Abstract
Introduction
In a phase III clinical trial (NCT02730299), omidubicel-onlv, a nicotinamide-modified allogeneic hematopoietic progenitor cell therapy, showed rapid hematopoietic and immune recovery compared with standard umbilical cord blood (UCB) transplant across all racial/ethnic groups.
Methods
A decision-tree model was used to project the effect of omidubicel-onlv availability on addressing health disparities in allogeneic hematopoietic cell transplantation (allo-HCT) access and outcomes for patients with hematologic malignancies. The model used a hypothetical population of 10,000 allo-HCT-eligible US adults, for whom matched related donors were not available. Patients received matched or mismatched unrelated donor, haploidentical, UCB transplant, or no transplant. Scenarios with omidubicel-onlv use of 0% (status quo), 10%, 15%, 20%, and 30% were modeled on the basis of proportional reductions in other allo-HCT sources or no transplant by racial/ethnic group.
Results
Increased omidubicel-onlv use was associated with a higher proportion of patients undergoing allo-HCT, decreased time to allo-HCT, decreased 1-year non-relapse mortality, and increased 1-year overall survival, particularly among racial minorities. In the scenario modeling 20% omidubicel-onlv use, the proportion of Black patients receiving allo-HCT increased by 129%; increases were also observed in Asian (64%), Hispanic (45%), and other (42%) patient groups. Modeled time to allo-HCT improved among transplanted patients (23%) from 11.4 weeks to 8.8 weeks. One-year OS in the overall population increased by 3%, with improvements ranging from 3% for White patients to 5% for Black patients.
Conclusion
This study demonstrates that broad access to omidubicel-onlv could increase access to allo-HCT and improve outcomes for patients, with the greatest benefits seen among racial/ethnic minority groups.
Graphical Abstract

Similar content being viewed by others
Why carry out this study? |
Many patients who are otherwise eligible for allogeneic hematopoietic cell transplantation (allo-HCT) lack an appropriate donor, and it can be challenging for some patients, including patients from racial and ethnic minorities, to find appropriate donors in registries. |
A phase 3 study of omidubicel-onlv, a nicotinamide-modified allogeneic hematopoietic progenitor cell therapy donor source, showed clinical benefits, including rapid hematopoietic and immune recovery and decreased rate of infections, compared with standard umbilical cord blood transplant for patients across all race/ethnic groups. |
A decision-tree model was used to project the effect of availability of omidubicel-onlv as a new donor source on addressing health equity disparities in allo-HCT access. |
What was learned from the study? |
Increased omidubicel-onlv use improved access to allo-HCT and improvements in clinical outcomes with the highest benefits seen among racial/ethnic minorities. |
Digital Features
This article is published with digital features, including a graphical abstract, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.24805905.
Introduction
Allogeneic hematopoietic cell transplantation (allo-HCT) is a widely accepted curative therapy for both malignant and nonmalignant diseases [1]. The majority of patients who are eligible for allo-HCT lack a human leukocyte antigen (HLA)-matched related donor (MRD) and rely on haploidentical (HI) related donors and donor registries to identify mismatched or matched unrelated donors (MMUD, MUD) and umbilical cord blood (UCB) units [2,3,4]. Finding a suitable donor is often a lengthy process and is especially challenging for racial and ethnic minorities underrepresented in donor registries [4,5,6].
Several studies have described the disparities in donor availability. In an analysis of data from the National Marrow Donor Program registry (NMDP), the likelihood of finding an 8/8 HLA-matched adult donor was 75% for White patients of European descent compared with 16–52% for other racial and ethnic groups (including Black, Hispanic, Asian/Pacific Islander, Native American patients); similarly, the likelihood of finding a 6/6 HLA-matched UCB unit was approximately 17% for White adult patients and ranged from 1% to 10% for other patients [4]. In a study of 601 consecutive adults with hematologic malignancies (HM) over a 6-year period at Memorial Sloan-Kettering Cancer Center, Europeans were more likely to receive an optimal donor graft compared with non-Europeans (84% vs 67%), with the lowest proportions observed for White Hispanics and African patients [6]. A prospective analysis evaluating unrelated UCB and HI donor availability observed that access to a suitable graft was highest for European patients (95% and 84%, respectively) compared with African patients (65% and 44%, respectively) or non-African, non-European patients (87% and 82%, respectively) [7]. Additionally, racial and ethnic disparities have been observed in transplant-related outcomes [8] including survival [9, 10], treatment failure [11], overall mortality [11, 12], and severe graft versus host disease [13].
