Abstract
Background
Coronavirus disease 2019 (COVID-19) has different manifestations in pediatric cases. It is assumed that they might present more gastrointestinal symptoms with a different viral shedding pattern in gastrointestinal samples. In this systematic review and meta-analysis, we aimed to evaluate the viral shedding pattern in gastrointestinal specimens of children with COVID-19.
Methods
We searched all published studies in English language in PubMed, Web of Science, and Scopus, up to date as of October 2021. Our search included the term "severe acute respiratory syndrome coronavirus 2, COVID-19, SARS-CoV-2, novel coronavirus, or coronavirus; and shed, excrete, secret, or carriage; and stool or rectal; and children or pediatrics". We included studies evaluating SARS-CoV-2 shedding in gastrointestinal specimens, including rectal swabs and stool samples of children with COVID-19 infection. We excluded duplicated data, case reports, and studies without original data.
Results
Twelve studies met the eligibility criteria for the qualitative synthesis, 10 of which were included in the meta-analysis. The pooled prevalence of gastrointestinal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA in children with COVID-19 was 86% (95% confidence interval 73%–96%, I2 = 62.28%). After respiratory specimen had become negative, 72% (43/60) had persistent shedding in gastrointestinal specimens. The gastrointestinal RNA had a positive test result for more than 70 days after symptoms onset.
Conclusions
Gastrointestinal shedding of SARS-CoV-2 might occur in a substantial portion of children and might persist long after negative respiratory testing. Further research is recommended to find the role of SARS-CoV-2 gastrointestinal shedding in transmission in children.
Similar content being viewed by others
Introduction
The outbreak of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) led to coronavirus disease 2019 (COVID-19). The disease spread quickly to the world and led to a major crisis, the COVID-19 pandemic [1, 2]. The most common clinical presentation of patients with COVID-19 are fever and respiratory symptoms; however, an increasing number of studies report that a variety of gastrointestinal (GI) symptoms such as diarrhea, vomiting, abdominal pain, as well as some atypical findings can also be found in adults and also pediatric patients [3,4,5,6]. COVID-19 mostly occurs in adults and children only represent 1%–8% of the total laboratory-confirmed cases [7]. SARS-CoV-2 is primarily transmitted through respiratory droplets and person-to-person close contact [8]. Based on this transmission route, COVID-19 infection is diagnosed by the presence of SARS-CoV-2 RNA in upper and lower respiratory specimens by real-time reverse transcription polymerase chain reaction (RT-PCR). However, viral RNA can be found in other samples [9]. SARS-CoV-2 RNA can also be detected in anal/rectal swabs and stool specimens from COVID-19 patients, due to the pathogenicity of the virus in the GI tract, raising concerns about the fecal–oral route of transmission. Interestingly, viral shedding through feces could continue even after respiratory tests are, or have become, negative [10,11,12].
A few studies have reviewed the possibility of the fecal–oral transmission in patients with COVID-19 [13,14,15,16], and a comprehensive result of fecal viral shedding in children is still lacking. On the other hand, children show different clinical characteristics, less severe infection, and different viral load and shedding pattern compared to the adults [17,18,19,20]. Therefore, this study aims to assess viral shedding through GI samples in children infected with COVID-19 and provide an overview of the available literature regarding the fecal–oral transmission of the SARS-CoV-2.
Methods
Search strategies
This study was performed according to the PRISMA guidelines (preferred reporting items for systematic reviews and meta-analysis) [21]. We searched electronic databases, including PubMed, Scopus, and Web of Science, up to date as of October 2021. Search studies were limited to those written in English. Our search included the terms: severe acute respiratory syndrome coronavirus 2, COVID-19, SARS-CoV-2, novel coronavirus, or coronavirus; and shed, excrete, secret, or carriage; and stool or rectal; and children or pediatrics. References cited by the identified studies were also screened for additional references.
Study selection
We included studies that met the following criteria: (1) laboratory-confirmed children (defined as being < 18 years) with respiratory COVID-19 infection based on positive RT-PCR results and (2) evaluation of GI specimen including stool collection or rectal swabs for SARS-CoV-2 RNA. We excluded (1) duplicated data; (2) case reports (< 2 patients); and (3) studies without original data (e.g., review articles).
