Abstract
At an early stage, esophageal cancer can be removed surgically or endoscopically. T1a tumors are removed by endoscopic resection, whereas T1b tumors are preferably surgically removed (esophagectomy) due to possible lymph node involvement. However, the diagnostic tools (endoscopic ultrasonography (EUS) and CT/PET-CT) used to distinguish between T1a and T1b tumors and to detect malignant lymph nodes are imprecise. This study aimed to review the accuracy of preoperative locoregional staging in superficial esophageal cancer in a Danish setting. This was a retrospective, multicenter study including patients with a cT1 esophageal tumor, both adenocarcinoma and squamous cell carcinoma. Patients receiving neoadjuvant treatment were excluded. Results from the preoperative diagnostics tools were compared with the pathology report to determine the diagnostic accuracy. Sixty-eight patients were included, 34 patients underwent esophagectomy, and 34 patients underwent endoscopic resection. The positive predictive value (PPV) of PET-CT (or CT) (when staged as a T1 tumor) was 77% (95%CI: 0.59–0.88), and the PPV of EUS (when staged as a T1a or T1b tumor) was 52% (95%CI: 0.32–0.72) and 60% (95%CI: 0.36–0.82), respectively. Six patients had malignant lymph nodes in the surgical specimen; none of them was identified before surgery. In conclusion, neither CT/PET-CT nor EUS is a precise tool to distinguish mucosal from submucosal esophageal tumors. Furthermore, in superficial malignant lesions, lymph node involvement is rare, but when present, it is rarely detected before surgery. To improve staging accuracy, all patients with cT1 tumors could be referred for a diagnostic endoscopic resection prior to possible other treatments.
Similar content being viewed by others
Introduction
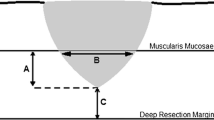
The correct staging of superficial esophageal cancer is of high importance to offer the patients the right treatment. In Denmark, 950 patients (16 per 100,000 inhabitants) are diagnosed with esophageal cancer every year [1], but the disease is rarely diagnosed at an early stage. According to European guidelines (ESMO Clinical Practice Guidelines updated in 2022 [2]), patients with a clinical-stage T1a (cT1a) tumor should be referred for endoscopic resection (ER), while in all stages beyond T1aN0, radical esophagectomy with lymphadenectomy should be considered. Some T1b tumors can be considered treated radically with only endoscopic resection, depending on invasion depth and ulceration [2]. This treatment strategy is based on the knowledge of a higher prevalence of lymph node involvement in more profound tumors [3,4,5,6,7,8,9]. In T1aAC (adenocarcinoma), endoscopic submucosal dissection (ESD) and endoscopic mucosal resection (EMR) are considered comparable [10]; in T1aSCC (squamous cell carcinoma), ESD seems superior compared with EMR and should be performed if possible [11]. However, as not all centers in Europe perform ESD, a lot of the patients will be referred for EMR instead. When performing EMR, larger lesions are removed piece-meal and, thus, are more difficult to examine histologically and to guarantee resection-free margins compared with ESD.
Multiple studies have investigated the best diagnostic tools to distinguish between early T-stages. Endoscopic ultrasonography (EUS), computed tomography (CT), and magnetic resonance imaging (MRI) have been evaluated. For locoregional staging, EUS seems to be the most accurate diagnostic tool, while CT is the most precise tool to identify metastases. Although, a recently published review showed that EUS might increase the risk of overdiagnosis of T1b tumors [12]. Several studies have shown that EUS can distinguish T1 and T2 tumors, but when it comes to discrimination between T1a (mucosal) and T1b (submucosal) tumors, the accuracy is significantly lower [12,13,14,15,16,17,18,19]. There seems to be no good tool to distinguish mucosal from submucosal tumors, even though it is crucial for the choice of treatment.
In the literature, the prevalence of lymph node metastases in superficial esophageal cancer differs from 1 to 23% [3, 4, 6, 7, 20,21,22,23]. For lymph node involvement, a meta-analysis including gastric cancer showed that EUS accuracy was not optimal, neither for N + confirmation nor exclusion [19], and the same seems to be applicable for esophageal tumors [24]. Another meta-analysis showed a sensitivity and specificity of > 84% in regard to lymph node involvement, and this could further be improved by combing EUS and FNA [25]. However, this is all tumor stages, and not only superficial lesions. Local nodal staging using FDG-PET is also limited, as discriminating the primary tumor from peritumoral lymph nodes is challenging [26].
Our primary aim was to review the accuracy of preoperative locoregional staging in superficial esophageal carcinomas in Denmark concerning both T- and N-stage. The primary focus was the use of EUS. It was hypothesized, in alignment with the literature, that EUS had low accuracy and that malignant lymph nodes were hard to identify preoperatively. Furthermore, it was hypothesized that the prevalence of lymph node metastases in pT1a tumors was low.
