Abstract
Introduction
The efficacy of prolonged-release fampridine (PR-FAM) may extend in multiple sclerosis (MS) beyond walking ability. The objective of this study was to evaluate the effect of PR-FAM treatment on cognition, fatigue, depression, and quality of life (QoL) in adult patients with MS in a real-world setting.
Methods
FAMILY was a multi-center, prospective, observational, real-world cohort study of MS patients receiving PR-FAM in the outpatient setting. Patients were treated as per PR-FAM’s local prescribing information for 6 months. Standardized protocols and questionnaires were used to evaluate changes in cognition (PASAT; Paced Auditory Serial Addition Test), fatigue (MFIS; Modified Fatigue Impact Scale), depression (BDI-II; Beck Depression Inventory-II) and QoL (MusiQoL; MS International Quality-of-Life questionnaire, MSIS-29; Multiple Sclerosis Impact Scale: PHYS and PSYCH subscales) at 3 and 6 months compared to baseline.
Results
In total, 102 eligible patients from 8 sites in Greece were analysed, of whom 92 completed the study and 10 discontinued. At 6 months, PR-FAM treatment resulted in improvements from baseline in PASAT-3′′ (p = 0.044), MFIS (p < 0.001), BDI-II (p < 0.001), MusiQoL (p < 0.001) and MSIS-29-PHYS (p = 0.012) and MSIS-PSYCH (p < 0.001). A positive effect was evident already at 3 months in PASAT-3′′ (ns), MFIS (p = 0.020), BDI-II (p = 0.034), MusiQoL (p = 0.001), MSIS-29-PHYS (ns) and MSIS-29-PSYCH (p < 0.001).
Conclusions
This observational study provides new data to the current literature in support of PR-FAM’s positive effects in cognition, fatigue, depression, and QoL in a large, heterogeneous group of Greek MS patients in the real-world setting.
Trial Registration
ClinicalTrials.gov identifier, NCT03164018.
Similar content being viewed by others
PR-FAM was effective in improving cognition, fatigue, depression and QoL in patients with MS in daily clinical practice. |
Patients with a clinically significant improvement in their walking speed also experienced more pronounced improvements in fatigue, depression, and QoL. |
Future studies are needed to further characterize the impact of PR-FAM on these non-walking variables as well as the possible link between them and walking ability. |
Digital Features
This article is published with digital features, including summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13352804.
Introduction
Multiple sclerosis (MS) is a progressive demyelinating inflammatory disease of the central nervous system (CNS), resulting in long-term physical disability with difficulties in walking being the major manifestation [1]. Beyond walking difficulty, other symptoms further constitute a long-term burden in patients affected by MS [2]. Cognitive impairment, fatigue and depression are highly prevalent in MS patients and fundamental for the overall QoL of these patients [3, 4]. Fatigue is among the most common symptoms in MS, reported by up to 80% of patients [5, 6]. For many patients, fatigue is considered the single most debilitating symptom, surpassing even physical disability [7]. Although many drugs have been tested in multiple clinical trials, oral treatments able to improve the levels of MS-related fatigue in a satisfactory manner remain scarce, reflecting our poor understanding of the underlying processes of fatigue in MS [8]. MS is also characterized by cognitive impairment occurring from the early phases of the disease, with at least half of all MS patients exhibiting some degree of cognitive decline at some point during their disease course [9, 10]. Although MS-related cognitive decline is usually heterogeneous in nature, there are certain cognitive aspects that are more vulnerable than others. Information processing speed and memory are not only the key cognitive functions most often impaired in MS [9] but their impairment may also be an early predictor of motor disability progression [10]. Similarly to cognitive impairment and fatigue, the prevalence of depression in patients suffering from MS is remarkably high; it is estimated that the presence of depression in patients with MS is 2–3 times higher than in the general population [11]. Interestingly, according to a recent longitudinal cohort study, patients with MS and comorbid depression have a significantly increased risk of disability worsening, emphasizing the rigorous need for early recognition and effective management of depression [12]. Patient and physician perspectives of the disease-related QoL (HRQoL) have been shown to be quite divergent, with the latter traditionally equating health to the absence or improvement of MS symptoms and not to the patient’s overall physical, mental, and social welfare. In recent decades, however, patient-reported HRQoL outcome measures are also being considered increasingly relevant for the evaluation of disease progression, treatment response, and the level of support needed by MS patients [13].
PR-FAM is a voltage-dependent potassium channel blocker known to enhance action-potential conduction in demyelinated nerve fibres and to facilitate synaptic transmission [14]. To date, it is the only symptomatic treatment approved for walking disability in MS adult patients (Expanded Disability Status Scale; EDSS 4–7). It received approval by the European Medicines Agency (EMA) in 2017, following a “conditional” approval in 2011 subject to the provision of further evidence with regard to PR-FAM’s long-term clinically meaningful therapeutic benefit [15, 16]. Given the assumed effects of PR-FAM on demyelinated axonal fibres at multiple sites along the CNS, PR-FAM’s positive effects on other neurological functions beyond ambulatory function are likely [17, 18]. Within this context, PR-FAM could also potentially improve fatigue, cognitive function, and mood directly through restoration of action potential conduction. Alternatively, PR-FAM-induced changes in one symptom may indirectly trigger secondary changes in other symptoms [19].