Two reviewers performed the initial screening of titles and abstracts independently to identify potentially relevant studies. The full texts of the selected studies were screened by two independent authors. There was a complete agreement regarding the excluded studies. Two authors independently performed data extraction from each study included. If necessary, we tried to contact the author of the original study by e-mail. Disagreements and uncertainties were resolved by consensus. EndNote (version X8) was used to manage the articles and citations. Information including the first author, study period, country of origin, age, infection status (symptomatic infection or asymptomatic infection), symptoms, number of confirmed patients with COVID-19, number of patients with positive SARS-CoV-2 RNA in GI samples before and after the loss of respiratory RNA, and maximum duration of positive GI samples from symptoms onset or hospitalization were extracted.
Quality assessment
The scale known as quality assessment of diagnostic accuracy studies (QUADAS) was used to assess the quality of the included studies [22]. The scale consists of 14 items, and 1 point is given to each item if the conditions are met.
Statistical analysis
We calculated a weighted pooled estimate of the proportion testing positive from the GI samples using random-effects modeling, which in case of heterogeneity provides more conservative estimates than fixed effects modeling. Heterogeneity was assessed visually using a forest plot, which represents the estimated prevalence and their relevant 95% confidence interval (CI). The heterogeneity of studies was examined using Cochran’s heterogeneity statistic (Q test) and summarized as I2. The I2 values of 25%, 50% and 75% were considered as low, medium, and high heterogeneity, respectively. Publication bias was assessed with funnel plots and Egger’s regression test [23]. All the analyses were undertaken using STATA software (Release 12. statistical software. College Station, Texas: STATA Corp LP).
Results
Search strategies
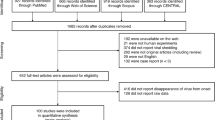
The search strategies resulted in 169 studies, which were reduced to 156 citations after removing the duplicates. The titles and abstracts of these records were screened, and then 142 studies were excluded, and 14 records were selected for full-text review. After a full-text review, two studies that did not have the required information, the number of positive results for SARS-CoV-2 RNA in GI specimens of children, were excluded [24, 25]. Finally, 12 studies met the eligibility criteria and were included in the qualitative synthesis. Two studies did not have the required information to be included in the meta-analysis [17, 18]. Figure 1 shows the study selection process based on the PRISMA guidelines.
Study characteristics
Most studies were performed in China (83%, 10/12), except for two studies that were conducted in Germany and Italy (Table 1). Of the included studies, all had case report/case series designs. All studies were conducted between January and April 2020. In total, 171 children were included in this study for qualitative analysis. All children had respiratory COVID-19 infection and were tested for SARS-CoV-2 RNA in GI specimens. The age of the patients ranged from 8 days to 210 months.
None of the children had severe disease. Of 171 patients, 38 (22%) were asymptomatic, and 41 had no information on symptoms available. The main symptoms were fever (52%, 64/124) and cough (33%, 41/124), and GI manifestations including vomiting, diarrhea, abdominal pain, and constipation were reported totally in 12% (15/124) of children. Nine (75%) studies tested SARS-CoV-2 presence in stool samples, 1 (8%) in rectal swabs, and 2 (17%) in rectal swabs or stool samples. All studies performed real-time RT-PCR to detect SARS-CoV-2 in GI specimens. Further details on study characteristics, along with the QUADAS score, are depicted in Table 1.
Prevalence of fecal SARS-CoV-2 RNA
The pooled prevalence of fecal SARS-CoV-2 RNA in patients with COVID-19 confirmed by respiratory samples was 86% (95% CI 73%–96%) (Fig. 2). The highest prevalence was 100% in three studies, and the lowest was 33% (3/10) in a study by Tan et al. [28]. Eight studies had available data to compare fecal SARS-CoV-2 positivity rate in symptomatic and asymptomatic patients. From symptomatic and asymptomatic children, 90% (45/50) and 69% (9/13) were positive for fecal RNA, respectively. There was no significant difference in the positivity rate of fecal RNA between symptomatic and asymptomatic patients (P > 0.05).
Persistent shedding of fecal SARS-CoV-2 RNA
All studies had serial SARS-CoV-2 test results for both respiratory and GI specimens, and all reported persistently positive results for SARS-CoV-2 RNA in GI specimens after the virus converted negative in respiratory samples. Nine studies had available data on the prevalence of SARS-CoV-2 RNA in GI samples after respiratory specimen had become negative. From children who had a positive GI specimen test collectively, 72% (43/60) had persistent positive GI specimen test despite negative respiratory test.
SARS-CoV-2 RNA was detected in GI specimens for more than 70 days after onset of illness and more than 5 weeks after hospital admission. In most studies, researchers did not continue follow-up until the point of negative results. One study compared the mean duration of viral shedding in the GI tract between symptomatic and asymptomatic cases, and no significant difference was reported (28.1 ± 13.3 days vs. 30.8 ± 18.6 days, P > 0.05).