Patients and Methods
Study Design and Patient Selection
This was a retrospective, multicenter case series analysis. Inclusion criteria were as follows: age ≥ 18 years, a malignant tumor in the esophagus including the gastroesophageal junction, stage cT1 (based on EUS, 18F-FDG-PET-CT (flourine-18 fluorodeoxyglucose positron emission tomography), or CT scan), having undergone esophagectomy or ER (either ESD or EMR) between 1st of June 2016 and 31st of Dec 2020 at one of the three centers (“A,” “B,” “C”). Exclusion criteria were as follows: neoadjuvant treatment received or no malignant diagnosis before resection (only dysplasia). This study is reported according to the “Standards for Reporting Diagnostic accuracy studies” 2015 checklist.
Data Collection
Data was collected retrospectively at three out of four highly specialized national centers in 2021 and stored in Research Electronic Data Capture (REDCap) [27, 28]. Data included age, sex, tumor type, tumor location, staging tools, and results from these (CT, PET-CT, EUS, and fine-needle aspiration (FNA)). Furthermore, the type of treatment, number, and location of harvested lymph nodes, results from the pathological report, and any surgical re-treatment were registered. Lastly, survival and recurrence were registered.
Surgical Procedure
The patients with tumors staged as cT1b were most commonly referred for Ivor Lewis esophagectomy. In 2016, one center began to refer patients with cT1a tumors for ESD, which led to those patients with cT1a tumors undergoing either esophagectomy or ER during the cohort period. In the other centers, only smaller cT1a tumors (< 10 mm) were removed endoscopically (EMR). During the study period, diagnostic EMR was not routinely performed. If a tumor-free resection margin was not achieved after resection, the patient was offered a second treatment. During the period, the ESMO Clinical Practice Guidelines from 2016 were valid [29].
Staging
Tumors were staged according to the 8th edition of the American Joint Committee on Cancer (AJCC) Cancer Staging Manual [30]. As standard, all patients were evaluated with a CT scan, and most patients were further evaluated with a PET-CT scan. Unfortunately, PET-CT was not routinely performed at all three centers at the beginning of the trial period. Only patients evaluated for ER were examined with EUS. Both radial and linear endoscopic ultrasound scopes were used. If larger or irregular lymph nodes were identified, an FNA was taken. Afterward, all patients were evaluated by a multi-disciplinary team, and a treatment strategy was determined.
Statistical Analysis
The number of eligible patients determined the study size during the study period. General characteristics were described as mean with standard deviation if continuous, and categorical variables were described as the number of patients and percentages.
Accuracy, using the clinical and pathological stages for all modalities for each patient, was calculated as the number of correct stagings divided by the total sample size. A correct staging was defined as when the clinical stage allied with the pathological stage. The pathological report was considered the standard reference regarding both T- and N-staging. If a preoperative EUS was performed, this result overruled the results from the CT; otherwise, the results from the PET-CT or CT (in that order) were used as cT-stage. The results are presented as positive or negative predictive values. The 95% confidence intervals were calculated using the method of Wilson.
Recurrence and survival rates were analyzed using the Kaplan–Meier method and compared using a log-rank test.
Missing data were visually analyzed for patterns of missingness and hereafter interpreted as missing at complete random. A p-value < 0.05 was considered statistically significant. All statistical analyses were performed using the software R, version 1.4.1717.
Ethics
The study protocol was approved as a quality control trial by the hospital manager at each center. At the time of referral, all patients were asked to consent that their personal data might be used for research purposes, with permission from the hospital board. Patients who had not consented to this were excluded from the study. Only anonymized data were shared between centers.
Results
Patient Characteristics
Initially, 93 patients with a malignant tumor staged as cT1 were screened for inclusion (Fig. 1). Twenty patients were excluded due to the lack of a malignant confirmation before treatment (only dysplastic cells), four patients were excluded as they received neoadjuvant chemotherapy due to possible lymph node involvement, and one patient was excluded as the pathological report was missing. Lastly, 68 patients were included in the cohort.
There were 53 males (78%) and 15 women; ages varied from 41 to 84 years (mean age: 68.3 years). In 91% of the cases (n = 62), the tumor was located in the lower part of the esophagus (including the gastroesophageal junction), and 90% of the tumors (n = 61) were adenocarcinomas. Seven patients had squamous cell carcinoma. Initially, 34 patients underwent esophagectomy, and 34 patients were referred for ER. However, due to positive surgical margins, another six patients were referred for esophagectomy after ER. General characteristics are described in Table 1.