While more and more evidence has emerged in recent years in favour of positive effects of short- and long-term treatment with PR-FAM on ambulatory function [20, 21], data demonstrating a possible long-term effect of the drug on non-walking functional outcomes are either still limited or discordant. Apart from one randomized, placebo-controlled study describing PR-FAM’s beneficial effects on different cognitive domains as well as on fatigue and depression over 2 years in a cohort of MS patients [18], most studies conducted so far, utilizing a randomized, placebo-controlled design, have failed to demonstrate fampridine’s benefits in such non-walking outcomes [22,23,24,25]. On the other hand, a limited number of open-label, uncontrolled studies have already described PR-FAM-induced improvements in fatigue, cognition, mood and overall QoL [4, 17, 19, 26,27,28,29,30,31]. Whereas these studies offer valuable information towards a possible role of PR-FAM on these functions, data remain unclear, with variabilities in study parameters, including study design, treatment algorithms and assessment protocols, do not allowing the drawing of univocal conclusions [32]. Thus, the aim of the FAMILY study was to complement existing literature with new real-life data regarding the effects of (6-month) treatment with PR-FAM on cognition, fatigue, depression and QoL in adult patients with MS as treated in daily clinical practice in Greece.
Methods
Study Design
FAMILY was a multi-center, prospective, observational, real-world cohort study of MS patients receiving PR-FAM in the outpatient setting. Patients were enrolled consecutively to avoid selection bias. Patients were treated for 6 months according to the local prescribing information of PR-FAM and the routine medical practice in terms of visit frequency and types of assessments. Notably, the decision to prescribe PR-FAM had already been taken prior to their study enrolment and was clearly separated from the physician’s decision to include them in the study. Assessments were performed at commencement (baseline), after 2, 12 and 24 weeks of treatment with PR-FAM. At baseline, patients’ walking ability was assessed by the physician using the Timed 25-Foot Walk test (T25FW) [33, 34] and the self-reported 12-item Multiple Sclerosis Walking Scale (MSWS-12) [35]. Patients’ cognitive function was assessed by the Paced Auditory Serial Addition Test (PASAT) [33, 34]. Patients were also asked by the physician to complete the following self-administered questionnaires: Modified Fatigue Impact Scale (MFIS) [36, 37], Beck Depression Inventory-II (BDI-II) [38, 39], MS International Quality-of-Life questionnaire (MusiQoL) [40, 41] and Multiple Sclerosis Impact Scale (MSIS-29) [42]. After 2 weeks on treatment with PR-FAM, patients’ walking ability was re-assessed, and physicians made a decision regarding patients’ response to PR-FAM as per their clinical judgement. At Weeks 12 and 24, patients underwent the same tests as performed at baseline. All serious and non-serious adverse events (AEs), occurring from the time of signing the Informed Consent Form (ICF) throughout the treatment period and until 14 days of study completion, were reported in patients’ medical records and in the relevant study documentation as per the study protocol and the local regulations.
The study was conducted in compliance with the principles laid down in the Declaration of Helsinki as well as with the local regulatory requirements, with approval obtained by the Ethics Committee of each participating site. A list of the respective Ethics Committees is included in Table S1. Written informed consent was obtained from all individual participants included in the study.
Inclusion and Exclusion Criteria
Patients eligible to participate in the study were: (1) adults (≥ 18 years old) with MS (McDonald 2017 criteria) [43]; (2) receiving PR-FAM for walking disability (EDSS 4–7) in line with the locally approved Summary of Product Characteristics (SmPC); and (3) receiving stable doses of any MS disease-modifying treatment (DMT) for at least 3 months prior to study entry. Exclusion criteria were: (1) having received more than 1 dose of PR-FAM at the time of enrolment; (2) meeting any of the contra-indications of the approved SmPC; and (3) receiving or having received treatment with any investigational product within 1 month or 5 half-lives of the investigational agent (whichever is longer) prior to commencement of PR-FAM.
Outcome Measures
The primary efficacy endpoints of the study were changes from baseline in the mean score of PASAT, BDI-II, MFIS, MSIS-29 and MusiQoL. PASAT is a measure assessing auditory information processing speed and flexibility, as well as calculation ability. It is widely used for assessing the cognitive function in several brain conditions. In this study, the version applying intervals of 3 s, thereafter referred to as “PASAT 3′′” was employed, as described in the Multiple Sclerosis Functional Composite (MSFC) [33, 34]. Changes in fatigue were assessed using the MFIS, which provides a self-reported assessment of physical, cognitive, and psychosocial functioning [36, 37]. The BDI-II, a 21-item self-report measure of the severity of depressive symptoms, was further utilized [38, 39]. Changes in the QoL of MS patients were assessed using two MS-specific instruments, the MusiQoL [40, 41] and the MSIS-29 [42]. The physical scale (MSIS-29-PHYS) consisting of 20 questions, and the psychological scale (MSIS-29-PSYCH) of 9 questions were applied separately [42]. Changes in walking speed were assessed using the T25FW as described in the MSFC [33, 34]. Patients were allowed to use an assistive device as long as it was consistently used across visits. The task was performed twice at each visit and an average score of the two completed trials was calculated.
Statistical Analysis
Statistical analysis was performed using IBM SPSS v.24. For all efficacy analysis as well as the description of baseline demographics and disease characteristics, the Modified Intention-to-Treat (mITT) population was used, defined as all subjects enrolled in the study with at least one post-baseline efficacy assessment, excluding those not fulfilling inclusion/exclusion criteria after objective examination according to ICH E9 guideline. Summary statistics were used to describe patients’ demographic and disease-related characteristics at baseline as well as test scores at different timepoints. Continuous parameters were presented as mean, median and standard deviation (SD), whereas categorical variables were presented as absolute (n) and relative (%) frequencies. The paired samples t test was implemented to evaluate the impact of PR-FAM administration on patient test score changes from baseline to Weeks 12 and 24. The statistical significance of the proportion of patients with ≥ 20% improvement in the T25FW at each study visit was assessed using a binomial test and the respective 95% confidence interval (CI); improvement was defined as a 20% increase of walking speed at T25FW. Walking times, transformed into speeds (more normally distributed than time), were averaged giving 1 value per visit. Changes in average walking speed on treatment are reported as percent change from baseline. A positive percent change indicated patients who walked faster following treatment [35]. P values < 0.05 were considered statistically significant. The ‘last observation carried forward’ approach was used to handle missing data. All patients enrolled in the study who were administered at least one dose of PR-FAM during the study period were used for the safety analysis (Safety Analysis Set; SAF). All AEs, occurring from the time of signing the ICF throughout the treatment period and until 14 days of study completion, were summarised by number and percentage of patients with each AE.