For racial and ethnic minority patients, UCB is a promising stem cell graft option owing to its rapid availability and less strict HLA matching criteria [14]. Omidubicel-onlv is a nicotinamide (NAM)-modified allogeneic hematopoietic progenitor cell therapy derived from a single banked UCB unit [15,16,17,18]. In a phase III, randomized trial comparing omidubicel-onlv to UCB, patients aged 12–65 years with high-risk HM and an available UCB unit HLA-matched at four or more loci were enrolled [15]. The median age of patients was 41 years, with most patients younger than 60 years old. AML (48%) and ALL (33%) accounted for the majority of the diagnosis in the patients; patients with marked or 3+ bone marrow fibrosis or chronic lymphocytic leukemia were excluded. The results demonstrated that patients receiving omidubicel-onlv vs UCB had significantly faster neutrophil engraftment (median 12 days vs 22 days; P < 0.001), faster platelet engraftment (55% vs 35% recovery by 42 days), lower infection rates (37% vs 57%), and shorter hospitalization time in the first 100 days (median 48 days vs 61 days). The trial included a notable proportion of non-White patients (16% Black, 14% Asian, 13% Hispanic or Latino, and 3% multiracial), which, despite the small number of patients, was more diverse compared with US patients receiving their first allo-HCT between 2009 and 2020 in a real-world study from the Center for International Blood & Marrow Transplant Research (CIBMTR) [19]; importantly, the clinical benefits in the overall population were consistent across all race and ethnicity groups studied. Omidubicel-onlv was associated with a trend toward improved progression-free survival and overall survival, although the study was not powered to detect a statistically significant difference in these endpoints. On the basis of these data, in April 2023, the US Food and Drug Administration approved omidubicel-onlv for use in adult and pediatric patients (12 years and older) with hematologic malignancies who are planned for UCB transplantation following myeloablative conditioning to reduce the time to neutrophil recovery and the incidence of infection [20].
Building on the encouraging results from the phase III study, the current analysis reports the results of a decision-tree model that was developed to investigate the projected impact of omidubicel-onlv access on racial and ethnic disparities in allo-HCT patient care. We hypothesize that broadening access to omidubicel-onlv can help reduce current racial disparities in allo-HCT access and improve transplant-related outcomes for populations underrepresented in donor registries.
This analysis is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Methods
Model Overview
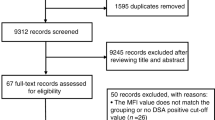
We developed a decision-tree model in Microsoft Excel® to evaluate allo-HCT access and clinical outcomes in a hypothetical population of 10,000 adult allo-HCT-eligible patients with HM who lack MRD in the USA. Across a 1-year period, modeled patients used the following transplant options: MUD, MMUD, HI bone marrow transplant (BMT)/peripheral blood stem cell transplant (PBSCT), UCB transplant, no transplant, or omidubicel-onlv. The model considered scenarios with omidubicel-onlv use of 0% (status quo), 10%, 15%, 20%, and 30%. In scenarios with omidubicel-onlv use, uptake was based on proportional reductions in other allo-HCT sources or no transplant. Model inputs are described in Tables S1–S3 in the Supplementary Material. CIBMTR 2019 data [21] and US Health and Human Services 2022 data [22] informed the modeled status quo proportion of patients using each transplant option and the racial distribution of patients within each transplant type. Assumptions or other clinical literature were used where data were not readily available (Tables S2–S3 in the Supplementary Material). Thus, the model is expected to reflect recent national transplant use and demographics of allo-HCT use in US adults with HM for whom MRDs were not available. Model outcomes included time to allo-HCT (defined as average time from transplant type decision to procedure), 1-year non-relapse mortality (NRM), the proportion of patients receiving a transplant, and 1-year overall survival (OS). The patient outcomes were modeled for the overall cohort and stratified by racial and ethnic groups to investigate the projected impact of different levels of omidubicel-onlv access on racial and ethnic disparities in allo-HCT patient care.
This analysis is based on data from previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Model Inputs
Proportion of Patients Receiving Each Transplant Type
Data on transplant type distribution were sourced from the CIBMTR [21] (Table S1 in the Supplementary Material). The most recent data available (2019) at the time of model development were used. The number of patients who did not receive allo-HCT was calculated as the number of patients for whom allo-HCT was indicated (as reported by the US Department of Health and Human Services [22]) minus the number of patients who actually received allo-HCT (as reported by CIBMTR) (Table S2 in the Supplementary Material) [21].