Results revealed a medium heterogeneity among the selected studies (I2 = 62.28%; P < 0.01). The funnel plot shows the presence of a possible publication bias. Based on Egger's regression test, the publication bias among included studies could not be ignored (P < 0.001; Fig. 3). The pooled estimates of prevalence might be reduced because of concerns regarding risk of bias (selection bias, detection bias, and attrition bias), and inconsistency of the tested patient populations; which may have contributed to the heterogeneity of findings across studies.
Discussion
We performed a systematic review and meta-analysis to clarify the viral shedding of SARS-CoV-2 through GI specimens in children with positive COVID-19 respiratory tests. In the previous study conducted by Wang et al. [35], GI symptoms and fecal nucleic acid detection in pediatric COVID-19 patients were analyzed. In this study, we performed a meta-analysis to find the prevalence of SARS-CoV-2 RNA in GI specimens. Our research did not identify any studies on children with severe disease. Based on the reports published, most infected children showed mild disease [36], however, approximately 4.4% of infected children have severe disease with a mortality rate of 0.2% [37]. In a study by Mamishi et al. [38], 71% (n = 24) of pediatric cases showed severe SARS-CoV-2 infection, and the mortality of 12.5% (n = 3) was reported. Based on our results regarding the main clinical manifestations, of 124 cases with available data on symptoms, fever was reported in 64 (52%), cough in 41 (33%), and GI symptoms including vomiting, diarrhea, abdominal pain, and constipation in 15 (12%).
In our study, the pooled prevalence of fecal SARS-CoV-2 RNA through GI specimens was 86% in children. Similarly, in systematic reviews by Xu et al. [39] (n = 42) and Wang et al. [35] (n = 106), the nucleic acid positivity rates of feces in children were 89% and 85.7%, respectively. However, based on the study by Cheung et al. [40] on adult patients (n = 4243), the pooled prevalence of fecal RNA was lower (54%). The lower prevalence might be due to the fact that children might present more often GI symptoms compared to adults, and a higher proportion of fecal SARS-CoV-2 RNA is observed in patients with GI manifestation [16, 41].
All included studies reported persistent detectable RNA in GI specimens after the loss of RNA in the respiratory tract. The positivity rate of fecal RNA after the respiratory tract specimens turned negative was 72% (43/60). In the systematic review by Wang et al. [35], 71.2% (52/73) had persistent positive fecal RNA despite negative respiratory tests. Small studies involving both adults and pediatric cases reported a higher incidence of positive fecal RNA after negative respiratory swab in children compared to adults [18]. However, in the systematic review by Cheung et al. [40], 70.3% (87/124) of adult patients with detectable RNA in stool samples remained positive after the loss of virus from respiratory specimens, which is near to studies on children.
SARS-CoV-2 RNA can be detected through GI specimens of children for more than 70 days. This prolonged shedding observed in pediatric cases also occurs in adults but to a less extent [41]. However, the duration of viral shedding might mainly be due to the host immune status leading to longer viral shedding [14, 42]. According to a previous report, a high level of IL-10 and reduced counts of T-cell and B-cell are associated with prolonged viral RNA shedding [42]. In a study by Ma et al. [17], the possible reasons behind this phenomenon are discussed and considered to be less hand hygiene and different expression of angiotensin converting enzyme 2, a functional receptor for SARS-CoV-2, in the intestine of children. Moreover, high-dose corticosteroids might result in delayed virus clearance and prolonged viral shedding time [14].
The detection of viral RNA in GI specimens does not necessarily indicate that viable infectious virions are present or can transmit through the fecal route [43]. However, some studies demonstrate live viruses through culturing positive SARS-CoV-2 fecal samples [24, 44, 45]. Moreover, since the genetics of SARS-CoV-2 is similar to SARS-CoV that had confirmed fecal–oral transmission, the possibility of a similar transmission route remains to be determined [46]. One limitation of our study is the small number of included studies, with small sample sizes. Studies with higher quality are required to better understand the fecal viral shedding of SARS-CoV-2 in children.
In conclusion, GI shedding of SARS-CoV-2 might occur in a substantial portion of children and also persist long after negative respiratory testing and symptoms resolution. Further research is recommended to find the role of SARS-CoV-2 GI shedding in transmission in children.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20.
Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115:766–73.