Results
A total of 119 patients (ITT population) were enrolled at 8 sites in Greece from 07/03/2017 to 15/12/2018 and thus were treated with PR-FAM. Among them, 106 completed the study and 13 discontinued from the study. After objective evaluation as per the ICH E9 principles, 17 patients were found not to fulfill all the inclusion criteria or to fulfill one of the exclusion criteria, and thus were identified as having erroneously been enrolled in the study. Therefore, 102 were finally deemed eligible and were included in the efficacy analysis (mITT), of whom 92 completed the study and 10 discontinued. The most frequent reason for study discontinuation was no response to treatment (4 patients, 3.9%) followed by lost to follow-up/non-adherence (3 patients, 2.9%) (Fig. 1).
Patients' demographics and disease characteristics at baseline are presented in Table 1. The vast majority of patients (79.4%) were diagnosed with relapsing–remitting MS (RRMS) according to the McDonald 2017 criteria [43]. The mean ± SD time since MS diagnosis was 11.44 ± 7.83 years. Only 16 (15.7%) patients had experienced at least one relapse during the last year before commencing treatment with PR-FAM, with 3 of them experiencing a relapse in the last month prior to PR-FAM treatment initiation. Patients had an EDSS score (median) of 4.0. At baseline, all patients (mITT) were receiving a DMT for their MS for at least 3 months prior to study entry, with fingolimod (33.3%) being the most frequently used DMT, followed by natalizumab (16.7%) and dimethyl fumarate (9.8%). Forty-seven (46.08%) patients were also receiving at least one concomitant medication, with nervous system (34.31%), musculoskeletal system (13.73%), genito-urinary system (11.76%), alimentary tract and metabolism (9.8%), systemic hormonal preparations, excluding sex hormones (7.8%), and cardiovascular system (6.86%) medications being the most common classes. Moreover, 39.22% of patients had at least one clinical diagnosis other than MS, with psychiatric disorders (23.53%) being the most commonly reported, followed by endocrine disorders (9.80%), nervous system disorders (7.84%), renal and urinary disorders (7.84%), vascular disorders (6.86%) and musculoskeletal and connective tissue disorders (3.92%).
Cognition
At baseline, patients achieved a PASAT-3′′ score of 30.64 ± 21.358 units; at 6 months (Week 24) from baseline, cognitive function was improved as reflected by a statistically significant increase of PASAT-3′′ score to 31.72 ± 21.874 units (p = 0.044). While a similar trend was already observed at 3 months from baseline (Week 12) with a mean PASAT-3′′ score of 31.20 ± 21.680, this did not reach statistical significance (Table 2).
Fatigue
The total MFIS score was 36.68 ± 16.981 units at baseline, whereas, at 6 months (Week 24), a statistically significant improvement of fatigue to 32.77 ± 16.123 was observed (p < 0.001). A statistically significant decrease in total MFIS score was already evident at 3 months (Week 12) with a score of 34.45 ± 17.272 being observed (p = 0.020) (Table 2).
Depression
Mood as measured by the BDI-II score improved from baseline to 6 months (Week 24) from 11.34 ± 8.031 to 9.17 ± 7.660 units and this change was statistically significant (p < 0.001). A decrease in depressive symptoms was already observed at 3 months (at Week 12) when the score was decreased to 10.41 ± 8.003 (p = 0.034) (Table 2). During a post hoc subgroup analysis, changes from baseline in BDI-II score at 6 months were compared across two subgroups of patients defined by concomitant use of anti-depressants, anxiolytics, psychostimulants and other nervous system medications known to affect mood. Results from this analysis revealed that mean change in BDI-II score from baseline to Week 24 consistently improved (i.e. decreased) with no statistically significant difference across the two subgroups as defined by concomitant use of such medications (Table 3).
Quality of Life
With regards to MS-related QoL as assessed by MusiQoL, at baseline, patients achieved a score of 63.45 ± 16.493, with an improvement at 6 months (Week 24) as reflected by a statistically significantly increase in score to 67.75 ± 15.247 (p < 0.001). An improvement in QoL as reflected by a statistically significant increase in MusiQoL score was already evident at 3 months (Week 12) with a mean score of 65.86 ± 15.975 units being observed (p = 0.001) (Table 2).
The MSIS-29-PHYS scale also demonstrated an MS-related QoL improvement, with a mean score decreasing from 32.00 ± 18.103 at baseline to 28.13 ± 17.007 units at 6 months (Week 24) and this decrease was statistically significant (p = 0.012). At 3 months, a decrease to 29.90 ± 17.380 units was also observed, although not statistically significant (p = 0.124). MS-related QoL was improved, as also shown by the MSIS-PSYCH scale, with the mean score being significantly lower at 6 months compared to baseline, with reported scores being 24.64 ± 23.301 and 32.11 ± 26.533, respectively (p < 0.001). Consistently, mean score at 3 months (Week 12) was 27.23 ± 23.025 which is also lower than baseline (p < 0.001) (Table 2). Of note, during the post hoc subgroup analysis, changes from baseline in MSIS-PSYCH scale at 6 months were also compared across the two subgroups of patients defined by concomitant use of anti-depressants, anxiolytics, psychostimulants and other nervous system medications known to affect mood. Results from this analysis revealed that mean change in MSIS-PSYCH score from baseline to Week 24 consistently improved (i.e. decreased) with no statistically significant difference across the two subgroups as defined by concomitant use of such medications (Table 3).
