Abstract
Introduction
To report eyedrop instillation techniques and factors associated with instillation failure among glaucoma subjects in the Video-Recorded Assessment of Medication Skill and Questionnaire-based evaluation of Perception in Glaucoma Study.
Methods
In this cross-sectional observational study, subjects were 60 patients with glaucoma (mean ± standard deviation age, 68.4 ± 11.3 years; 30 men) who required ocular hypotensive medication(s). Subjects completed ophthalmologic examinations and the Mini-Cog cognitive function test; their typical eyedrop instillation technique was video-recorded. Subjects rated their technique as successes/failures by questionnaire and two examiners rated the successes/failures based on video assessment. Discrepancy between self-reported and video-assessed success/failure rates of instillation was the main outcome measures. Multivariate logistic regression identified factors in instillation failure.
Results
Of 48/56 (86%) self-reported successes, 27/48 (56%) failed based on video assessment; as a result, 32/56 (57%) were inconsistent between subjective and objective assessments. Overall, 30/56 (54%) failed based on video assessment. In the subject-based data model, older age [odds ratio (OR) 0.93/year, P = 0.025] and lower cognitive function score (OR 2.7/score, P = 0.025) were factors in failed instillations. In the eye-based data model, less myopic objective refractive error (OR 0.77/diopter, P = 0.016) and lower visual field foveal threshold (OR 1.1/decibel, P = 0.041) were factors in failures.
Conclusion
In addition to older age, decreased cognitive function, hyperopia, and decreased foveal sensitivity are risks for failed eyedrop instillation. Treating physicians can screen patients who require guidance by checking the risk factors of instillation failure rather than by relying on patient reports.
Similar content being viewed by others
The patient’s ability to instill eyedrops was evaluated through video recordings, and the proportion of patients with glaucoma who instilled eyedrops correctly was clarified in the Video-Recorded Assessment of Medication Skill and Questionnaire-based evaluation of Perception in Glaucoma (VRAMS-QPiG) study. |
Self-assessment of eyedrop technique exhibited discrepancies when compared to evaluations by third parties; over half of the participants who self-reported successful instillation were actually deemed unsuccessful. |
Advanced age, decreased cognitive function, hyperopia, and reduced foveal sensitivity have been identified as risk factors associated with failures in eyedrop instillation. |
The identification of risk factors for eyedrop instillation failures can be a valuable method for identifying patients with glaucoma who would benefit from educational interventions to enhance their eyedrop instillation skills. |
Introduction
Glaucoma is typically treated with intraocular pressure (IOP)-lowering eyedrops [1]. To minimize progression of visual field (VF) defects, patients need to instill eyedrops correctly and continuously [2, 3], although many patients have difficult instilling medications [4] that include directing the drop, turning face-up, avoiding multiple drop instillation, and preventing contamination of the eyedrop bottle tip [5]. Deviations from these basic principles for eyedrop instillation are associated with poor medication adherence/compliance [3, 6]. Furthermore, incorrect instillation interferes with IOP control and increases the risk of drug side effects [7]. Thus, to obtain good medication adherence, patients with glaucoma should eliminate these potential issues associated with eyedrop instillation.
A major problem in the management of glaucoma medication therapy is that patients tend to overestimate their own ability to instill eyedrops [8]. Instillation failure directly affects therapeutic efficacy but is difficult for physicians to detect during daily practice. Understanding the patient's instillation ability and related factors for instillation failure are critical for considering the individual patient guidance by physicians and medical staffs [8]. Several reports have described patients' knowledge of the eyedrop instillation technique and the factors involved in failure to properly instill eyedrops [3, 9,10,11,12]. Previously, advanced age, female sex, concomitant arthritis, severe visual impairment, low corrected visual acuity (VA), worse inferior visual field (VF) defects, low self-efficacy, low education level, and lack of eyedrop training have been reported as factors associated with instillation failure [5, 10, 11]; however, the factors associated with instillation failure have not been fully established.
In this study, the patient ability in eyedrop instillation was assessed using video-recordings, and the proportion of patients with glaucoma who instilled eyedrops correctly was clarified. In addition, factors associated with instillation failure were assessed.
Methods
Study Design and Setting
The Video-Recorded Assessment of Medication Skill and Questionnaire-based evaluation of Perception in Glaucoma (VRAMS-QPiG), a single-center, cross-sectional study, was designed to explore (1) the discrepancy between patient perception of their own eyedrop instillation technique and objective assessment, and (2) the changing effects of subsequent medication education intervention on their perception of the instillation technique. We present the results of part (1) of the study.