Mahmoudi S, Mehdizadeh M, Shervin Badv R, Navaeian A, Pourakbari B, Rostamyan M, et al. The coronavirus disease 2019 (COVID-19) in children: a study in an Iranian Children’s Referral Hospital. Infect Drug Resist. 2020;13:2649–55.
Ekbatani MS, Hassani SA, Tahernia L, Yaghmaei B, Mahmoudi S, Navaeian A, et al. Atypical and novel presentations of coronavirus disease 2019: a case series of three children. Br J Biomed Sci. 2021;78:47–52.
Mamishi S, Movahedi Z, Mohammadi M, Ziaee V, Khodabandeh M, Abdolsalehi MR, et al. Multisystem inflammatory syndrome associated with SARS-CoV-2 infection in 45 children: a first report from Iran. Epidemiol Infect. 2020;148:e196.
Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Carducci FIC, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4:653–61.
World Health Organization. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations: scientific brief, 29 March 2020 (No. WHO/2019-nCoV/Sci_Brief/Transmission_modes/2020.1). 2020.
Pourakbari B, Mahmoudi S, Mahmoudieh Y, Eshaghi H, Navaeian A, Rostamyan M, et al. SARS-CoV-2 RNAaemia in children: an Iranian referral hospital-based study. J Med Virol. 2021;93:5452–7.
Ling Y, Xu SB, Lin YX, Tian D, Zhu ZQ, Dai FH, et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J (Engl). 2020;133:1039–43.
Wu Y, Guo C, Tang L, Hong Z, Zhou J, Dong X, et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol. 2020;5:434–5.
Chen Y, Chen L, Deng Q, Zhang G, Wu K, Ni L, et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol. 2020;92:833–40.
van Doorn AS, Meijer B, Frampton CM, Barclay ML, de Boer NK. Systematic review with meta-analysis: SARS-CoV-2 stool testing and the potential for faecal-oral transmission. Aliment Pharmacol Ther. 2020;52:1276–88.
Yan D, Zhang X, Chen C, Jiang D, Liu X, Zhou Y, et al. Characteristics of viral shedding time in SARS-CoV-2 infections: a systematic review and meta-analysis. Front Public Health. 2021;9:652842.
Parasa S, Desai M, Thoguluva Chandrasekar V, Patel HK, Kennedy KF, Roesch T, et al. Prevalence of gastrointestinal symptoms and fecal viral shedding in patients with coronavirus disease 2019: a systematic review and meta-analysis. JAMA Netw Open. 2020;3:e2011335.
Zhang Y, Cen M, Hu M, Du L, Hu W, Kim JJ, et al. Prevalence and persistent shedding of fecal SARS-CoV-2 RNA in patients with COVID-19 infection: a systematic review and meta-analysis. Clin Transl Gastroenterol. 2021;12:e00343.
Ma X, Su L, Zhang Y, Zhang X, Gai Z, Zhang Z. Do children need a longer time to shed SARS-CoV-2 in stool than adults? J Microbiol Immunol Infect. 2020;53:373–6.
Su L, Ma X, Yu H, Zhang Z, Bian P, Han Y, et al. The different clinical characteristics of corona virus disease cases between children and their families in China–the character of children with COVID-19. Emerg Microbes Infect. 2020;9:707–13.
de Souza TH, Nadal JA, Nogueira RJ, Pereira RM, Brandão MB. Clinical manifestations of children with COVID-19: a systematic review. Pediatr Pulmonol. 2020;55:1892–9.
Xing YH, Ni W, Wu Q, Li WJ, Li GJ, Wang WD, et al. Prolonged viral shedding in feces of pediatric patients with coronavirus disease 2019. J Microbiol Immunol Infect. 2020;53:473–80.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84.
Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Zhang Y, Chen C, Song Y, Zhu S, Wang D, Zhang H, et al. Excretion of SARS-CoV-2 through faecal specimens. Emerg Microbes Infect. 2020;9:2501–8.
Kipkorir V, Cheruiyot I, Ngure B, Misiani M, Munguti J. Prolonged SARS-CoV-2 RNA detection in anal/rectal swabs and stool specimens in COVID-19 patients after negative conversion in nasopharyngeal RT-PCR test. J Med Virol. 2020;92:2328–31.
Cai J, Wang X, Zhao J, Ge Y, Xu J, Tian H, et al. Comparison of clinical and epidemiological characteristics of asymptomatic and symptomatic SARS-CoV-2 infection in children. Virol Sin. 2020;35:803–10.
Hua CZ, Miao ZP, Zheng JS, Huang Q, Sun QF, Lu HP, et al. Epidemiological features and viral shedding in children with SARS-CoV-2 infection. J Med Virol. 2020;92:2804–12.