Walking Ability
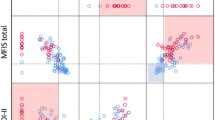
Following 14 days of treatment with PR-FAM (Week 2), 14.4% of patients experienced an improvement in their walking speed of at least 20% as assessed by the T25FW with this percentage slightly increasing at Week 12 (18.3%) and Week 24 (19.8%) (Table 4). When patients were sub-grouped according to improvement in T25FW performance from baseline to Week 12, those with a ≥ 20% improvement, i.e. 17 patients, showed an improvement in MFIS (p < 0.001), BDI-ΙΙ (p = 0.047) and MSIS-29 PHYS (p = 0.009) as compared to the rest of the population (i.e. 76 patients with < 20% T25FW improvement) (Table 5). Similarly, patients with ≥ 20% improvement in their walking speed at Week 24, i.e. 18 patients, showed statistically significant improvements in MFIS (p < 0.001), BDI-II (p = 0.004), MusicQoL (p = 0.030), MSIS-29- PHYS (p = 0.002) and MSIS-29 PSYCH (p = 0.037) as compared to the rest of the population, i.e. 73 patients (Table 5).
Safety
Twenty-three (19.3%) out of 119 patients (SAF) reported at least one AE, 9 (7.56%) reported at least one AE possibly related to PR-FAM and 3 (2.52%) reported at least one AE that led to drug discontinuation. No serious adverse event (SAE) was reported. The most commonly reported AE was headache (5.04%) (Table 6). Overall, the incidence of AEs was consistent with the known safety profile of PR-FAM and did not reveal any new safety signal for PR-FAM.
Discussion
Current evidence from early real-world clinical experience points towards PR-FAM’s broader benefits on other MS-related facets beyond those on walking ability [1]. In support of this notion, our study showed that treatment with PR-FAM for 6 months led to significant improvements in cognition, fatigue, depression and QoL in a large, heterogeneous group of Greek MS patients in everyday clinical practice.
According to our results, information processing speed, a core aspect of cognition, as assessed by PASAT-3′′ was significantly superior to baseline values after 6 months on treatment with PR-FAM. These findings are consistent with a number of previous studies which also reported an improvement in PASAT after short- or long-term treatment with PR-FAM [17, 24, 26]. Studies utilizing the Symbol Digit Modalities Test (SDMT) further corroborate these results by demonstrating an improvement in visual processing speed after short- and long-term treatment with PR-FAM [28, 30, 44, 45]. In contrast, some studies failed to demonstrate an impact of PR-FAM on cognitive function, as assessed either by PASAT or SDMT [24, 27, 31]. Interestingly, in the study of Satchidanand et al. (2020), while there was no effect of fampridine on cognitive outcomes when compared with placebo, performance in PASAT but not in SDMT improved significantly among “responders” in the treatment group compared with “non-responders”, reflecting a possible cognition–motor coupling [31]. A recently conducted meta-analysis showed conflicting results with regards to the effect of PR-FAM on cognitive function. Nevertheless, these parameters were secondary outcomes in the reviewed studies with only some cohort studies focusing on them and finding a positive effect of PR-FAM on cognitive, emotional and speech functions [32]. Our findings, together with others’, are quite encouraging but warrant more in-depth examination. Information processing speed is a domain of cognitive function that may be favoured by treatment with PR-FAM. This favourable PR-FAM effect could be interpreted in part by PR-FAM’s ability to cross the blood–brain barrier (BBB) and potentially target disseminated demyelinated lesions in different associative brain regions, ultimately resulting in an improvement in nerve conduction [46]. However, assuming that PR-FAM enhances nerve conduction resulting in faster processing speed is a rather superficial explanation of how increased conduction on a neural level can lead to an improvement in more complex cognitive processes [47]. Thus, further understanding of how MS disease leads to patterns of cognitive decline is needed to drive therapeutic decisions. Ιt should also be noted that all studies assessing fampridine’s effects in cognitive function conducted so far were limited to rather crude tests including PASAT or SDMT. In that sense, interpretation of performance of MS patients in PASAT-3′′ during our study may also have been confounded by secondary factors, including variations in premorbid intelligence, sensory-motor impairment, fatigue, depression and overall emotional status during performing the test [9]. Moreover, PASAT performance may also have been subject to practice effects upon repeated administration [33, 48]. Taken together, although there are clear limitations to its use, PASAT remains a measure highly sensitive to certain cognitive functions frequently affected in MS, although not intended to be a global measure of cognitive dysfunction [33]. Thus, future studies assessing PR-FAM’s benefits applying a more comprehensive neuropsychological assessment should be designed.