All eligible patients were enrolled consecutively at Shimane University Hospital, Japan. All participants provided written informed consent before enrollment. The study was conducted according to the tenets of the Declaration of Helsinki and Ethical Guidelines for Medical and Biological Research Involving Human Subjects in Japan and was approved by the Institutional Review Board of Shimane University Faculty of Medicine, Shimane, Japan (IRB No. 20210209-1; registry ID UMIN000045396).
Study Population
Sixty-two patients provided written informed consent, but two withdrew consent for personal reasons. Ultimately, 60 patients (112 eyes) were enrolled. The inclusion criteria included age of 20 years or older, a diagnosis of glaucoma, and an initial visit to the glaucoma outpatient clinic of Shimane University Hospital from September 2021 to February 2022. To secure the ability to review the recorded videos during the medication guidance conducted later, patients were excluded who had a corrected VA less than 0.3 (in decimal VA) in the better eye or the presence of any problem in viewing the video. Considering the feasibility, we preset the sample size of 60 in this study. With this sample size, the rate of the successful eyedrop instillation assumed to be 50% [4, 8, 11] was predictable with ± 12% (± 95% confidence interval) accuracy.
Observation Procedure
At the outpatient visit, the subjects underwent an ophthalmologic examination and cognitive function testing, and then demonstrated their typical eyedrop instillation technique using artificial tears (Soft SanTear; Santen, Osaka, Japan) while being video-recorded (HDR-CX470; SONY, Tokyo, Japan). After the video-recording, all subjects completed questionnaire-A about their instillation technique and experience. Medical staff members then instructed the subjects on the correct instillation method. Subjects reviewed the recorded video and finally completed questionnaire-B regarding changes in their perception of the eyedrop technique.
Measurements
We recorded each subject’s age, gender, handedness, instillation posture, cognitive function, VA (based on a decimal chart), subjective and refractive errors, VF mean deviation (MD), pattern standard deviation (PSD), foveal sensitivity, and prostaglandin-associated periorbitopathy (PAP) severity. Cognitive function was estimated from 0 (poor) to 5 (good) with the Mini-Cog test [13]. The IOP was measured by Goldmann applanation tonometry. The subjective refractive error was estimated with VA testing, and the objective refractive error was measured by auto-refractometry (TonoRef III; Nidek, Gamagori, Japan). VF indices were obtained using the central 30–2 program with SITA-standard algorithm (Humphrey Visual Field Analyzer; Carl Zeiss Meditec, Dublin, CA, USA). The PAP severity was recorded from 0 (no) to 3 (severe) with the Shimane University PAP grading system [14, 15].
Assessment of Instillation Success/Failure
Subjects were instructed to instill artificial tears based on their normal practice. The entire process was digitally video-recorded. By reviewing the recorded video, the success or failure of eye instillation was judged based on the consensus of two examiners (M.M. and A.T.). Successful instillation was defined as the instillation of one drop in the eye on the first attempt without touching the eye, periocular tissue, and eyelashes [8, 11]. In a subject for whom both eyes were eligible, the instillation in each eye was judged, and for subject based analysis, success was determined when the instillation was successful in both eyes. The subject's self-reported success or failure instillation was recorded based on the answer to the question "Do you think you were able to instill the eyedrops correctly?" in questionnaire-A.
Statistical Analysis
All statistical analyzes were outsourced to KONDO Photo Process (Osaka, Japan) and were performed using IBM SPSS Statistics 28.0 Windows ver. (IBM, Armonk, NY. USA) or R version 4.1.2. The bivariate relationships between the continuous variables were analyzed using Pearson correlation coefficients or Aspin–Welch t tests. For categorical variables, Fisher’s exact probability test or the Wilcoxon rank sum test was used. To assess the factors associated with eyedrop instillation success/failure, multivariate logistic regression analysis was performed. In multivariate analysis, bias derived from both eyes of a patient was adjusted by the mixed-effects model. The multivariate regression model was obtained using the subject- and eye-based data independently. In each model, the independent variable was selected with the stepwise backward elimination method (exclusion threshold, P ≥ 0.05). For the subject-based data model, age, gender, both or right or left eye, instillation posture and Mini-Cog score were considered as candidate variables. For the eye-based data model, age, gender, right or left eye, Mini-Cog score, instillation posture, uncorrected VA in logarithm of the minimal angle of resolution (LogMAR), objective spherical and cylindrical refractive errors, IOP, MD, PSD, foveal sensitivity, and Shimane University (SU)-PAP score were considered as candidate variables. Before establishing the multivariate model, the absence of multi-collinearity among candidate variables was determined by each pair’s Pearson’s correlation coefficient (correlation coefficient, 0.8 or lower). For the eye-based data model, the candidate variables were reduced by excluding the variables with P ≥ 0.25 by univariate logistic regression analysis between the surgical success/failure groups. For calculating LogMAR VA, counting fingers, hand motions, light perception, and no light perception were regarded as decimal VAs of 0.0025, 0.002, 0.0016, and 0.0013, respectively [16].