Proportion of Patients Receiving Each Transplant Type by Race/Ethnicity
Data on the racial/ethnic distribution of patients who received MUD/MMUD and UCB transplant were sourced from CIBMTR (Table S1 in the Supplementary Material) [21]. Data were not available for the racial/ethnic distribution of patients who received HI transplant, so an assumption was made that the distribution was the same as that of MUD/MMUD patients. The racial/ethnic distribution of patients who do not receive transplants was not readily available in the literature. Therefore, the modeled racial/ethnic distribution input used for the no transplant group was calculated on the basis of assumptions and demographic data reported about transplanted patients by Gragert et al. [4] and CIBMTR [21]. Gragert et al. [4] reported the probability of finding at least a 4/6 HLA-matched and suitable UCB unit for different racial and ethnic groups. We used this information to calculate the likelihood of transplant by race/ethnic group. We then applied these likelihoods to data on UCB-transplanted patients as reported in CIBMTR and backed out the proportion of patients who did not receive transplant by race/ethnic group (Table S2 in the Supplementary Material) [4, 21]. For omidubicel-onlv, racial/ethnic distribution was based on the distributions of the other modeled options. It was assumed that, with omidubicel-onlv on the market, there would be proportional reductions in use of other modeled allo-HCT types and of the no transplant group among racial groups (e.g., if there was 10% omidubicel-onlv use, every other transplant option would contribute 10% of its patients proportionately from each racial/ethnic group).
Clinical Outcomes
Clinical outcome model inputs, including time to transplant, 1-year OS, and 1-year NRM, by transplant type are summarized in Table S3 in the Supplementary Material. Omidubicel-onlv and UCB inputs were sourced from the phase III multicenter, randomized clinical trial (NCT02730299) comparing omidubicel-onlv with UCB transplant [15]. Time to transplant for omidubicel-onlv was based on assumptions about the anticipated time it would take for patients to receive omidubicel-onlv outside of a clinical trial setting.
For inputs for the other modeled transplant types, a targeted literature review was performed to identify relevant publications. Priority was given to CIBMTR as a comprehensive source of real-world evidence. In addition, studies that reported a mixed HM population were prioritized. Where data were not available, studies including AML and ALL populations were considered, as these conditions comprised a large portion of the overall population for the omidubicel-onlv trial (48% AML and 33% ALL) and, in general, are the main indications for allo-HCT. Further, studies were prioritized on the basis of study design and sample size and included outcomes with definitions and time points that were similar to the omidubicel-onlv trial. Finally, studies featuring populations with two or more transplant options that were included in the model were used, as it was assumed this population would be similar to our modeled population who could receive any of the modeled options rather than being indicated only for one.
Time to transplant for the HI group was informed by a retrospective study from MD Anderson investigating the outcomes of patients with AML and matched unrelated donors [23]. Time to transplant for the MUD/MMUD group was based on a review examining advancements in the UCB field [24]. The 1-year OS inputs for patients in the MUD/MMUD group were informed by OS outcomes reported by CIBMTR. Specifically, results for 1-year survival among patients with AML or ALL and classified as in first remission or second or subsequent remission were extracted and averaged on the basis of the sample sizes contributing to each group. The 1-year OS inputs for patients in the HI group were extracted from the BMT CTN 0603 (NCT00849147) clinical trial [25]. Survival outcomes for patients receiving no transplant were sourced from a retrospective study examining patients with newly diagnosed AML receiving either CPX-351 or Venetoclax and azacytidine [26] and a multicenter clinical trial examining the role of allo-HCT in patients with ALL [27]. The 1-year OS model inputs were calculated as a weighted average of the results, with weighting based on the proportion of patients with AML and ALL from the omidubicel-onlv phase III clinical trial [15]. The 1-year NRM inputs for patients in the MUD/MMUD and HI groups were extracted from a retrospective study investigating allo-HCT outcomes among HI and MUD recipients with an HM [28].
Model Design
Modeled patients were a hypothetical population of 10,000 allo-HCT-eligible adults in the USA with HM lacking MRD (Fig. 1). Specific HMs were not considered in the model. The model did not perform statistical testing, so the statistical significance of modeled results was not assessed.
