Abstract
Primary central nervous system lymphoma (PCNSL) is a highly aggressive non-Hodgkin lymphoma confined to the central nervous system. Diffuse large B cell lymphoma (DLBCL) is the most common subtype, and it follows a much more aggressive course than its systemic counterpart. Differential diagnosis of PCNSL and systemic DLBCL depends on clinical staging, which is expensive and time consuming. Protein kinase C delta (PKCD) is a protein with proapopitotic properties and has a major role in negative selection of B cells in germinal centers, a regulatory function in B cell receptor (BCR) pathway and MHC II expression. Mutations identified in its gene are reported to be unique for PCNSL and not encountered in systemic DLBCL. Our aim is to evaluate immunohistochemical (IHC) expression and the mutation status of PKCD in PCNSLs and systemic DLBCLs in order to find out whether PKCD could be a novel marker that could be used in differential diagnosis of both entities. A total of 43 cases diagnosed with PCNSL, and 43 cases diagnosed with systemic DLBCL were included in the study. Immunohistochemistry for PKCD antibody and Sanger sequencing targeting exon 16 and exon 18 of PKCD gene were performed. Although immunoreactivity for PKCD was observed in all PCNSL and 95.3% of systemic DLBCL cases, strong and diffuse staining was found to be more frequent in PCNSL than systemic diffuse large B cell lymphomas (p < 0.001). However, mutations defined in literature were not encountered in our cohort. While clinical staging is still the primary way for differential diagnosis of PCNSL and systemic DLBCL, the diffuse and strong PKCD expression can be used as a supportive feature for PCNSL diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphoma (PCNSL) is a rare and aggressive subtype of extra-nodal non-Hodgkin lymphomas (NHL). PCNSL must be confined to the central nervous system (brain, spinal cord, eyes, and leptomeninges) and there should be no evidence of systemic involvement or immunodeficiency [1]. PCNSL is mostly comprised of diffuse large B cell lymphomas (DLBCL) (> 90%) but its biology and behavior are different from its systemic counterpart [1, 2].
Regarding its difference to systemic DLBCL, protein kinase C delta (PKCD) mutations are reported to be specific for PCNSL [3, 4]. PKCD is a novel type of serine/threonine kinase in protein kinase C family [5]. It has a critical role in B cell maturation (specifically in negative selection), B cell receptor (BCR) pathway, and expression of the major histocompatibility class II (MHC II) antigens [6,7,8]. PKCD was proposed as a diagnostic marker for PCNSLs [9].
In this study we evaluated the immunohistochemical (IHC) expression of PKCD and its mutation status in PCNSLs and systemic DLBCLs in order to find out whether PKCD is a helpful diagnostic marker in the differential diagnosis of both entities.
Material and methods
Case selection
We retrieved 43 cases diagnosed with PCNSL between 2001 and 2019 and 43 cases diagnosed with systemic DLBCL between 2011 and 2020 from the archive records of Istanbul University, Istanbul Faculty of Medicine, and Department of Pathology. DLBCLs of the central nervous system with no known immunodeficiency, with no EBV virus infection (determined with EBER in situ hybridization), and no systemic involvement detected by standard staging procedures are accepted as PCNSL.
The control group consisted of systemic DLBCL cases with no association with EBV or immunodeficiency.
Immunohistochemistry
Immunohistochemistry was performed on the sections of the 10% formalin fixed paraffin embedded tissue blocks, representing the tumor, by using an automated immuno-stainer (Ventana Medical System-Benchmark XT/ISH Staining module).
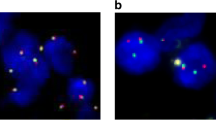
For PKCD, we used a monoclonal antibody directed at the C-terminal of the PKCD protein (Abcam, EPR17075, 1/2000). Urothelial carcinoma was used as positive and liver tissue was used as negative control (as recommended in the data sheet) and specific cytoplasmic staining was accepted as positive (Fig. 1). Staining intensity and extent of staining were evaluated as follows: extent of staining is defined as percentage of positive stained neoplastic cells, intensity of staining is scored as 3 + (strong staining), 2 + (moderate staining), 1 + (weak staining), and 0 (no reactivity).
Besides the PKCD antibody, each case was stained with CD3 (BioCare, LN10, 1/200), CD20 (BioCare, LN26, 1/200), CD10 (Abcam, 56C6, 1/60), bcl-6 (BioCare, LN22, 1/60), MUM1 (Abcam, MUM-1p, ready to use), bcl-2 (Sigma-Aldrich, 100/05, 1/100), Ki-67 (BioCare, MIB-1, 1/100), c-myc (Cell Marque, EP121, 1/50) antibodies, and EBER ISH (Roche).