Results
The subject- and eye-based demographics and clinical characteristics are shown in Tables 1 and 2, respectively. By subject-based aggregation (Table 1), the mean age (± SD) of all patients was 68.4 ± 11.3 years (range, 37–90 years), and more than half of the subjects were 70 years old or older. The patients were evenly divided between men and women. Fifty percentage of subjects achieved a score of 5 (good) on cognitive function testing. By eye-based aggregation (Table 2), more than half of the 112 eyes had primary open-angle glaucoma followed by exfoliation glaucoma. Approximately half of the eyes had uncorrected decimal VA of 0.3 or higher, and more than 90% of them had a corrected decimal VA of 0.3 or higher. The mean refractive errors were myopic with both subjective and objective measurements.
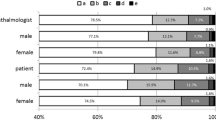
Self-reported and video-assessed rates of success or failure of eyedrop instillation are shown in Table 3. Of 56 subjects with a judgeable video available, 48 (86%) reported that their instillation was successful during the video-recording, while 8 (14%) reported that their instillation was unsuccessful. However, the video assessment by the judges found that 27 (56%) of the 48 subjects “self-reported success” were failures. However, 5 (63%) of 8 subjects with “self-reported failures” were considered successes by video assessment. As a result, success or failure was inconsistent between the self-report and video assessment in 32 (57%) of 56 subjects.
Overall, 30 (54%) of 56 subjects were judged to have failed eye instillation based on video assessment. The reasons for the failures were “instillation of multiple drops in one attempt” in 18 (60%) subjects, and “contact of the bottle tip with eye, periocular tissue, or eyelashes” in 15 (50%). By eye-based aggregation, it appeared that 19 (17%) of 112 eyes even failed to instill eyedrops into the conjunctival sac. While the current study defined failure as the administration of multiple drops in a single attempt, it is worth considering that many patients might perceive using two drops as better than not using any at all. Consequently, the concept of failure in our study and the concept of failure in actual patient care could potentially diverge.
Univariate comparisons of background characteristics between groups stratified by instillation success or failure are shown in Tables 4 (subject-based analysis) and 5 (eye-based analysis). In the failure group, compared with the success group, the age distribution was significantly older, and the Mini-Cog score was significantly worse, while there were no differences in gender, handedness, or instillation posture between the groups (Table 4). The uncorrected VA was significantly worse in the instillation success group than in the instillation failure group, while the corrected VA was equivalent (Table 5). Both subjective and objective spherical refractive errors were significantly myopic in the instillation success group compared with the failure group, while the astigmatic error did not differ between groups (Table 5). VF foveal sensitivity tended to be higher in the success group than in the failure group, while the MD and PSD were equivalent. The SU-PAP score did not differ between the groups (Table 5).
In the subject-based data model of multiple regression analysis, older age [odds ratio (OR), 0.93/year; 95% confidence interval (CI) 0.87–0.99, P = 0.025] and lower cognitive function score (OR 2.7/score; 95% CI 1.1–6.6; P = 0.025) were identified as significant factors in instillation failure. There was no significant interaction between these two factors (OR 1.0; 95% CI 0.94–1.1; P = 0.62). In the eye-based data model, less myopic objective refractive error (OR 0.77/D; 95% CI 0.63–0.95; P = 0.016) and lower VF foveal threshold (OR 1.1/dB; 95% CI 1.0–1.3; P = 0.041) were identified as significant in instillation failure. There was no significant interaction between these two factors (OR 1.0; 95% CI 0.98–1.0; P = 0.50).
Discussion
This study investigated the status of the eyedrop instillation procedure in patients with glaucoma. Despite the high rate (86%) of self-reported instillation success, more than half (54%) of the subjects were judged as “instillation failures”; as a result, the subjects’ own perception and the observation were inconsistent in 57%. Older age, worse cognitive function score, hyperopic refractive error, and worse foveal sensitivity were identified as factors associated with failure. To the best of our knowledge, the last three are unique risk factors of instillation failure in the literature.
