Abstract
Background
Since complications of postmastectomy breast reconstruction may reduce patient satisfaction, we investigated complications of reconstruction with tissue expanders (TEs), particularly surgical site infections requiring TE/permanent implant (PI) removal.
Patients and methods
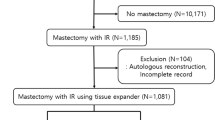
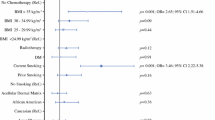
A retrospective review was performed of 234 primary breast cancer patients undergoing 239 postmastectomy breast reconstructions with TEs/PIs from 1997 to 2009. Clinicopathological findings and postoperative complications, particularly infections, were analyzed. Data were analyzed by the Chi-square test and a multivariate logistic regression model. TE infection risk factors considered for model inclusion were excisional biopsy, (neo) adjuvant chemotherapy, lymph node resection, body mass index (BMI), simultaneous bilateral reconstructions, and seroma aspiration.
Results
Removal of TEs/PIs was observed in 15.5 % (37/239) of reconstructions, and 18/37 underwent re-reconstructions. Of the 19/37 reconstructions that were not achieved completely, the most frequent reason was TE infection (11 reconstructions). The completion rate was 92 % (220/239 reconstructions) and it was significantly higher in reconstructions without TE infection than with infection (96 vs. 54 %, p < 0.0001). Patients with BMI ≥ 25 kg/m2 and seroma aspiration were more likely to develop TE infections (p = 0.0019, p < 0.001, respectively). By multivariate logistic regression analysis, seroma aspiration was a significant independent risk factor for TE infection (odds ratio 28.75, 95 % confidence interval 5.71–40.03, p < 0.0001).
Conclusion
To improve completion rates of breast reconstruction, prevention of TE infection plays a key role. We should reduce unnecessary seroma aspirations and delay elevation/exercise of the ipsilateral arm.

Similar content being viewed by others
References
Polivy J. Psychological effects of mastectomy on a woman’s feminine self-concept. J Nerv Ment Dis. 1977;164(2):77–87.
Ray C. Psychological implications of mastectomy. Br J Soc Clin Psychol. 1977;16(4):373–7.
Jamison KR, Wellisch DK, Pasnau RO. Psychosocial aspects of mastectomy: i. the women’s perspective. Am J Psychiatry. 1978;135(4):432–6.
Schover LR. Sexuality and body image in younger women with breast cancer. J Natl Cancer Inst Monogr. 1994;16:177–82.
Psychological response to mastectomy. A prospective comparison study. Psychological aspects of Breast Cancer Study Group. Cancer. 1987;59(1):189–96.
Casso D, Buist DS, Taplin S. Quality of life of 5-10 year breast cancer survivors diagnosed between age 40 and 49. Health Quality Life Outcomes. 2004;2:25.
Yurek D, Farrar W, Andersen BL. Breast cancer surgery: comparing surgical groups and determining individual differences in postoperative sexuality and body change stress. J Consult Clin Psychol. 2000;68(4):697–709.
Weitzner MA, Meyers CA, Stuebing KK, Saleeba AK. Relationship between quality of life and mood in long-term survivors of breast cancer treated with mastectomy. Support Care Cancer. 1997;5(3):241–8.
Dean C, Chetty U, Forrest AP. Effects of immediate breast reconstruction on psychosocial morbidity after mastectomy. Lancet. 1983;1(8322):459–62.
Ueda S, Tamaki Y, Yano K, Okishiro N, Yanagisawa T, Imasato M, Shimazu K, Kim SJ, Miyoshi Y, Tanji Y, et al. Cosmetic outcome and patient satisfaction after skin-sparing mastectomy for breast cancer with immediate reconstruction of the breast. Surgery. 2008;143(3):414–25.
Alderman AK, Wilkins EG, Lowery JC, Kim M, Davis JA. Determinants of patient satisfaction in postmastectomy breast reconstruction. Plast Reconstr Surg. 2000;106(4):769–76.
Al-Ghazal SK, Fallowfield L, Blamey RW. Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. Eur J Cancer. 2000;36(15):1938–43.
Nano MT, Gill PG, Kollias J, Bochner MA, Malycha P, Winefield HR. Psychological impact and cosmetic outcome of surgical breast cancer strategies. ANZ J Surg. 2005;75(11):940–7.
Al-Ghazal SK, Sully L, Fallowfield L, Blamey RW. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol. 2000;26(1):17–9.
Wellisch DK, Schain WS, Noone RB, Little JW 3rd. Psychosocial correlates of immediate versus delayed reconstruction of the breast. Plast Reconstr Surg. 1985;76(5):713–8.
Krueger EA, Wilkins EG, Strawderman M, Cederna P, Goldfarb S, Vicini FA, Pierce LJ. Complications and patient satisfaction following expander/implant breast reconstruction with and without radiotherapy. Int J Radiat Oncol Biol Phys. 2001;49(3):713–21.
Andrade WN, Baxter N, Semple JL. Clinical determinants of patient satisfaction with breast reconstruction. Plast Reconstr Surg. 2001;107(1):46–54.
Colakoglu S, Khansa I, Curtis MS, Yueh JH, Ogunleye A, Haewyon C, Tobias AM, Lee BT. Impact of complications on patient satisfaction in breast reconstruction. Plast Reconstr Surg. 2011;127(4):1428–36.