PCNSLs were analyzed for cell of origin classification according to the Hans algorithm [10] and for double expresser phenotype. Both features were evaluated in conjunction with PKCD expression.
Sanger sequencing
Mutations in exon 16 and 18 of PKCD gene (NM_006254.4) were performed on representative formalin-fixed paraffin-embedded tumor samples by using the PCR-based direct sequencing (analytical sensitivity 25%) method. Tumor targets (> 75% viable tumor) were manually micro-dissected from 5-µm thick unstained histological sections for enrichment of tumor cellularity. Deparaffinization of the sections was performed. Then, DNA was isolated using QIAamp DNA FFPE Tissue Kit (50) (catalog #: 56,404) (QIAGEN, Hilden, Germany). The amplification process was carried out in a Thermal Cycler (Veriti 96‐Well Thermal Cycler, Applied Biosystems, Thermo Fisher Scientific Inc., Foster City, CA, USA). HotStarTaq DNA Polymerase kit (catalog #: 203,205) (QIAGEN, Hilden, Germany), forward (exon 16: 5′GGACCTCAAACTGGACAATGT′3, exon 18: 5′TGAAGCTCCAATTTCCCATG′3) and reverse (exon 16: 5′CTTGGACATCACTGCCCTTG′3, exon 18: 5′CGGCTGTGACTGAACATGC′3) primers were used in the preparation of PCR master mix. The final volume of PCR reactions was 50 µl. The mixture of PCR comprised of 200 ng of each tumor DNA, 6 µl of each primer (4 pmol/µl), 5 µl 10 × PCR Buffer, 1.5 µl 10 mM dNTP mix (Applied Biosystems, Thermo Fisher Scientific Inc., Foster City, CA, USA), 25 mM MgCl2 (3 μl for exon 16 and 1 μl for exon 18), 0.25 µl of Hot Start Taq DNA polymerase and nuclease free water. The PCR condition protocol consisted of an initial denaturation at 95 °C for 15 min, followed by 42 cycles of 30-s denaturation at 95 °C, 30-s optimized annealing at 53 °C (exon 16), at 58 °C (exon 18) and 45-s extension at 72 °C. The PCR run ended with a final extension at 72 °C for 10 min. The intensities of PCR products and reagent contamination control were analyzed by gel electrophoresis using a UV trans-illuminator (Gel Logic 200 Imaging System, Eastman Kodak Company, Rochester, NY, USA). Then, all succeeded PCR products were cleaned up to remove unincorporated primers and dNTPs for Sanger sequencing using QIAquick PCR Purification Kit (catalog #: 28,106) (QIAGEN, Hilden, Germany) according to the manufacturer’s instructions. The purified amplicons were sequenced in both the forward and reverse directions using reagents from the Big Dye Terminator v3.1 Cycle Sequencing kit (catalog #: 4,337,455) (Applied Biosystems, Thermo Fisher Scientific Inc., Foster City, CA, USA) in accordance with the manufacturer’s protocol. After ethanol precipitation, the reaction products were run on the ABI-3730 (48 capillary) automatic sequencer (Applied Biosystems, Thermo Fisher Scientific Inc., Foster City, CA, USA). Bidirectional sequence traces were analyzed with SeqScape® Software v3.0 (Applied Biosystems, Thermo Fisher Scientific Inc., Foster City, CA, USA) and manually reviewed.
Statistical analysis
Chi-squared and Fischer’s exact test and Statistical Package for Social Sciences (SPSS) v22.0 were used for statistical analysis. P-values less than 0.05 were considered statistically significant.
Results
Patient demography and clinical features
PCNSL group consists of 20 male and 23 female, and systemic DLBCL group consists of 21 male and 22 female patients. The mean age of PCNSLs was 62.81 ± 11.78 years ranging between 29 and 79 years, and 60.20 ± 16.7 years for systemic DLBCLs, ranging between 23 and 79 years.
A total of 40 PCNSL cases were supratentorial and 3 were infratentorial. Sites of origin for systemic lymphomas were nodal for 40 cases, soft tissue for 1 case, spleen for 1 case, and ovary for 1 case.
Histologic features
Diffuse pattern (30/43) is the most common growth pattern in PCNSL group. Followed by diffuse-perivascular (7/43), interstitial (3/43), interstitial-perivascular (2/43), and perivascular (1/43). Cytomorphological features of 7 cases could not be determined due to the crushing artifact. For the remaining 36 cases, 32 were centroblastic, 2 were immunoblastic, and 2 were centroblastic-immunoblastic (Fig. 2).