Although there were variations due to differences in patient backgrounds, survey methods, and definitions of failure, 10–90% of patients have been reported as unable to instill eyedrops correctly [5]. Accordingly, the current failure rate of 54% agreed with those reported previously. As in previous reports [3,4,5,6,7,8, 10, 17], the need for multiple drop instillations, contact of the bottle tip to the ocular and periocular tissues, and inability to drop the solutions onto the conjunctiva sac were also the major reasons for failure in our study. Instilling multiple drops in one attempt increased waste and led to additional medical costs [9]. Bottle tip contact with the ocular tissues may result in contamination of the bottle and increase the risk of complications such as infection [8, 18]. The inability to instill medication into the conjunctival sac could be more serious in managing glaucoma than other reasons for failure [7, 8], because the target IOP was not reached and led to additional drug prescriptions and glaucoma surgery. With this scenario, the patient burden such as medical expenses and risk of adverse events due to medications/surgeries would increase.
Many patients were unaware of errors in their eyedrop instillation technique [18, 19]; therefore, patients often claimed that there was nothing wrong with instilling the eyedrops themselves [20]. Thus, our results that showed the gap between subjects’ perception and observers could explain this discrepancy. Although the educational intervention by eyedrop guidance was effective, the sustainability of its effect over the long term can be limited [12, 21, 22]. Because the patient's own evaluation of the eyedrop instillation technique is easily overestimated, it seems appropriate to periodically check the instillation methods, explain the correct method, and conduct practical training.
To effectively screen patients with poor instillation skills, the factors associated with such skill are of interest. The previously reported risk factors for instillation failure included advanced age, female sex, concomitant arthritis, severe visual defect, low corrected VA, low self-efficacy, low education level, and lack of eyedrop training [5, 10, 11]. Aging, a commonly detected risk factor in previous [9, 10] and current studies, is reasonable since patient’s physiologic and motor functions are impaired [10]. In our subject-based analysis, a lower cognitive function score was another risk factor. The Mini-Cog cognitive function test is comprised of 3-item word recall and a clock drawing test [13]. Cognitive decline detected by the clock drawing test interfered with the reliability of visual function evaluations such as VF testing [23]. The current study clarified that cognitive function was also related to the success/failure of eye instillation, probably through decline in executive, learning, and/or memory functions [13]. Previous cognitive testing and subsequent modifications of eyedrop instillation guidance (e.g., asking for the assistance of a family member/helper) or medication prescription (e.g., reduced bottle number) might improve glaucoma management in cases with impaired cognitive function. In this regard, the Mini-Cog test can be a good option for screening for cognitive impairment during busy dally practice, since it takes only several minutes.
In the eye-based multiple regression model, subjective spherical refractive error and foveal threshold were associated with instillation failure. By univariate comparisons, both subjective and objective spherical errors shifted clearly to less myopic in the failure group than the success group; worse uncorrected far VA in the success group than failure group reflected well with the less myopic refractive characteristics of the failure group (Table 5). Previously, worse corrected VA and inferior VF defects were associated with instillation failure through patient inability to see the tip of the medication bottle [11]. In the previous and current studies, rather than the general VF defect and distance-corrected VA, decreased central vision and uncorrected near VA can be associated more directly with difficulty in eyedrop instillation in patients with glaucoma. Since the foveal sensitivity checking is set to off in the default setting of the Humphrey Visual Field Analyzer, we recommend that examiners turn it on when the VFs are tested in patients with glaucoma.
The current study had several limitations. Because this study was conducted at the glaucoma clinic of a tertiary hospital, most subjects visited for further IOP reduction; thus, some selection and regional bias might exist. We did not assess the lens status (i.e., crystalline lens or intraocular lens). Considering the mean age of the study subjects was 68.4 years, it is likely that most of the participants had presbyopia, regardless of their lens status. Nonetheless, we cannot disregard the potential influence of differences in accommodative power on our observations (i.e., less myopia was the risk factor), particularly among the younger participants. Absence of near VA data was also a weak point of this study. This study did not assess the treatment duration, patient's physical ability, educational level, and economic status, which might affect the outcome of the instillation success or failure via differences in their proficiency in medication use and understanding of the instructions. A confounding factor that should be considered is that the instillation scene was recorded at the hospital outpatient clinic. Patients might have been conscious of performing tasks more accurately than usual.