Disa JJ, Ad-El DD, Cohen SM, Cordeiro PG, Hidalgo DA. The premature removal of tissue expanders in breast reconstruction. Plast Reconstr Surg. 1999;104(6):1662–5.
Nahabedian MY, Tsangaris T, Momen B, Manson PN. Infectious complications following breast reconstruction with expanders and implants. Plast Reconstr Surg. 2003;112(2):467–76.
Francis SH, Ruberg RL, Stevenson KB, Beck CE, Ruppert AS, Harper JT, Boehmler JHt, Miller MJ. Independent risk factors for infection in tissue expander breast reconstruction. Plast Reconstr Surg. 2009;124(6):1790–6.
Ho A, Cordeiro P, Disa J, Mehrara B, Wright J, Van Zee KJ, Hudis C, McLane A, Chou J, Zhang Z, et al. Long-term outcomes in breast cancer patients undergoing immediate 2-stage expander/implant reconstruction and postmastectomy radiation. Cancer. 2012;118(9):2552–9.
Angarita FA, Acuna SA, Torregrosa L, Tawil M, Escallon J, Ruiz A. Perioperative variables associated with surgical site infection in breast cancer surgery. J Hosp Infect. 2011;79(4):328–32.
Barry M, Kell MR. Radiotherapy and breast reconstruction: a meta-analysis. Breast Cancer Res Treat. 2011;127(1):15–22.
Mitchem J, Herrmann D, Margenthaler JA, Aft RL. Impact of neoadjuvant chemotherapy on rate of tissue expander/implant loss and progression to successful breast reconstruction following mastectomy. Am J Surg. 2008;196(4):519–22.
Woerdeman LA, Hage JJ, Hofland MM, Rutgers EJ. A prospective assessment of surgical risk factors in 400 cases of skin-sparing mastectomy and immediate breast reconstruction with implants to establish selection criteria. Plast Reconstr Surg. 2007;119(2):455–63.
Gottschlich MM, Mayes T, Khoury JC, Warden GD. Significance of obesity on nutritional, immunologic, hormonal, and clinical outcome parameters in burns. J Am Diet Assoc. 1993;93(11):1261–8.
Smith AG, Sheridan PA, Harp JB, Beck MA. Diet-induced obese mice have increased mortality and altered immune responses when infected with influenza virus. J Nutr. 2007;137(5):1236–43.
Banerjee D, Williams EV, Ilott J, Monypenny IJ, Webster DJ. Obesity predisposes to increased drainage following axillary node clearance: a prospective audit. Ann R Coll Surg Engl. 2001;83(4):268–71.
Hoffman JP, Kusiak J, Boraas M, Genter B, Steuber K, Weese JL, Keidan RD, Eisenberg BL, Cox T, Litwin S. Risk factors for immediate prosthetic postmastectomy reconstruction. Am Surg. 1991;57(8):514–21; discussion 522.
Tadych K, Donegan WL. Postmastectomy seromas and wound drainage. Surg Gynecol Obstet. 1987;165(6):483–7.
Woodworth PA, McBoyle MF, Helmer SD, Beamer RL. Seroma formation after breast cancer surgery: incidence and predicting factors. Am Surg. 2000;66(5):444–50; discussion 450–441.
Nadkarni MS, Rangole AK, Sharma RK, Hawaldar RV, Parmar VV, Badwe RA. Influence of surgical technique on axillary seroma formation: a randomized study. ANZ J Surg. 2007;77(5):385–9.
Boostrom SY, Throckmorton AD, Boughey JC, Holifield AC, Zakaria S, Hoskin TL, Degnim AC. Incidence of clinically significant seroma after breast and axillary surgery. J Am Coll Surg. 2009;208(1):148–50.
Moyer KE, Potochny JD. Technique for seroma drainage in implant-based breast reconstruction. J Plast Reconstr Aesthet Surg. 2012;65(12):1614–7.
ten Wolde B, van den Wildenberg FJ, Keemers-Gels ME, Polat F, Strobbe LJ. Quilting prevents seroma formation following breast cancer surgery: closing the dead space by quilting prevents seroma following axillary lymph node dissection and mastectomy. Ann Surg Oncol. 2014;21(3):802–7.
Liang MD, Narayanan K, Ravilochan K, Roche K. The permeability of tissue expanders to bacteria: an experimental study. Plast Reconstr Surg. 1993;92(7):1294–7.
Watt-Boolsen S, Nielsen VB, Jensen J, Bak S. Postmastectomy seroma. A study of the nature and origin of seroma after mastectomy. Dan Med Bull. 1989;36(5):487–9.
Srivastava V, Basu S, Shukla VK. Seroma formation after breast cancer surgery: what we have learned in the last two decades. J Breast Cancer. 2012;15(4):373–80.
Shamley DR, Barker K, Simonite V, Beardshaw A. Delayed versus immediate exercises following surgery for breast cancer: a systematic review. Breast Cancer Res Treat. 2005;90(3):263–71.
Conflict of interest
All the authors have read the manuscript and approved this submission. No financial support for this study was provided. The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ota, D., Fukuuchi, A., Iwahira, Y. et al. Identification of complications in mastectomy with immediate reconstruction using tissue expanders and permanent implants for breast cancer patients. Breast Cancer 23, 400–406 (2016). https://doi.org/10.1007/s12282-014-0577-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-014-0577-4