For the systemic DLBCL group, a diffuse infiltration pattern was observed in all cases and centroblastic morphology was the most common cytological feature (Fig. 3).
Immunohistochemical features
Positivity with PKCD was seen in 100% of the PCNSLs and 95.34% (41 cases) of systemic DLBCL cases (Table 1). Staining extent for PKCD in PCNSL cases was ranging between 60 and 100% (mean 93.48 ± 9.73). For PCNSL cases, 24 (55.81%) showed 3 + , 16 (37.20%) showed 2 + , and 3 (6.97%) showed 1 + staining with PKCD antibody (Fig. 2). In the systemic DLBCL cohort, staining extent was ranging between 0 and 100% (mean 87.20 ± 22.39). Eight (18.60%) cases showed 3 + , 25 (58.13%) cases showed 2 + , 8 (18.60%) cases showed 1 + staining with PKCD antibody, and 2 (4.65%) cases were negative (Fig. 3). While the difference in staining extent was not statistically significant, the differences in staining intensity between PCNSL and DLBCL were statistically significant for 3 + and ≥ 2 + staining (p < 0.001 and p = 0.035 respectively) (Table 1). The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for both thresholds are summarized in Table 2. For 3 + staining, sensitivity was 55.8% and specificity were 81.4%. For ≥ 2 + threshold, sensitivity increases up to 93% but specificity decreases to 23.2%.
Cell of origin classification according to Hans Algorithm [10] for PCNSL and systemic DLBCL is summarized in Table 3. Immunohistochemically 18 (41.86%) of 43 PCNSL cases showed double expressor phenotype. Mean value for Ki67 proliferation index was 74.12 ± 19.64.
When evaluated in conjunction with the cell of origin data, there was no statistically significant PKCD staining difference among cases with ABC or GBC phenotype in both PCNSL and systemic DLBCL cohorts.
The distribution of PKCD staining intensity score among cases with double expresser phenotype was as follows: 7 showed 3 + , 8 showed 2 + , and 3 showed 1 + . Among the 3 cases that show c-myc overexpression (> 40%) but negative for bcl2, one showed 3 + and two showed 2 + staining with PKCD. C-myc high (> 40%) cases have less intense PKCD expression when compared with c-myc low (< 40%) PCNSL cases (p = 0.045).
PKCD mutation analysis
Sanger sequencing was performed to find out whether this difference in protein expression has a genetic basis. Exon 16 and exon 18 were specifically targeted based on former studies [3, 4]. 3 + , 1 + , and negative cases were selected for sequencing. A total of 45 cases comprising 27 PCNSLs and 18 systemic DLBCLs underwent sequencing. Seven of 27 PCNSL and four of the 18 systemic DLBCL cases that met the criteria could not be sequenced due to the low DNA content.
The results of mutation analysis are summarized in Table 4. Systemic DLBCL cases showed no sequence variations in exon 16 and 18. In the PCNSL cohort, 5 cases showed sequence variations in exon 16 (2 cases) and 18 (3 cases). Variations c.1470 C > T (rs781875657) and c.1440 G > T (rs782332004) were located at exon 16 and variations c.1815 C > T (rs1553670466), c.1788 C > T, and c.1872 G > A were located at exon 18. All the point mutations were synonymous type and did not cause a change in protein sequence. Mutations defined in former studies [3, 4] were not encountered.
Discussion
PCNSL is a rare and aggressive subtype of extra-nodal NHLs [1]. Since PCNSL shares all the morphologic and immunophenotypic features of its systemic counterpart, currently, clinical staging is the only way to confirm the diagnosis [1, 11,12,13]. Although clinical staging is the gold standard for this differential, in reports of previously thought PCNSL cases having occult systemic disease [14,15,16], the time and cost of the clinical staging necessitate an approach that is cheaper, less time consuming and being able to detect PCNSL on a biological level. With reasons mentioned above and relevant information from the literature [3, 4, 9], we investigated immunohistochemical expression of PKCD in PCNSL and systemic DLBCs to determine whether it can fulfill this role.
The novel member of protein kinase C family PKCD has apoptotic functions; it is the negative regulator of B cell receptor (BCR) pathway and has a role in MHC II expression [6,7,8]. BCR pathway is an important oncogenic pathway in PCNSL [1, 2, 17, 18] making PKCD intriguing. Biallelic losses and missense-type mutations (p. A490V, p. M494V and p. W608S) affecting the amino acids in the catalytic region of the PKCD protein were identified in different studies, and these mutations were reported to be specific for PCNSLs [3, 4].