Conclusion
Self-assessment of the eyedrop technique was inconsistent with third-party judgment. More than half of the subjects who reported successful instillation were considered failures. Decreased cognitive function, hyperopia, and decreased foveal sensitivity are newly identified risk factors related to eyedrop instillation failure. Checking these factors can be useful to screen for patients with glaucoma who require educational interventions of eyedrop instillation skills.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gedde SJ, Vinod K, Wright MM, et al. Primary open-angle glaucoma preferred practice pattern®. Ophthalmology. 2021;128(1):P71-p150. https://doi.org/10.1016/j.ophtha.2020.10.022.
Juzych MS, Randhawa S, Shukairy A, Kaushal P, Gupta A, Shalauta N. Functional health literacy in patients with glaucoma in urban settings. Arch Ophthalmol. 2008;126(5):718–24. https://doi.org/10.1001/archopht.126.5.718.
Sleath B, Blalock S, Covert D, et al. The relationship between glaucoma medication adherence, eye drop technique, and visual field defect severity. Ophthalmology. 2011;118(12):2398–402. https://doi.org/10.1016/j.ophtha.2011.05.013.
Schwartz GF, Hollander DA, Williams JM. Evaluation of eye drop administration technique in patients with glaucoma or ocular hypertension. Curr Med Res Opin. 2013;29(11):1515–22. https://doi.org/10.1185/03007995.2013.833898.
Davis SA, Sleath B, Carpenter DM, Blalock SJ, Muir KW, Budenz DL. Drop instillation and glaucoma. Curr Opin Ophthalmol. 2018;29(2):171–7. https://doi.org/10.1097/icu.0000000000000451.
Shu YH, Wu J, Luong T, et al. Topical medication adherence and visual field progression in open-angle glaucoma: analysis of a large US health care system. J Glaucoma. 2021;30(12):1047–55. https://doi.org/10.1097/ijg.0000000000001943.
Gupta R, Patil B, Shah BM, Bali SJ, Mishra SK, Dada T. Evaluating eye drop instillation technique in glaucoma patients. J Glaucoma. 2012;21(3):189–92. https://doi.org/10.1097/IJG.0b013e31820bd2e1.
Stone JL, Robin AL, Novack GD, Covert DW, Cagle GD. An objective evaluation of eyedrop instillation in patients with glaucoma. Arch Ophthalmol. 2009;127(6):732–6. https://doi.org/10.1001/archophthalmol.2009.96.
Hennessy AL, Katz J, Covert D, Protzko C, Robin AL. Videotaped evaluation of eyedrop instillation in glaucoma patients with visual impairment or moderate to severe visual field loss. Ophthalmology. 2010;117(12):2345–52. https://doi.org/10.1016/j.ophtha.2010.03.040.
Kashiwagi K, Matsuda Y, Ito Y, et al. Investigation of visual and physical factors associated with inadequate instillation of eyedrops among patients with glaucoma. PLoS ONE. 2021;16(5):e0251699. https://doi.org/10.1371/journal.pone.0251699.
Naito T, Namiguchi K, Yoshikawa K, et al. Factors affecting eye drop instillation in glaucoma patients with visual field defect. PLoS ONE. 2017;12(10):e0185874. https://doi.org/10.1371/journal.pone.0185874.
Sayner R, Carpenter DM, Robin AL, et al. How glaucoma patient characteristics, self-efficacy and patient-provider communication are associated with eye drop technique. Int J Pharm Pract. 2016;24(2):78–85. https://doi.org/10.1111/ijpp.12215.
Borson S, Scanlan JM, Chen P, Ganguli M. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51(10):1451–4. https://doi.org/10.1046/j.1532-5415.2003.51465.x.
Ishida A, Miki T, Naito T, Ichioka S, Takayanagi Y, Tanito M. Surgical results of trabeculectomy among groups stratified by prostaglandin-associated periorbitopathy severity. Ophthalmology. 2022. https://doi.org/10.1016/j.ophtha.2022.10.024.
Tanito M, Ishida A, Ichioka S, et al. Proposal of a simple grading system integrating cosmetic and tonometric aspects of prostaglandin-associated periorbitopathy. Medicine (Baltimore). 2021;100(34):7e26874. https://doi.org/10.1097/md.0000000000026874.
Grover S, Fishman GA, Anderson RJ, et al. Visual acuity impairment in patients with retinitis pigmentosa at age 45 years or older. Ophthalmology. 1999;106(9):1780–5. https://doi.org/10.1016/s0161-6420(99)90342-1.
