Abstract
Purpose
Triple-negative breast cancer (TNBC) is an aggressive subtype of breast cancer, more commonly diagnosed among black women than other subgroups. TNBC varies geographically, but little is known about area-level characteristics associated with elevated incidence.
Methods
We generated 2011–2013 age-adjusted TNBC incidence rates for state economic areas (SEAs) in 43 states using data from North American Association of Central Cancer Registries. For cases missing data on molecular markers, we imputed TNBC status using cross-marginal proportions. We linked these data to SEA covariates from national sources. Using linear ecological regression, we examined correlates of TNBC incidence rates for the overall population and for age (< 50 years or 50 + years)- or race (white or black)-specific subgroups.
Results
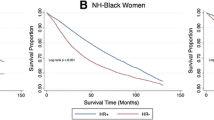
The mean annual incidence of TNBC across SEAs was 13.7 per 100,000 women (range = 4.5–26.3), with especially high and variable rates among African American women (mean = 20.5, range 0.0–155.1). TNBC incidence was highest in South Atlantic and East South Central Census Divisions and lowest in Mountain Division. Overall TNBC incidence was associated with SEA sociodemographics (e.g., percent of females age 45 + who are non-Hispanic black: coefficient estimate [est.] = 1.62), healthcare characteristics (e.g., percent of population without health insurance: est. = − 0.52), and health behaviors (e.g., prevalence of obesity among women: est. = 0.72) (all p < 0.05). Other variables related to TNBC incidence included density of obstetrician/gynecologists and prevalence of smoking.
Conclusion
TNBC incidence varied across SEAs in the U.S., particularly for African American women. Identifying areas with elevated TNBC incidence can facilitate research and interventions on area- and individual-level correlates of TNBC.



Similar content being viewed by others
References
National Cancer Institute. Cancer stat facts: Female breast cancer. 2018; https://seer.cancer.gov/statfacts/html/breast.html (2018).
Kohler BA, Sherman RL, Howlader N, et al. Annual report to the nation on the status of cancer, 1975–2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. J Natl Cancer Inst. 2015;107(6):djv048.
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V. Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype. Cancer. 2007;109(9):1721–8.
Carey LA, Perou CM, Livasy CA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295(21):2492–502.
Dawood S. Triple-negative breast cancer. Drugs. 2010;70(17):2247–58.
Yang XR, Sherman ME, Rimm DL, et al. Differences in risk factors for breast cancer molecular subtypes in a population-based study. Cancer Epidemiol Prev Biomarkers. 2007;16(3):439–43.
Howlader N, Altekruse SF, Li CI, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106(5):dju055.
Chollet-Hinton L, Anders CK, Tse CK, et al. Breast cancer biologic and etiologic heterogeneity by young age and menopausal status in the Carolina Breast Cancer Study: a case-control study. Breast Cancer Res. 2016;18(1):79.
Millikan RC, Newman B, Tse CK, et al. Epidemiology of basal-like breast cancer. Breast Cancer Res Treat. 2008;109(1):123–39.
Turkoz FP, Solak M, Petekkaya I, et al. Association between common risk factors and molecular subtypes in breast cancer patients. Breast. 2013;22(3):344–50.
Bandera EV, Chandran U, Hong C-C, et al. Obesity, body fat distribution, and risk of breast cancer subtypes in African American women participating in the AMBER Consortium. Breast Cancer Res Treat. 2015;150(3):655–66.
Wheeler SB, Reeder-Hayes KE, Carey LA. Disparities in breast cancer treatment and outcomes: biological, social, and health system determinants and opportunities for research. Oncologist. 2013;18(9):986–93.
U. S. Preventive Services Task Force. Final update summary: Breast cancer: Screening. (2016).
Collett K, Stefansson IM, Eide J, et al. A basal epithelial phenotype is more frequent in interval breast cancers compared with screen detected tumors. Cancer Epidemiol Prev Biomarkers. 2005;14(5):1108–12.
South SJ, Baumer EP. Deciphering community and race effects on adolescent premarital childbearing. Soc Forces. 2000;78(4):1379–407.
Anderson KN, Schwab RB, Martinez ME. Reproductive risk factors and breast cancer subtypes: a review of the literature. Breast Cancer Res Treat. 2014;144(1):1–10.
North American Association of Central Cancer Registries. Data standards & data dictionary, volume II. 2018; https://www.naaccr.org/data-standards-data-dictionary/ (2018).
U.S. Census Bureau. Geographic areas reference manual. 2015; https://www.census.gov/geo/reference/garm.html (2018)
Anderson WF, Katki HA, Rosenberg PS. Incidence of breast cancer in the United States: current and future trends. J Natl Cancer Inst. 2011;103(18):1397–402.
Howlader N, Noone A-M, Yu M, Cronin KA. Use of imputed population-based cancer registry data as a method of accounting for missing information: application to estrogen receptor status for breast cancer. Am J Epidemiol. 2012;176(4):347–56.