Model schema developed to project allo-HCT access and clinical outcomes in a hypothetical population. allo-HCT allogeneic hematopoietic cell transplantation, BMT bone marrow transplant, HI haploidentical, MRD matched related donor, MUD matched unrelated donor, MMUD mismatched unrelated donor, NRM non-relapse mortality, OS overall survival, PBSCT peripheral blood stem cell transplant, UCB umbilical cord blood, US United States
At the model start, patients were assigned a transplant option: MUD/MMUD BMT/PBSCT, HI BMT/PBSCT, UCB transplant, or no transplant. In the status quo setting, no patients were modeled to receive omidubicel-onlv, serving as a reference case for scenarios of omidubicel-onlv access. Within each transplant option, the mutually exclusive racial and ethnic identity, distribution-based CIBMTR classifications were applied: White, Black, Hispanic, Asian, and Other (unknown, other, and multiple races). Scenarios with 10%, 15%, 20%, and 30% omidubicel-onlv uptake were modeled on the basis of reductions in use of other modeled allo-HCT types or no transplant (e.g., 10% from each group), drawing proportionately from racial groups.
Over a 1-year model time horizon, patients experienced clinical outcomes according to the transplant type received. The patient outcomes were modeled as an overall cohort, as well as stratified by the mutually exclusive racial and ethnic identities. For each scenario (status quo; 10%, 15%, 20%, or 30% omidubicel-onlv use), weighted averages of the modeled outcomes across transplant types were calculated for the overall population and by racial/ethnic group. The proportion of patients receiving a transplant and 1-year OS were modeled in the entire patient cohort (including those not receiving a transplant). Time to transplant and 1-year NRM were related to transplant receipt, and so were modeled only among patients receiving a transplant.
Key Model Assumptions
All race/ethnicity groups modeled were based on CIBMTR classification and were considered to be mutually exclusive. Clinical outcomes were assumed to be the same for all patients who received a given modeled transplant option, regardless of race/ethnicity or underlying HM. Time to transplant was the time elapsed between the decision being made about the transplant type used and the transplant procedure, which primarily captured the UCB or donor search time for each respective transplant type. It did not include time spent exploring alternative transplant options. Omidubicel-onlv was assumed to take market share from other transplant options using the same percentage reduction from each option (e.g., 10% of patients from each option). The distribution of patients’ races within a transplant type was assumed not to change between scenarios.
Sensitivity Analysis
In a sensitivity analysis, an alternative input for the racial distribution of HI transplant patients was tested. In the base case (described previously), HI patients followed the same racial distribution as unrelated bone marrow or peripheral blood donors reported by CIBMTR. The sensitivity analysis assumed HI patients followed the same racial distribution as related (matched or unmatched) donor recipients reported by CIBMTR.
Results
Status Quo Scenario Without Omidubicel-onlv
In a modeled population of 10,000 patients for whom MRD were unavailable, 4477 (45%) were estimated to receive allo-HCT using current comparator donor sources (MUD, MMUD, HI, UCB) under the status quo scenario without omidubicel-onlv. A total of 5523 (55%) patients in the status quo population did not receive allo-HCT. Among transplanted patients, 66% of White patients underwent allo-HCT, while only 31% of Hispanic, 24% of Asian, and 13% of Black patients received allo-HCT. Mean times from transplant assignment to transplant procedure and 1-year NRM were 11.4 weeks and 24%, respectively, among transplanted patients. Including those not transplanted, 1-year OS was 62% overall, ranging from 59% in Black patients to 65% in White patients.
Scenario with Omidubicel-onlv Uptake
In a scenario evaluating 20% omidubicel-onlv uptake, the proportion of patients receiving a transplant increased overall by 25% (Fig. 2). Black patients receiving allo-HCT increased by 129%, with increases also noted in Asian (64%), Hispanic (45%), Other (42%), and White patients (10%). Modeled time to allo-HCT improved 23% among transplanted patients, from 11.4 to 8.8 weeks (Fig. 3). Improvements in time to transplant ranged from 40% in Black patients to 18% in White patients. Similarly, NRM decreased 13%, with a 10% reduction among White patients, 25% reduction among Black patients, and 16–19% reductions among Asian, Hispanic, and other racial or ethnic groups (Fig. 4). The 1-year OS increased by 3% in the overall population, with improvements ranging from 3% among White patients to 5% among Black patients (Fig. 5). When modeled rates of omidubicel-onlv were increased, the direction of the outcomes remained the same. For instance, as the proportion of omidubicel-onlv transplants increased from 20% to 30%, the modeled time to allo-HCT improved 11% among transplanted patients, from 8.8 to 7.8 weeks (Fig. 3).