In our study, PKCD staining was found to be diffuse in both PCNSL and systemic DLBCL group, and its extent was generally more than 60%. Expression of PKCD did not seem to be correlated with cytomorphological features or COO classification according to Hans algorithm. When PCNSL group is divided by their c-myc expressions (high (> 40%) and low (< 40%)), we encountered a marginally significant difference (p = 0.045) for PKCD expression. PKCD staining intensity was lesser in cases with high c-myc expression. C-myc gene was one of the targets of the BCR pathway [2, 19], and lesser expression of one of its negative regulators could be a contributor to its higher expression.
The antibody used in our study is a monoclonal antibody that recognizes the carboxyl end of the PKCD. We observed strong (3 +) PKCD staining to be more frequent in PCNSLs (p < 0.001). As a diagnostic tool, strong (3 +) and weak (1 +)/no staining supports the diagnosis of PCNSL and systemic DLBCL respectively. However, moderate staining (2 +) comprised many cases in both groups and did not help in differential diagnosis. As this is the first study to use this antibody for this purpose, more data is needed for a definitive conclusion, especially with different antibody clones specific to different epitopes of the PKCD protein.
Since missense mutations were documented in the PKCD gene involving exons 16 and 18 [3, 4], these sites were selected for sequencing. Both abovementioned studies used whole exome sequencing (WES) and other next generation sequencing (NGS) methods and confirmed their findings by Sanger sequencing. Other than single nucleotide polymorphisms (SNPs), mutations defined in former studies, p. A490V, p. M494V, and p. W608S [3, 4] were not detected in our cohort by the Sanger sequencing. But we cannot make an argument about copy number variations since our method was not suitable for this purpose. Our results indicate that the difference in immunohistochemical expression of PKCD does not relate with the abovementioned mutations in exon 16 and 18. This leaves us with three possible explanations: (I) genetic abnormality causing this difference originates from a different location in PKCD gene that was not covered in our study, (II) epigenetic modifications, (III) mutations in BCR pathway other than PKCD gene [1, 2, 10, 12, 13].
To our knowledge, this study is the first study evaluating PKCD by IHC in PCNSLs. A reasonable number of PCNSL cases and evaluation of the defined genetic alterations in PKCD were the strong points, whereas the limited scope of sequencing of PKCD gene was the primary weak point.
While clinical staging is still the primary way for differential diagnosis between PCNSL and systemic DLBCL, the elevated PKCD expression in PCNSLs could be used as a supportive feature for PCNSL diagnosis. On the contrary, reduced expression can also be used in the same way for the systemic DLBCL infiltration of the CNS.
References
Cai Q, Fang Y, Young KH (2019) Primary central nervous system lymphoma: molecular pathogenesis and advances in treatment. Transl Oncol 12:523–538. https://doi.org/10.1016/j.tranon.2018.11.011
Deckert M, Montesinos-Rongen M, Brunn A, Siebert R (2014) Systems biology of primary CNS lymphoma: from genetic aberrations to modeling in mice. Acta Neuropathol 127:175–188. https://doi.org/10.1007/s00401-013-1202-x
Bruno A, Boisselier B, Labreche K, Marie Y, Polivka M, Jouvet A, Adam C, Figarella-Branger D, Miquel C, Eimer S, Houillier C, Soussain C, Mokhtari K, Daveau R, Hoang-Xuan K (2014) Mutational analysis of primary central nervous system lymphoma. Oncotarget 5:5065–5075. https://doi.org/10.18632/oncotarget.2080
Braggio E, Van Wier S, Ojha J, McPhail E, Asmann YW, Egan J, da Silva JA, Schiff D, Lopes MB, Decker PA, Valdez R, Tibes R, Eckloff B, Witzig TE, Stewart AK, Fonseca R, O’Neill BP (2015) Genome-wide analysis uncovers novel recurrent alterations in primary central nervous system lymphomas. Clin Cancer Res 21:3986–3994. https://doi.org/10.1158/1078-0432.CCR-14-2116