U. S. Census Bureau. American Community Survey (ACS). 2018; https://www.census.gov/programs-surveys/acs/, (2018).
U. S. Department of Health and Human Services. Area Health Resources Files 2016; https://data.hrsa.gov/topics/health-workforce/ahrf (2018).
Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. 2014; https://www.cdc.gov/brfss/ (2014).
National Cancer Institute. Small area estimates for cancer risk factors & screening behaviors. 2016; https://sae.cancer.gov/, (2018)
Brewer CA, Pickle L. Evaluation of methods for classifying epidemiological data on choropleth maps in series. Ann Assoc Am Geogr. 2002;92(4):662–81.
Richards TB, Berkowitz Z, Thomas CC, et al. Choropleth map design for cancer incidence, part 2. Prev Chronic Dis. 2010;7(1):A24.
Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences, vol. 3. London: Lawrence Erlbaum Associates; 2003.
Kogevinas M, Porta M. Socioeconomic differences in cancer survival: a review of the evidence. IARC Sci Publ. 1997;138(138):177–206.
Schinasi L, Leon ME. Non-Hodgkin lymphoma and occupational exposure to agricultural pesticide chemical groups and active ingredients: a systematic review and meta-analysis. Int J Environ Res Public Health. 2014;11(4):4449–527.
Singh GK, Siahpush M. Inequalities in US life expectancy by area unemployment level, 1990–2010. Scientifica. 2016;2016:8290435.
Ambroggi M, Biasini C, Del Giovane C, Fornari F, Cavanna L. Distance as a barrier to cancer diagnosis and treatment: review of the literature. Oncologist. 2015;20(12):1378–85.
Schneider BP, Winer EP, Foulkes WD, et al. Triple-negative breast cancer: risk factors to potential targets. Clin Cancer Res. 2008;14(24):8010–8.
Meilleur A, Subramanian SV, Plascak JJ, Fisher JL, Paskett ED, Lamont EB. Rural residence and cancer outcomes in the United States: issues and challenges. Cancer Epidemiol Biomark Prev. 2013;22(10):1657–67.
Kabat GC, Kim M, Phipps AI, et al. Smoking and alcohol consumption in relation to risk of triple-negative breast cancer in a cohort of postmenopausal women. Cancer Causes Control. 2011;22(5):775–83.
Dolle JM, Daling JR, White E, et al. Risk factors for triple-negative breast cancer in women under the age of 45 years. Cancer Epidemiol Biomarkers Prev. 2009;18(4):1157–66.
Kawai M, Malone KE, Tang MT, Li CI. Active smoking and the risk of estrogen receptor-positive and triple-negative breast cancer among women ages 20 to 44 years. Cancer. 2014;120(7):1026–34.
Dwyer-Lindgren L, Mokdad AH, Srebotnjak T, Flaxman AD, Hansen GM, Murray CJ. Cigarette smoking prevalence in US counties: 1996–2012. Popul Health Metrics. 2014;12(1):5.
Datta GD, Subramanian SV, Colditz GA, Kawachi I, Palmer JR, Rosenberg L. Individual, neighborhood, and state-level predictors of smoking among US Black women: a multilevel analysis. Soc Sci Med. 2006;63(4):1034–44.
Guzman GG. Household income. Am Commun Surv Br. 2016;2017:1–7.
Mathews T, Hamilton BE. Total fertility rates by state and race and Hispanic origin: United States, 2017. Natl Vital Stat Rep. 2019;68(1):1–11.
Beckfield J, Bambra C. Shorter lives in stingier states: Social policy shortcomings help explain the US mortality disadvantage. Soc Sci Med. 1982;2016(171):30–8.
Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156(5):471–82.
Rakha EA, Reis-Filho JS, Ellis IO. Basal-like breast cancer: a critical review. J Clin Oncol. 2008;26(15):2568–81.
Reis-Filho JS, Tutt AN. Triple negative tumours: a critical review. Histopathology. 2008;52(1):108–18.
Acknowledgements
These data are based on the NAACCR December 2016 data submission. Support for cancer registries is provided by the state, province or territory in which the registry is located. In the U.S., registries also participate in the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program or the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR) or both. In Canada, all registries submit data to the Canadian Cancer Registry maintained by Statistics Canada. The opinions expressed in this article are the authors’ own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Funding
The authors completed this work as part of active duty at the National Cancer Institute. No additional funding to support this project was received.
Author information
Authors and Affiliations
Contributions
JLM obtained, analyzed, and interpreted the data and drafted the manuscript. ZT assisted with data analysis and interpretation, and revised the manuscript. LZ assisted with data analysis and interpretation, and revised the manuscript. CM contributed to data cleaning, analysis, and interpretation, and revised the manuscript. KAC provided study oversight and assisted with data interpretation, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Moss, J.L., Tatalovich, Z., Zhu, L. et al. Triple-negative breast cancer incidence in the United States: ecological correlations with area-level sociodemographics, healthcare, and health behaviors. Breast Cancer 28, 82–91 (2021). https://doi.org/10.1007/s12282-020-01132-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-020-01132-w