Sensitivity Analysis
The results were largely consistent between the base-case model and the sensitivity analysis. Average time to transplant, the percentage of patients experiencing 1-year NRM, and the percentage of patients achieving 1-year OS remained steady across the model versions. The updated assumption for the racial distribution of HI patients led to more racial minorities receiving transplants in the status quo scenario. This change led to a smaller percentage of improvement in the proportion of patients receiving transplants by race as the uptake of omidubicel-onlv increased. In the scenario evaluating 20% omidubicel-onlv uptake, the number of Black patients receiving allo-HCT increased by 91%, Asian patients receiving allo-HCT increased by 57%, and Hispanic, Other, and White patients receiving allo-HCT increased by 38%, 37%, and 11%, respectively. The 1-year OS increased by 3% among White patients, to 5% among Black patients, and 4% for Asian, Hispanic, and Other patients. Modeled time to allo-HCT improvements ranged from 31% in Black patients (from 8.7 to 6.0 weeks) to 19% in White patients (from 12.3 to 9.9 weeks). NRM decreased by 22% among Black patients, 10% among White patients, and 15–18% among Asian, Hispanic, and Other racial or ethnic groups.
Discussion
While allo-HCT is the only potentially curative option for eligible patients, finding a donor match in registries is particularly difficult for racial and ethnic minority patients [2, 4, 5]. The number of unrelated-donor allo-HCT procedures has increased in the last 10 years [2]; however, racial and ethnic minority patients remain most at risk of not receiving a transplant, experiencing a delayed time to transplant and eventually receiving suboptimal donor grafts [6]. UCB sources can extend access to allo-HCT because of less stringent HLA-match requirements, rapid availability, and flexible transplant schedules [14]. Omidubicel-onlv is the first UCB-derived stem and progenitor cell therapy donor source to receive FDA approval based on phase III data, demonstrating promising efficacy and an acceptable safety profile [15,16,17]; furthermore, hematologic and immune reconstitution were consistent across all race and ethnicity groups studied in the phase III trial [15].
In a modeled population of 10,000 adult patients for whom MRD were not available, our decision-tree model demonstrated that broadening access to omidubicel-onlv was associated with higher proportions of eligible patients undergoing allo-HCT and shorter time to allo-HCT; additionally, increased omidubicel-onlv uptake improved transplant-related outcomes (i.e., decreased 1-year NRM and increased 1-year OS), with greatest benefits noted among racial/ethnic minorities. A sensitivity analysis was performed to evaluate an alternative input for the racial distribution of HI transplant patients. Data were not available on this key input for patients who received HI transplant, so an assumption was made in the base-case model that the distribution was the same as that of MUD/MMUD patients. In the sensitivity analysis, it was assumed that HI patients followed the same racial distribution as unrelated bone marrow or peripheral blood donors. Results from the sensitivity analysis were largely consistent with the base-case decision-tree model. Time to transplant, the percentage of patients experiencing 1-year NRM, and the percentage of patients achieving 1-year OS remained steady across all scenarios of omidubicel-onlv uptake. Increased access to omidubicel-onlv was associated with higher proportions of eligible patients undergoing allo-HCT, a shorter time to allo-HCT, and improved NRM and OS, particularly among racial minorities. Previously, the registrational phase 3 study showed that omidubicel-onlv provides a CD34+ cell dose that is comparable to an adult mobilized peripheral blood stem cell graft [15]. Furthermore, analyses from a prospective substudy of the phase 3 study, which included patients representative of ethnic subgroups, have shown that omidubicel-onlv promotes rapid, balanced, and functional immune reconstitution across both myeloid and lymphoid compartments [29]. The CD34+ content of omidubicel-onlv correlated with faster recovery of the immune cells and coincided with hematopoietic recovery. Similarly, early natural killer and helper T cell reconstitution correlated with a decreased rate of viral infections, suggesting that omidubicel-onlv potentially endows patients with protective immunity by combined hematopoietic and immune recovery [29]. Future studies might consider conducting a similar analysis in pediatric patients with HM and in pediatric and adult patients with nonmalignant HM eligible for allo-HCT for whom MRD were not available. Additionally, a real-world study following omidubicel-onlv uptake in clinical practices (e.g., retrospective observational cohort analysis with data collected from electronic medical records or patient medical charts) could be used to further validate results from this study.