Mellor H, Parker PJ (1998) The extended protein kinase C superfamily. Biochem J 332(Pt 2):281–292. https://doi.org/10.1042/bj3320281
Limnander A, Zikherman J, Lau T, Leitges M, Weiss A, Roose JP (2014) Protein kinase Cδ promotes transitional B cell-negative selection and limits proximal B cell receptor signaling to enforce tolerance. Mol Cell Biol 34:1474–1485. https://doi.org/10.1128/MCB.01699-13
Kwon MJ, Soh JW, Chang CH (2006) Protein kinase C delta is essential to maintain CIITA gene expression in B cells. J Immunol 177:950–956. https://doi.org/10.4049/jimmunol.177.2.950
Kwon MJ, Yao Y, Walter MJ, Holtzman MJ, Chang CH (2007) Role of PKCdelta in IFN-gamma-inducible CIITA gene expression. Mol Immunol 44:2841–2849. https://doi.org/10.1016/j.molimm.2007.01.035
Shingleton JR, Dave SS (2018) Genetic convergence of rare lymphomas. Curr Opin Hematol 25:307–314. https://doi.org/10.1097/MOH.0000000000000435
Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, Müller-Hermelink HK, Campo E, Braziel RM, Jaffe ES, Pan Z, Farinha P, Smith LM, Falini B, Banham AH, Rosenwald A, Staudt LM, Connors JM, Armitage JO, Chan WC (2004) Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 103:275–282. https://doi.org/10.1182/blood-2003-05-1545
Rubenstein JL (2017) Biology of CNS lymphoma and the potential of novel agents. Hematology Am Soc Hematol Educ Program 2017:556–564. https://doi.org/10.1182/asheducation-2017.1.556
Sugita Y, Muta H, Ohshima K, Morioka M, Tsukamoto Y, Takahashi H, Kakita A (2016) Primary central nervous system lymphomas and related diseases: pathological characteristics and discussion of the differential diagnosis. Neuropathology 36:313–324. https://doi.org/10.1111/neup.12276
Phillips EH, Fox CP, Cwynarski K (2014) Primary CNS lymphoma. Curr Hematol Malig Rep 9:243–253. https://doi.org/10.1007/s11899-014-0217-2
Provencher S, Ferlay C, Alaoui-Slimani K, Devidas A, Lepretre S, de Prijck B, Sebban C, de la Fouchardiere A, Chassagne-Clement C, Ketterer N, Thyss A, Delannoy A, Tilly H, Biron P, Blay JY, Ghesquières H (2011) Clinical characteristics and outcome of isolated extracerebral relapses of primary central nervous system lymphoma: a case series. Hematol Oncol 29:10–16. https://doi.org/10.1002/hon.944
Batchelor T, Loeffler JS (2006) Primary CNS lymphoma. J Clin Oncol 24:1281–1288. https://doi.org/10.1200/JCO.2005.04.8819
Scott BJ, Douglas VC, Tihan T, Rubenstein JL, Josephson SA (2013) A systematic approach to the diagnosis of suspected central nervous system lymphoma. JAMA Neurol 70:311–319. https://doi.org/10.1001/jamaneurol.2013.606
Montesinos-Rongen M, Schmitz R, Brunn A, Gesk S, Richter J, Hong K, Wiestler OD, Siebert R, Küppers R, Deckert M (2010) Mutations of CARD11 but not TNFAIP3 may activate the NF-kappaB pathway in primary CNS lymphoma. Acta Neuropathol 120:529–535. https://doi.org/10.1007/s00401-010-0709-7
Montesinos-Rongen M, Schäfer E, Siebert R, Deckert M (2012) Genes regulating the B cell receptor pathway are recurrently mutated in primary central nervous system lymphoma. Acta Neuropathol 124:905–906. https://doi.org/10.1007/s00401-012-1064-7
Luo W, Weisel F, Shlomchik MJ (2018) B cell receptor and CD40 signaling are rewired for synergistic induction of the c-Myc transcription factor in germinal center B cells. Immunity 48:313-326.e5. https://doi.org/10.1016/j.immuni.2018.01.008
Funding
This study was funded by Istanbul University Scientific Research Projects Unit (BAP) with grant number TTU-2019–34909.
Author information
Authors and Affiliations
Contributions
Design: AYA, GY, and ÖD. Data collection and processing: AYA, GY, GÜ, and BB. Analysis or interpretation: AYA, GY, and İY. Literature search: AYA and GY. Writing: AYA and GY.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the Istanbul University, Istanbul Medical Faculty (No: 2019/810).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Altay, A.Y., Yilmaz, İ., Unverengil, G. et al. Protein kinase c delta expression in primary central nervous system lymphomas. J Hematopathol 15, 75–81 (2022). https://doi.org/10.1007/s12308-022-00490-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12308-022-00490-y