD, PhD, (Nancy), Lorenco Xavier, MD, (Nouméa), Justine Zini, MD, (Garches).
Author information
Authors and Affiliations
Contributions
MLB, NV: methodology, validation, investigation, writing–original draft. ML, MR: conceptualization, methodology, writing–review and editing. ARB: formal analysis, writing–review and editing. EJ, SB, JD, MC: Investigation, Writing–Review and Editing. FA: onceptualization, writing–review and editing. SL: conceptualization, methodology, writing–review and editing, supervision. DB: conceptualization, methodology, validation, formal analysis, data curation, writing–review and editing, supervision.
Corresponding author
Ethics declarations
Conflicts of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approval
The Local Research Ethics Committee for health research of the University Hospital of CAEN approved our protocol on May 16, 2022 (ID 3456). This study was part of the official public health activity (Ministry of Solidarity and Health) and was approved as a medical registry assessment without the requirement for patient consent by the French Advisory Committee on Information Processing in Health Research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lockhart-Bouron, M., Vanel, N., Levy, M. et al. Severe acute respiratory syndrome coronavirus-2-related and imputable deaths in children: results from the French pediatric national registry. World J Pediatr (2024). https://doi.org/10.1007/s12519-023-00791-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12519-023-00791-x