Several studies have addressed disparities in allo-HCT access. The recent 15-MMUD multicenter phase II study sponsored by the NMDP assessed MMUD BMT with post-transplant cyclophosphamide and reported a 1-year OS of greater than 70% [30]. Almost half (48%) of the 80 enrolled patients were from racial and ethnic minority groups, suggesting the feasibility of this approach in expanding allo-HCT access for patients lacking an MUD or MRD. Long-term follow-up outcomes were favorable; the 3-year OS was 70% and 62% for patients who had received reduced intensity or myeloablative conditioning, respectively [31]. The ongoing ACCESS trial is a follow-up to the 15-MMUD study exploring the safety and efficacy of MMUD BMT in pediatric patients as well as MMUD PBSCT in adults [32, 33]. The results from these trials are expected to expand access to MMUD in underserved patient populations, potentially increasing the proportion of patients receiving MMUD in real-world practice. Updating the current study’s model to reflect an increase in MMUD may influence our model’s input assumptions and impact projected outcomes. Additionally, the American Society for Transplantation and Cellular Therapy and the NMDP formed the ACCESS Initiative to directly assess non-donor-related factors with a goal of addressing access barriers and outcome disparities to improve allo-HCT outcomes for all patients [34].
Other factors may impact access to allo-HCT and clinical outcomes. Poor engraftment and survival have been shown in patients who have donor-specific HLA antibodies against the chosen UCB unit [35]. Additionally, we recognize that manufacturing failure (8%) and the time for manufacturing (approximately 21 days) of omidubicel-onlv can exclude some patients from being able to receive therapy because of disease progression [20, 36]. As noted in the registrational phase 3 study [15], a single UCB unit with total nucleated cell dose of at least 1.5 × 107 cells per kg is required, which may not always be available for adult patients. Future processing improvements, including shorter manufacturing time, ability to use UCBs with lower total nucleated cell dose requirement, or the ability to generate off-the-shelf products, may circumvent this issue and extend access of omidubicel-onlv to a broader patient population.
As with any modeling study, limitations with our model should be noted. These include limited generalizability beyond the modeled population and the use of simplifying assumptions where specific data were not readily available. Additionally, inputs such as the utilization and outcomes data used for model inputs were based on historical studies, registries, clinical trials, and assumptions. The projections generated by this model were based on assumed levels of omidubicel-onlv uptake and the translation of clinical trial results into real-world outcomes. Clinical inputs in this present study were based on the best available evidence identified in a targeted literature review, although some of these sources were older studies as a result of a lack of more recent relevant literature on these topics; however, the inputs were reviewed and validated by clinical experts. We did not report on any financial considerations in the use of omidubicel-onlv as compared to other graft sources when looking at access. The present study focused on racial/ethnic disparities due to a lack of optimal donors. However, there are other possible contributors to inequities in the use of allo-HCT for minority patients, such as biologic differences, financial barriers, referral bias, care-seeking challenges, or geographic hurdles. These factors will need to be studied systematically and addressed with campaigns to increase awareness about these advances concomitant with policy changes to achieve the aim of equitable distribution of allo-HCT for underserved patient populations.
Conclusion
This study showed that increased use of omidubicel-onlv in a large, diverse patient population could lead to improvements in transplant use and clinical outcomes, with the greatest benefits seen among racial and ethnic minorities. Thus, increased use of omidubicel-onlv may extend access and possibly improve outcomes to allo-HCT to underserved, eligible patients across racial and ethnic minority groups.
Data Availability
Data are available upon reasonable request from Smitha Sivaraman at smithas@gamida-cell.com.
References
National Marrow Donor Program: Be the Match. Disease-specific HCT indications and outcomes data. https://bethematchclinical.org/transplant-indications-and-outcomes/disease-specific-indications-and-outcomes/. Accessed June 15, 2021.
Kekre N, Antin JH. Hematopoietic stem cell transplantation donor sources in the 21st century: choosing the ideal donor when a perfect match does not exist. Blood. 2014;124:334–43.
Howard CA, Fernandez-Vina MA, Appelbaum FR, et al. Recommendations for donor human leukocyte antigen assessment and matching for allogeneic stem cell transplantation: consensus opinion of the blood and marrow transplant clinical trials network (BMT CTN). Biol Blood Marrow Transplant. 2015;21:4–7.
Gragert L, Eapen M, Williams E, et al. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N Engl J Med. 2014;371:339–48.
Eapen M, Rocha V, Sanz G, et al. Effect of graft source on unrelated donor haemopoietic stem-cell transplantation in adults with acute leukaemia: a retrospective analysis. Lancet Oncol. 2010;11:653–60.
Fingrut WB, Gyurkocza B, Davis E, et al. Racial disparities in access to alternative donor allografts persist in the era of “donors for all.” Blood Adv. 2022;6:5625–9.
Kosuri S, Wolff T, Devlin SM, et al. Prospective evaluation of unrelated donor cord blood and haploidentical donor access reveals graft availability varies by patient ancestry: practical implications for donor selection. Biol Blood Marrow Transplant. 2017;23:965–70.