Similar to our results, which demonstrated improvement in fatigue at 6 months, most previous studies demonstrated short- and long-term improvements in fatigue in MS patients following PR-FAM treatment [4, 17,18,19, 25,26,27,28,29, 49]. Notably, in the study of Korsen et al. (2017), response to PR-FAM treatment was dependent on the responder status (determined based on a ≥ 20% improvement in T25FW), while no effects were observed in the total patient cohort [17]. Interestingly, a randomized, placebo-controlled trial, although failing to show a difference between fampridine and placebo in terms of fatigue amelioration, did show a significant improvement in fatigue in those patients with a high blood concentration of fampridine [25]. Although the pathophysiology of fatigue remains poorly understood, the primary mechanism that seems to be mostly consistent with a response to fampridine is fatigue due to demyelination and axonal loss that leads to increased axonal energy demands required for conduction [19, 50]. Thus, the improvement of fatigue noted in our study and previous studies may once again be attributed to PR-FAM’s potential ability to cross the BBB and improve conduction of demyelinated axons [46]. Another possible explanation may lie in improvements in secondary factors comprising underlying causes of fatigue within the context of MS. Depression comprises one such factor, with anti-depression treatments in MS patients also reducing fatigue [27].
Our study also demonstrated an improvement in the depressive status of MS patients after the 6-month treatment with PR-FAM. Only a limited number of studies investigating PR-FAM’s potential effect on depression have been conducted so far. One study demonstrated a short-term benefit on depression following a 14-day treatment with PR-FAM [27]. These observations were extended by another study demonstrating PR-FAM’s positive effects on depressive symptoms over 2 years in a cohort of MS patients; of note, responsiveness in depression did not coincide with an improvement in ambulatory function [18]. On the contrary, no positive effect on depression was reported after 6 and 12 months of PR-FAM treatment in a recent real-life study also conducted within Greece [28]. Given that fatigue and depression are closely interrelated with a similar pathophysiological mechanism even being speculated within the context of MS, it is not surprising that a paralleled improvement was observed in both variables. Therefore, the improvement in fatigue during our study may be partly attributed to the reduction of depressive symptoms and vice versa. However, the possibility that improvement in those two MS aspects may have occurred independently cannot be fully excluded.
We also found positive results in terms of PR-FAM’s effect on the QoL of MS patients after 6 months as assessed using two different MS-specific questionnaires. Previous studies have similarly reported a long-term improvement in MS-related QoL, as reflected in both MSIS-29 subscales [28, 51]. Significant improvement from baseline in MSIS-29-PHYS in favour of PR-FAM after a 24-week treatment was also reported during ENHANCE, the largest and longest randomized trial of PR-FAM to date [22]. In line with these positive results, significant improvements in QoL, as captured by general patient-reported and MS-specific measures, were observed over 48 weeks in ENABLE [52]. A meta-analysis also showed that PR-FAM has a positive effect on patient satisfaction and QoL, although all the analyses except for one were based on responders [32]. Given the demonstrated efficacy of PR-FAM in the ambulatory function, a consequent improvement in health-related QoL of MS patients is therefore not surprising. Additionally, such an improvement may also be the result of PR-FAM-driven changes in other non-walking aspects than those investigated in this study.
With regard to a clinically significant response to PR-FAM, in terms of lower limb function, data from placebo-controlled randomized studies consistently report the proportion of patients achieving a clinically significant improvement as roughly 35–42% [21]. An increase of ≥ 20% in the T25FW has been widely suggested as a minimal clinically important difference (MCID) [53], but it is unclear if this outcome best identifies short- and long-term clinically meaningful responses to PR-FAM in the setting of real clinical practice. Most studies conducted in a real-world setting, mainly considering improvement in the T25FW as MCID, have yielded similar results to the pivotal clinical trials [21]. Nevertheless, in our study, a marginally increasing trend was observed over time in the proportion of patients with a ≥ 20% T25FW improvement, implying that some patients may have a slower response to PR-FAM. This percentage was consistently found to be lower than expected over the course of the study, ranging from only 14.2% to a maximum of approximately 20% after 2-, 12- and 24-week treatments with PR-FAM. In current routine clinical practice, the neurologist is responsible for assessing treatment response to PR-FAM, which must be discontinued in patients not showing any improvement on the basis of walking ability after 2–4 weeks of treatment. In our study, although a small number of patients demonstrated a ≥ 20% improvement in T25FW after 2 weeks on PR-FAM, the majority of patients continued treatment for up to 6 months.
Neurologists in our study seem to have relied their decision to determine patients’ response to PR-FAM over time not only upon changes in walking speed but also upon their global judgement of walking ability as well as patients’ overall status; an approach critically acclaimed in the recent literature [1, 21]. Interestingly, despite this general limited improvement in walking speed, beneficial effects were observed in all other aspects of relevance to MS, i.e. cognition, fatigue, depression and QoL. Moreover, additional analyses on changes over time in the primary efficacy measures between patients who did or did not achieve a ≥ 20% improvement in the T25FW revealed that this ≥ 20% improvement was accompanied by improvements in the fatigue, depression and QoL aspects of MS. These results suggest that the presence of improvement in walking ability is an important but not the sole indicator of improvement in these perceived aspects.
Potential limitations of this study are those mainly associated with its non-interventional nature, including the lack of a control group, which leads to a risk of confounding and bias, making it difficult to ascribe the positive outcomes observed for PR-FAM itself. In our study, there is also an apparent presence of comorbidities and concomitant medications, including antidepressants, potentially acting as confounders. In an effort to partially address this bias, and given the large number of patients on antidepressant medication and other relevant medications acting on the CNS and known to potentially affect mood, a post hoc subgroup analysis was performed, which indicated that the observed changes in mood did not seem to be affected by such concomitant use. In addition, the quite recent occurrence of relapse events prior to PR-FAM treatment, though only in a limited number of patients, may also have a confounding effect in the results. Another limitation lies on the absence of a pre-definition of a “responder” to PR-FAM in terms of walking ability, which could result in significant variability in the physicians’ global judgement of response. Moreover, use of the PASAT to assess cognitive function entails a potential limitation due to a possible learning effect upon serial testing [33, 48]. Finally, it is important to be aware of the potential bias related to the self-report questionnaires utilized in this study, which may have been influenced by memory deficits or the desire to please the neurologist. On the one hand, self-reported measures successfully provide unique information of how patients feel and function, but, on the other hand, there are trade-offs including a risk of high spontaneous variability and a high placebo effect as a natural consequence of this variability [22]. Despite such limitations, the significance of our study lies in the fact that it highlights PR-FAM’s potential to improve various functions in MS besides walking ability in the context of real-life situations. Real-life studies, instead of employing strict inclusion/exclusion criteria resulting in a highly selective population, adopt pragmatic clinical settings in non-selected patients, even those with comorbidities or concomitant medications, who daily visit the physician, thus mimicking daily clinical practice [54, 55]. Thus, the “real-life” design of this study provides high external validity, which is further strengthened by the geographical site representation leading to an even more heterogeneous population potentially illustrative of the general population.