Davies I, Williams AM, Muir KW. Aids for eye drop administration. Surv Ophthalmol. 2017;62(3):332–45. https://doi.org/10.1016/j.survophthal.2016.12.009.
Hennessy AL, Katz J, Covert D, et al. A video study of drop instillation in both glaucoma and retina patients with visual impairment. Am J Ophthalmol. 2011;152(6):982–8. https://doi.org/10.1016/j.ajo.2011.05.015.
Tatham AJ, Sarodia U, Gatrad F, Awan A. Eye drop instillation technique in patients with glaucoma. Eye (Lond). 2013;27(11):1293–8. https://doi.org/10.1038/eye.2013.187.
Brown MM, Brown GC, Spaeth GL. Improper topical self-administration of ocular medication among patients with glaucoma. Can J Ophthalmol. 1984;19(1):2–5.
Feng A, O’Neill J, Holt M, Georgiadis C, Wright MM, Montezuma SR. Success of patient training in improving proficiency of eyedrop administration among various ophthalmic patient populations. Clin Ophthalmol. 2016;10:1505–11. https://doi.org/10.2147/opth.S108979.
Lazcano-Gomez G, Castillejos A, Kahook M, Jimenez-Roman J, Gonzalez-Salinas R. Videographic assessment of glaucoma drop instillation. J Curr Glaucoma Pract. 2015;9(2):47–50. https://doi.org/10.5005/jp-journals-10008-1183.
Raman P, Khy Ching Y, Sivagurunathan PD, Ramli N, Mohd Khalid KH. The association between visual field reliability indices and cognitive impairment in glaucoma patients. J Glaucoma. 2019;28(8):685–90. https://doi.org/10.1097/ijg.0000000000001269.
Acknowledgements
Medical Writing/Editorial Assistance
Statistical analysis and data management were performed by the Data Research Section, KONDO Photo Process Co., Ltd. (Osaka, Japan). Medical writing and editorial support for this manuscript was provided by Naruhiro Ishida, PhD (Santen Pharmaceutical Co., Ltd.). Technical assistance was supported by Etsuyo Miyamoto and Naomi Otsuka (Santen Pharmaceutical Co., Ltd.). Statistical interpretation support was provided by Kazunori Santo, MSc (Santen Pharmaceutical Co., Ltd.). The funding for this writing support was provided by Santen Pharmaceutical Co., Ltd. Mini-Cog was used in this study under permission from Dr. Soo Borson, MD, University of Washington.
Funding
Financial support for this study and its publication, including the journal’s Rapid Service and Open Access Fees, was provided by Santen Pharmaceutical Co., Ltd. (Osaka, Japan). The sponsor participated in the design of the study; management, interpretation of the data; preparation, review, and approval of the manuscript.
Author information
Authors and Affiliations
Contributions
Masaki Tanito, Yumiko Kataoka, Yasutaka Takagi, and Daisuke Shii were involved in the conceptualization and design of the study and Masaki Tanito, Mihoko Mochiji, Aika Tsutsui, Akiko Harano, Sho Ichioka, and Yuji Takayanagi were involved in data collection. All authors were involved in analysis and interpretation of data, drafting the article, revising it critically, and final approval of the version to be submitted. All authors attest that they meet the current ICMJE criteria for authorship.
Corresponding author
Ethics declarations
Conflict of Interest
Masaki Tanito had research funding from Santen Pharmaceutical Co., Ltd.. Yumiko Kataoka, Yasutaka Takagi and Daisuke Shii are employees of Santen Pharmaceutical Co., Ltd. Mihoko Mochiji, Aika Tsutsui, Akiko Harano, Sho Ichioka, and Yuji Takayanagi have no conflict of interest to disclose.
Ethical Approval
The study was conducted according to the tenets of the Declaration of Helsinki and Ethical Guidelines for Medical and Biological Research Involving Human Subjects in Japan and was approved by the Institutional Review Board of Shimane University Faculty of Medicine, Shimane, Japan (IRB No. 20210209-1; registry ID UMIN000045396). All participants provided written informed consent before enrollment.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tanito, M., Mochiji, M., Tsutsui, A. et al. Factors Associated with Topical Medication Instillation Failure in Glaucoma: VRAMS-QPiG Study. Adv Ther 40, 4907–4918 (2023). https://doi.org/10.1007/s12325-023-02646-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02646-3