Landry I. Racial disparities in hematopoietic stem cell transplant: a systematic review of the literature. Stem Cell Investig. 2021;8:24.
Ballen KK, Klein JP, Pedersen TL, et al. Relationship of race/ethnicity and survival after single umbilical cord blood transplantation for adults and children with leukemia and myelodysplastic syndromes. Biol Blood Marrow Transplant. 2012;18:903–12.
Pulte D, Redaniel MT, Jansen L, Brenner H, Jeffreys M. Recent trends in survival of adult patients with acute leukemia: overall improvements, but persistent and partly increasing disparity in survival of patients from minority groups. Haematologica. 2013;98:222–9.
Baker KS, Loberiza FR Jr, Yu H, et al. Outcome of ethnic minorities with acute or chronic leukemia treated with hematopoietic stem-cell transplantation in the United States. J Clin Oncol. 2005;23:7032–42.
Khera N, Hahn TE, Brazauskas R, et al. Trends in use and outcomes of autologous and allogeneic hematopoietic cell transplantation in racial/ethnic minorities. Blood. 2021;138:427.
Mielcarek M, Gooley T, Martin PJ, et al. Effects of race on survival after stem cell transplantation. Biol Blood Marrow Transplant. 2005;11:231–9.
Barker JN, Kurtzberg J, Ballen K, et al. Optimal practices in unrelated donor cord blood transplantation for hematologic malignancies. Biol Blood Marrow Transplant. 2017;23:882–96.
Horwitz ME, Stiff PJ, Cutler C, et al. Omidubicel vs standard myeloablative umbilical cord blood transplantation: results of a phase 3 randomized study. Blood. 2021;138:1429–40.
Horwitz ME, Wease S, Blackwell B, et al. Phase I/II study of stem-cell transplantation using a single cord blood unit expanded ex vivo with nicotinamide. J Clin Oncol. 2019;37:367–74.
Horwitz ME, Chao NJ, Rizzieri DA, et al. Umbilical cord blood expansion with nicotinamide provides long-term multilineage engraftment. J Clin Invest. 2014;124:3121–8.
Peled T, Shoham H, Aschengrau D, et al. Nicotinamide, a SIRT1 inhibitor, inhibits differentiation and facilitates expansion of hematopoietic progenitor cells with enhanced bone marrow homing and engraftment. Exp Hematol. 2012;40:342–55.
Auletta JJ, Kou J, Chen M, et al. Real-world data showing trends and outcomes by race and ethnicity in allogeneic hematopoietic cell transplantation: a report from the Center for International Blood and Marrow Transplant Research. Transplant Cell Ther. 2023;29:346.
OMISERGE prescribing information. April 2023. https://www.fda.gov/media/167202/download. Accessed May 22, 2023.
National Marrow Donor Program, a contractor for the C.W. Bill Young Cell Transplantation Program operated through the U.S. Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau. Donor registry transplant data. Last updated: April 14, 2022.
U.S. Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau. The need for more marrow donors. https://bloodstemcell.hrsa.gov/donor-information/donate-bone-marrow/need-more-marrow-donors. Accessed Apr 15, 2022.
Ciurea SO, Bittencourt MCB, Milton DR, et al. Is a matched unrelated donor search needed for all allogeneic transplant candidates? Blood Adv. 2018;2:2254–61.
Mayani H, Wagner JE, Broxmeyer HE. Cord blood research, banking, and transplantation: achievements, challenges, and perspectives. Bone Marrow Transplant. 2020;55:48–61.
Brunstein CG, Fuchs EJ, Carter SL, et al. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood. 2011;118:282–8.
Matthews AH, Perl AE, Luger SM, et al. Real-world effectiveness of CPX-351 vs venetoclax and azacitidine in acute myeloid leukemia. Blood Adv. 2022;6:3997–4005.
Goldstone AH, Richards SM, Lazarus HM, et al. In adults with standard-risk acute lymphoblastic leukemia, the greatest benefit is achieved from a matched sibling allogeneic transplantation in first complete remission, and an autologous transplantation is less effective than conventional consolidation/maintenance chemotherapy in all patients: final results of the international ALL trial (MRC UKALL XII/ECOG E2993). Blood. 2008;111:1827–33.
Baker M, Wang H, Rowley SD, et al. Comparative outcomes after haploidentical or unrelated donor bone marrow or blood stem cell transplantation in adult patients with hematological malignancies. Biol Blood Marrow Transplant. 2016;22:2047–55.