Conclusions
This “real-life” observational study provides new data to the current literature in support of the benefits of PR-FAM on broader MS aspects beyond walking ability in terms of cognition, fatigue, depression and overall QoL in a large and heterogeneous group of Greek patients under conditions of everyday clinical practice. Among them, improvements in fatigue, depression and QoL are shown to be more pronounced in patients also demonstrating a significant improvement in their walking ability as compared with the rest of the population, implying a potential advantage of this patient subgroup with regard to clinical response to PR-FAM. To this end, future more extensive studies to further characterize PR-FAM’s impact on these non-walking variables and their potential interaction are needed.
References
Albrecht P, Bjørnå IK, Brassat D, Farrell R, Feys P, Hobart J, et al. Prolonged-release fampridine in multiple sclerosis: clinical data and real-world experience. Report of an expert meeting. Ther. Adv. Neurol. Disord. 2018;11:1–8.
Ziemssen T. Multiple sclerosis beyond EDSS: depression and fatigue. J. Neurol. Sci. 2009;277(S1):S37–41.
Amato MP, Ponziani G, Rossi F, Liedl CL, Stefanile C, Rossi L. Quality of life in multiple sclerosis: The impact of depression, fatigue and disability. Mult Scler. 2001;7:340–4.
Rodriguez-Leal FA, Haase R, Akgün K, Eisele J, Proschmann U, Schultheiss T, et al. Nonwalking response to fampridine in patients with multiple sclerosis in a real-world setting. Ther Adv Chronic Dis. 2019;10:1–11.
Krupp L. Fatigue is intrinsic to multiple sclerosis (MS) and is the most commonly reported symptom of the disease. Mult Scler. 2006;12(4):367–8.
Lerdal A, Gulowsen Celius E, Krupp L, Dahl AA. A prospective study of patterns of fatigue in multiple sclerosis. Eur J Neurol. 2007;14(12):1338–43.
Braley TJ, Chervin RD. Fatigue in Multiple Sclerosis: Mechanisms, Evaluation, and Treatment. Sleep [Internet]. 2010;33:1061–7. Available from: https://doi.org/10.1093/sleep/33.8.1061
Tur C. Fatigue Management in Multiple Sclerosis. Curr. Treat. Options Neurol. 2016;18:26.
Rosti E, Hämäläinen P, Koivisto K, Hokkanen L. PASAT in detecting cognitive impairment in relapsing-remitting MS. Appl Neuropsychol. 2007;14(2):101–12.
Moccia M, Lanzillo R, Palladino R, Chang KCM, Costabile T, Russo C, et al. Cognitive impairment at diagnosis predicts 10-year multiple sclerosis progression. Mult Scler. 2016;22(5):659–67.
Patten SB, Marrie RA, Carta MG. Depression in multiple sclerosis [Internet]. Int. Rev. Psychiatry. Taylor and Francis Ltd; 2017;29(5):463–72. Available from: https://www.tandfonline.com/doi/full/https://doi.org/10.1080/09540261.2017.1322555.
Binzer S, McKay KA, Brenner P, Hillert J, Manouchehrinia A. Disability worsening among persons with multiple sclerosis and depression: A Swedish cohort study. Neurology. 2019;93:1–8.
Ysrraelit MC, Fiol MP, Gaitán MI, Correale J. Quality of life assessment in multiple sclerosis: Different perception between patients and neurologists. Front Neurol. 2018;8:729.
Dunn J, Blight A. Dalfampridine: A brief review of its mechanism of action and efficacy as a treatment to improve walking in patients with multiple sclerosis. Curr. Med. Res. Opin. 2011;27(7):1415–23.
EMA. Assessment Report; Fampyra [Internet]. 2011. Available from: https://www.ema.europa.eu/en/documents/assessment-report/fampyra-epar-public-assessment-report_en.pdf
EMA. Assessment Report; Fampyra [Internet]. 2017. Available from: https://www.ema.europa.eu/en/documents/variation-report/fampyra-h-c-2097-ii-0036-g-epar-assessment-report-variation_en.pdf
Korsen M, Kunz R, Schminke U, Runge U, Kohlmann T, Dressel A. Dalfampridine effects on cognition, fatigue, and dexterity. Brain Behav. 2017;7(1):e0059.
Broicher SD, Filli L, Geisseler O, Germann N, Zörner B, Brugger P, et al. Positive effects of fampridine on cognition, fatigue and depression in patients with multiple sclerosis over 2 years. J Neurol. 2018;265(5):1016–25.
Triche EW, Ruiz JA, Olson KM, Lo AC. Changes in cognitive processing speed, mood, and fatigue in an observational study of persons with multiple sclerosis treated with dalfampridine-ER. Clin Neuropharmacol. 2016;39(2):73–80.