Tan YP, Tan BY, Pan J, Wu J, Zeng SZ, Wei HY. Epidemiologic and clinical characteristics of 10 children with coronavirus disease 2019 in Changsha. China. J Clin Virol. 2020;127:104353.
Xu Y, Li X, Zhu B, Liang H, Fang C, Gong Y, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26:502–5.
Liu P, Cai J, Jia R, Xia S, Wang X, Cao L, et al. Dynamic surveillance of SARS-CoV-2 shedding and neutralizing antibody in children with COVID-19. Emerg Microbes Infect. 2020;9:1254–8.
Ma X, Su L, Cheng L, Zhang Z, Sun J, Liu M, et al. Severe acute respiratory syndrome coronavirus 2 viral load in respiratory and feces specimens of children with coronavirus disease 2019. Future Virol. 2021;16:85–91.
Wolf GK, Glueck T, Huebner J, Muenchhoff M, Hoffmann D, French LE, et al. Clinical and epidemiological features of a family cluster of symptomatic and asymptomatic severe acute respiratory syndrome coronavirus 2 infection. J Pediatric Infect Dis Soc. 2020;9:362–5.
Cai J, Xu J, Lin D, Yang Z, Xu L, Qu Z, et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis. 2020;71:1547–51.
De Ioris MA, Scarselli A, Ciofi degli Atti ML, Ravà L, Smarrazzo A, Concato C, et al. Dynamic viral severe acute respiratory syndrome coronavirus 2 RNA shedding in children: preliminary data and clinical consideration of Italian regional center. J Pediatric Infect Dis Soc. 2020;9:366–9.
Wang JG, Cui HR, Tang HB, Deng XL. Gastrointestinal symptoms and fecal nucleic acid testing of children with 2019 coronavirus disease: a systematic review and meta-analysis. Sci Rep. 2020;10:17846.
Sancho-Shimizu V, Brodin P, Cobat A, Biggs CM, Toubiana J, Lucas CL, et al. SARS-CoV-2–related MIS-C: a key to the viral and genetic causes of Kawasaki disease? J Exp Med. 2021;218:e20210446.
Zare-Zardini H, Soltaninejad H, Ferdosian F, Hamidieh AA, Memarpoor-Yazdi M. Coronavirus disease 2019 (COVID-19) in children: prevalence, diagnosis, clinical symptoms, and treatment. Int J Gen Med. 2020;13:477–82.
Mamishi S, Heydari H, Aziz-Ahari A, Shokrollahi MR, Pourakbari B, Mahmoudi S, et al. Novel coronavirus disease 2019 (COVID-19) outbreak in children in Iran: atypical CT manifestations and mortality risk of severe COVID-19 infection. J Microbiol Immunol Infect. 2021;54:839–44.
Xu CL, Raval M, Schnall JA, Kwong JC, Holmes NE. Duration of respiratory and gastrointestinal viral shedding in children with SARS-CoV-2: a systematic review and synthesis of data. Pediatr Infect Dis J. 2020;39:e249–56.
Cheung KS, Hung IFN, Chan PPY, Lung KC, Tso E, Liu R, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis. Gastroenterology. 2020;159:81–95.
Al-Beltagi M, Saeed NK, Bediwy AS, El-Sawaf Y. Paediatric gastrointestinal disorders in SARS-CoV-2 infection: epidemiological and clinical implications. World J Gastroenterol. 2021;27:1716–27.
Hao S, Lian J, Lu Y, Jia H, Hu J, Yu G, et al. Decreased B cells on admission associated with prolonged viral RNA shedding from the respiratory tract in coronavirus disease 2019: a case–control study. J Infect Dis. 2020;222:367–71.
Atkinson B, Petersen E. SARS-CoV-2 shedding and infectivity. Lancet. 2020;395:1339–40.
Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843–4.
Xiao F, Sun J, Xu Y, Li F, Huang X, Li H, et al. Infectious SARS-CoV-2 in feces of patient with severe COVID-19. Emerg Infect Dis. 2020;26:1920.
Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020;5:335–7.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MM involved in designing and interpretations the manuscript. BS involved in gathering and grouping the articles and writing the draft of the manuscript. MS involved in statistical analysis and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Benvari, S., Mahmoudi, S. & Mohammadi, M. Gastrointestinal viral shedding in children with SARS-CoV-2: a systematic review and meta-analysis. World J Pediatr 18, 582–588 (2022). https://doi.org/10.1007/s12519-022-00553-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00553-1