Szabolcs P, Mazor RD, Yackoubov D, et al. Immune reconstitution profiling suggests antiviral protection after transplantation with omidubicel: a phase 3 substudy. Transplant Cell Ther. 2023;29:517.e1-517.e12.
Shaw BE, Jimenez-Jimenez AM, Burns LJ, et al. National Marrow Donor Program-sponsored multicenter, phase II trial of HLA-mismatched unrelated donor bone marrow transplantation using post-transplant cyclophosphamide. J Clin Oncol. 2021;39:1971–82.
Shaw BE, Jimenez-Jimenez AM, Burns LJ, et al. Three-year outcomes in recipients of mismatched unrelated bone marrow donor transplants using post-transplanation cyclophosphamide: follow-up from a National Marrow Donor Program-sponsored prospective clinical trial. Transplant Cell Ther. 2023;29:208.
Malki MMA, Devine SM, Shaw BE, et al. Access: a multi-center, phase II trial of HLA-mismatched unrelated donor hematopoietic cell transplantation with post-transplantation cyclophosphamide for patients with hematologic malignancies. Blood. 2022;140(suppl 1):7591–3.
National Marrow Donor Program: Be The Match. National Marrow Donor Program/Be The Match announce plan to launch ACCESS clinical trial: assessing HLA-mismatched unrelated donor hematopoietic cell transplantation with post-transplantation cyclophosphamide [press release]. 2021. https://bethematch.org/news/news-releases/national-marrow-donor-program/be-the-match-announce-plan-to-launch-access-clinical-trial/. Accessed 15 Dec 2022.
Auletta JJ, Sandmaier BM, Jensen E, et al. The ASTCT-NMDP ACCESS Initiative: a collaboration to address and sustain equal outcomes for all across the hematopoietic cell transplantation and cellular therapy ecosystem. Transplant Cell Ther. 2022;28:802–9.
Cutler C, Kim HT, Sun L, et al. Donor-specific anti-HLA antibodies predict outcome in double umbilical cord blood transplantation. Blood. 2011;118:6691–7.
Shpall EJ, Rezvani K. Cord blood expansion has arrived. Blood. 2021;138:1381–2.
Medical Writing Assistance
Medical writing support was provided by Christy Chao, PhD, of Evidence Scientific Solutions, Philadelphia, PA, and was funded by Gamida Cell. Analytic support was provided by Ariel Lerner of Analysis Group, Inc., which received consulting fees from Gamida Cell to conduct this study.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
Development of this study, manuscript, and all associated publication costs, including the journal’s Rapid Service and Open Access fees, were funded by Gamida Cell, Boston, MA, USA. The sponsor was involved in design and conduct of the study; analysis and interpretation of the data; preparation, review, and approval of the manuscript; and decision to submit the manuscript for publication. Funding for writing assistance was provided by Gamida Cell, Boston, MA, USA.
Author information
Authors and Affiliations
Contributions
Nandita Khera, Marie Louise Edwards, Yan Song, Rochelle Sun, Rocio Manghani, Heayoung Shin, Ronit Simantov, James Signorovitch, Smitha Sivaraman, and Usama Gergis were involved in the concept/design of the study, data interpretation, and critically reviewed, revised, and approved the manuscript content for publication. Additionally, Marie Louise Edwards, Yan Song, Rochelle Sun, and James Signorovitch were involved in the data analysis.
Corresponding author
Ethics declarations
Conflict of Interest
Rocio Manghani, Heayoung Shin, Ronit Simantov, and Smitha Sivaraman are employees of and own equity holdings with Gamida Cell, Inc. Marie Louise Edwards, Yan Song, Rochelle Sun, and James Signorovitch are employees of Analysis Group, Inc., which received consulting fees from Gamida Cell to conduct this study. Usama Gergis has received consulting fees from and owns stock in Gamida Cell, Inc. Nandita Khera has received consulting fees from Incyte.
Ethical Approval
This analysis is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Additional information
Prior Presentation: Part of the material in this manuscript was presented at the 2022 Tandem Meetings of ASTCT and CIBMTR, April 23–26, 2022, in Salt Lake City, UT and 2022 Annual Cord Blood Connect Meeting, September 9–11, 2022, in Miami Beach, FL as a poster presentation.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Khera, N., Edwards, M.L., Song, Y. et al. Projected Impact of Omidubicel-onlv on Racial/Ethnic Disparities in Allogeneic Hematopoietic Cell Transplantation (Allo-HCT) Outcomes in Hematologic Malignancies. Adv Ther 41, 1637–1651 (2024). https://doi.org/10.1007/s12325-023-02771-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02771-z