Jacques F, Schembri A, Nativ A, Paquette C, Kalinowski P. Prolonged-release fampridine as adjunct therapy to active motor training in ms patients: a pilot, double-blind, randomized, placebo-controlled study. Mult Scler J Exp Transl Clin. 2018;4(1):2055217318761168.
Rodriguez-Leal FA, Haase R, Thomas K, Eisele JC, Proschmann U, Schultheiss T, et al. Fampridine response in MS patients with gait impairment in a real-world setting: Need for new response criteria? Mult Scler J. 2018;24(10):1337–46.
Hobart J, Ziemssen T, Feys P, Linnebank M, Goodman AD, Farrell R, et al. Assessment of clinically meaningful improvements in self-reported walking ability in participants with multiple sclerosis: results from the randomized, double-blind, phase III ENHANCE trial of prolonged-release fampridine. CNS Drugs. 2019;33(1):61–79.
Jensen HB, Nielsen JL, Ravnborg M, Dalgas U, Aagaard P, Stenager E. Effect of slow release-Fampridine on muscle strength, rate of force development, functional capacity and cognitive function in an enriched population of MS patients. A randomized, double blind, placebo controlled study. Mult Scler Relat Disord. 2016;10:137–44.
Morrow SA, Rosehart H, Johnson AM. The effect of Fampridine-SR on cognitive fatigue in a randomized double-blind crossover trial in patients with MS. Mult Scler Relat Disord. 2017;11:4–9.
Rossini PM, Pasqualetti P, Pozzilli C, Grasso MG, Millefiorini E, Graceffa A, et al. Fatigue in progressive multiple sclerosis: Results of a randomized, double-blind, placebo-controlled, crossover trial of oral 4-aminopyridine. Mult Scler. 2001;7(6):354–8.
Ruck T, Bittner S, Simon OJ, Göbel K, Wiendl H, Schilling M, et al. Long-term effects of dalfampridine in patients with multiple sclerosis. J Neurol Sci. 2014;337(1–2):18–24.
Pavsic K, Pelicon K, Ledinek AH, Sega S. Short-term impact of fampridine on motor and cognitive functions, mood and quality of life among multiple sclerosis patients. Clin Neurol Neurosurg. 2015;139:35–40.
Bakirtzis C, Konstantinopoulou E, Langdon DW, Grigoriadou E, Minti F, Nikolaidis I, et al. Long-term effects of prolonged-release fampridine in cognitive function, fatigue, mood and quality of life of MS patients: The IGNITE study. J Neurol Sci. 2018;395:106–12.
Allart E, Benoit A, Blanchard-Dauphin A, Tiffreau V, Thevenon A, Zephir H, et al. Sustained-released fampridine in multiple sclerosis: effects on gait parameters, arm function, fatigue, and quality of life. J Neurol. 2015;262(8):1936–45.
Jensen HB, Ravnborg M, Mamoei S, Dalgas U, Stenager E. Changes in cognition, arm function and lower body function after slow-release fampridine treatment. Mult Scler J. 2014;20:1872–80.
Satchidanand N, Drake A, Smerbeck A, Hojnacki D, Kolb C, Patrick K, et al. Dalfampridine benefits ambulation but not cognition in multiple sclerosis. Mult Scler J. 2020;26(1):91–8.
Valet M, Quoilin M, Lejeune T, Stoquart G, Van Pesch V, El Sankari S, et al. Effects of fampridine in people with multiple sclerosis: a systematic review and meta-analysis. CNS Drugs. 2019;33(11):1087–99.
Fischer JS, Rudick RA, Cutter GR, Reingold SC. The multiple sclerosis functional composite measure (MSFC): an integrated approach to MS clinical outcome assessment. Mult Scler. 1999;5(4):244–50.
Fischer JS, Jak AJ, Judith Kniker ME, Richard Rudick MA, Cutter G, Ellison G, et al. Administration and scoring manual manual prepared by administration and scoring manual. 2001
Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ. Measuring the impact of MS on walking ability: the 12-item MS Walking Scale (MSWS-12). Neurology. 2003;60(1):31–6.
Bakalidou D, Voumvourakis K, Tsourti Z, Papageorgiou E, Poulios A, Giannopoulos S. Validity and reliability of the Greek version of the Modified Fatigue Impact Scale in multiple sclerosis patients. Int J Rehabil Res. 2014;37(3):271–6.
Miskovic A, Ehrlich-Jones L. Measurement characteristics and clinical utility of the modified fatigue impact scale in individuals with multiple sclerosis. Arch Phys Med Rehabil. 2018;97(7):1219–20.
Giannakou M, Roussi P, Kosmides ME, Kiosseoglou G, Adamopoulou A, Garyfallos G. Adaptation of the beck depression inventory-II to greek population. Hell J Psychol. 2013;10(2):120–46.
Watson TM, Ford E, Worthington E, Lincoln NB. Validation of mood measures for people with multiple sclerosis. Int J MS Care. 2014;16(2):105–9.
Triantafyllou N, Triantafillou A, Tsivgoulis G. Validity and reliability of the greek version of the multiple sclerosis international quality-of-life questionnaire. J Clin Neurol. 2009;5(4):173–7.
Baumstarck K, Butzkueven H, Fernández O, Flachenecker P, Stecchi S, Idiman E, et al. Responsiveness of the Multiple Sclerosis International Quality of Life questionnaire to disability change: a longitudinal study. Health Qual Life Outcomes. 2013;11:127.
Jones KH, Ford DV, Jones PA, John A, Middleton RM, Lockhart-Jones H, et al. The physical and psychological impact of multiple sclerosis using the MSIS-29 via the web portal of the UK MS register. PLoS One. 2013;8(1):e55422.
Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018;17(2):162–73.
Ozakbas S, Yigit P, Cinar B. The effect of fampridine treatment on cognition: two year prospective study. Mult Scler J. 2017;23:412.
De Giglio L, De Luca F, Gurreri F, Ferrante I, Prosperini L, Borriello G, et al. Effect of dalfampridine on information processing speed impairment in multiple sclerosis. Neurology. 2019;9:1–14.
Foschi M, Lugaresi A. Evaluating dalfampridine for the treatment of relapsing-remitting multiple sclerosis: does it add to the treatment armamentarium? Expert Opin Pharmacother. 2019;20(11):1309–20.
Sumowski JF, Muhlert N. Dalfampridine improves slowed processing speed in MS: picking up the pace. Neurology. 2019;93(8):325.
Rosti E, Hämäläinen P, Koivisto K, Hokkanen L. One-year follow-up study of relapsing-remitting MS patients’ cognitive performances: paced auditory serial addition test’s susceptibility to change. J Int Neuropsychol Soc [Internet]. 2007;13:791–8. Available from: http://www.journals.cambridge.org/abstract_S1355617707071019
Sagawa Y, Magnin E, Paillot L, Moulin T, Decavel P. Fampridine and quality of life in individuals with multiple sclerosis. Springerplus. 2016;5(1):1070.
Khan F, Amatya B, Galea M. Management of fatigue in persons with multiple sclerosis. Front Neurol [Internet]. Frontiers Research Foundation; 2014;5:177. Available from: http://journal.frontiersin.org/article/https://doi.org/10.3389/fneur.2014.00177/abstract
Gasperini C, Hupperts R, Lycke J, Short C, McNeill M, Zhong J, et al. Prolonged-release fampridine treatment improved subject-reported impact of multiple sclerosis: Item-level analysis of the MSIS-29. J Neurol Sci. 2016;370:123–131. https://doi.org/10.1016/j.jns.2016.08.052.
Nagels G, Macdonell R, Soelberg Sorensen P, Pozzilli C, Laplaud D, de Jong B, et al. Long-Term Prolonged-Release Fampridine Treatment and Health-Related Quality of Life Outcomes: Interim Results of the Enable Study. Value Heal. 2013;16(7):627.
Hobart J, Blight AR, Goodman A, Lynn F, Putzki N. Timed 25-Foot Walk: Direct evidence that improving 20% or greater is clinically meaningful in MS. Neurology. 2013;16:1509–17.
Saturni S, Bellini F, Braido F, Paggiaro P, Sanduzzi A, Scichilone N, et al. Randomized controlled trials and real life studies A clinical point of view. Approaches and methodologies. Pulm Pharmacol Ther. 2014;27(2):129–38. https://doi.org/10.1016/j.pupt.2014.01.005.
Mahajan R. Real world data: Additional source for making clinical decisions. Int J Appl Basic Med Res. 2015;5(2):82. https://doi.org/10.4103/2229-516X.157148.
Acknowledgements
The authors would like to thank all participants of this study.
Funding
This study was co-funded by Biogen Idec International GmbH and Genesis Pharma S.A. Biogen Idec International GmbH and Genesis Pharma S.A also funded the journal’s Rapid Service and Open Access Fees.
Medical Writing and Editorial Assistance
The authors would also like to thank Sofia Poulou, InSciSol – Integrated Scientific Solutions,for medical writing support funded by Genesis Pharma S.A. and Biogen Idec International GmbH.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
All authors contributed to the study conception and design, as well as the collection, analysis, and interpretation of data. The first draft of the manuscript was written by InSciSol and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Dimos D. Mitsikostas has received grants from Biogen, Genzyme, Merz, ElectroCore; consulting fees or honoraria from Allergan, Amgen, Novartis, Roche, Teva and Mylan; travel support from Allergan, Amgen, Cefaly and Genesis Pharma; fees for participation in review activities from Novartis, Eli Lily, Amgen, Genesis Pharma and Teva; speaker’s fees from Eli Lily, Novartis, Merck-Serono, Teva and Roche. Dimitrios Papadopoulos has received honoraria for participation to advisory boards from Bayer, Genesis Pharma, Sanofi-Aventis and Novartis; travel support for national and international meetings from Bayer, Roche, Genesis Pharma, Merck, Sanofi-Aventis, Mylan and Novartis; speaker’s fees from Bayer, Genesis Pharma, Merck, Sanofi-Aventis, Novartis, Specifar and Teva. Nikolaos Fakas has received consultation fees and speaker’s honoraria from Genesis Pharma. Stylianos Gkatzonis, Panayiotis Mitsias, Maria Maltezou and Triantafyllos Doskas have no conflict of interest to declare. Rania Gourgioti is an employee of Genesis Pharma SA. No other potential conflict of interest relevant to this article was reported.
Compliance with Ethics Guidelines
The study was conducted in compliance with the principles laid down in the Declaration of Helsinki as well as with the local regulatory requirements, with approval obtained by the Ethics Committee of each participating site. A list of the respective Ethics Committees is included in Table S1. Written informed consent was obtained from all individual participants included in the study.
Data Availability
The authors declare that all relevant data supporting the findings of this study are available within the article.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mitsikostas, D.D., Doskas, T., Gkatzonis, S. et al. A Prospective, Observational, Cohort Study to Assess the Efficacy and Safety of Prolonged-Release Fampridine in Cognition, Fatigue, Depression, and Quality of Life in Multiple Sclerosis Patients: The FAMILY Study. Adv Ther 38, 1536–1551 (2021). https://doi.org/10.1007/s12325-020-01606-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01606-5