Preoperative Staging and Treatment Strategy
All patients were evaluated with a CT scan, 57 patients had a PET-CT, and 44 patients had an EUS performed. The treatment strategy was based on the results from these exams, as well as the patient’s medical and surgical history and patient’s wishes and preferences. In Table 2, the results from both EUS and CT/PET-CT are listed. Most tumors that were not detected with CT scan images were detected with EUS (only two tumors were not detected with EUS). Six patients had an FNA performed. Treatment distribution based on the cT-stage is listed in Fig. 2. In the table, both cT-stage and pT-stage are listed, as well as lymph node status. After the first ER, positive surgical margins were found in 15 cases (6 pT1a, 6 pT1b, 2 pT2, and one patient with only dysplastic cells). Five patients were referred for esophagectomy, six patients were offered a second ER, and the last four patients declined a second treatment. Out of the four patients who declined further treatment, two patients were still alive without any sign of recurrence at the end of the study, one patient was diagnosed with pulmonary metastases and died only 4 months after the initial treatment, and the last patient died 30 months after treatment without any clinical signs of recurrence. Lastly, one patient was referred for an esophagectomy after two ERs. Ten patients who underwent an esophagectomy had a pT1a tumor. In at least five of these cases, it was preoperatively described that the tumor was not suitable for or accessible by ER (longer Barrett’s esophageal segments, larger lesions, or the tumor location itself).
Treatment strategy and staging accuracy. The distribution of results from the preoperative staging, cT-stage based on EUS, or if not performed, a PET-CT or CT. Hereafter, the selected treatment strategy, pT-stage, and, if lymph node invasion, pTN-stage in the bottom. None of the malignant lymph nodes was detected before treatment. 1No visible tumor. *Referred for esophagectomy after ER due to positive resection margins
Accuracy of cT-Stage
EUS
Forty-four patients were evaluated with an EUS (Table 2) (no detectable tumor, cT1a, cT1b, or cT1x). Out of these, 20 patients initially underwent an esophagectomy. The positive predictive value of EUS when staged as a T1a or T1b tumor was 52% (95%CI: 0.32–0.72) and 60% (95%CI: 0.36–0.82), respectively. In five cases, histology revealed a pT2 tumor (three of them had a preoperative EUS performed, one was staged as a T1b tumor, and the other two as T1x), and two patients had a pT3 tumor (one of them had a preoperative EUS performed (T1a)).
PET-CT/CT Scan
Preoperative radiological T staging (from CT scan or PET-CT) was performed in all patients, and the results are listed in Table 2 (no detectable tumor, T1, or T2). The positive predictive value of PET-CT/CT when staged as a T1 tumor was 77% (95%CI: 0.59–0.88).
Accuracy of N-Stage
The pN-stage is only available for patients who had an esophagectomy (n = 40). The mean number of lymph nodes resected was 24 (SD = 10.7). Six patients had lymph node metastases after surgery (pT1a: no patients (0/12 resected pT1a tumors); pT1b: 4 patients (4/17); pT2: 1 patient (1/5); and pT3: 1 patient (1/2)). The results are seen in Fig. 2. The malignant lymph nodes in the T1b tumors were found in station 2, station 7, and the para esophageal station, station 9, and stations 3 and 4, respectively. The negative predictive value of the cN stage (combined results from CT, PET-CT, EUS, and FNA) was 85% (95%: 0.70–0.93). None of the true malignant lymph nodes was detected before surgery.
Recurrence and Survival
All patients were followed for at least 8 months after treatment. The total follow-up time was 2332 months (mean: 34 months). At the end of the trial, two patients had a local recurrence (at 204 and 559 days after ER, respectively), and seven patients had a distant recurrence (two patients treated with ER and five patients who underwent esophagectomy). Ninety-day survival was 100%. At the end of the follow-up period, 15 patients were dead. There was no difference in survival nor recurrence rates between the patients who underwent esophagectomy and the patients treated with ER (log-rank test; p = 0.7 (survival) and p = 0.9 (recurrence)). Survival curves are presented in Fig. 3.
Survival curves. Kaplan–Meier survival curves for patients who underwent esophagectomy (yellow) and patients who underwent ER (endoscopic resection) (black), respectively. Time is presented in days. At the end of the follow-up, 53 out of the 68 patients were still alive. There was no difference in survival between the two groups, log-rank test: p = 0.7
Discussion
In this study, it was once again stated that the diagnostic accuracy of EUS is low when it comes to distinguishing between T1a and T1b esophageal tumors. Furthermore, lymph node involvement in early esophageal cancer is rare (15% of patients undergoing esophagectomy in this cohort, only grade T1b or higher). Thus, no true malignant lymph nodes were acknowledged before surgery.
This study showed that only 52% of the T1a carcinomas and 60% of the T1b carcinomas were preoperatively staged correctly with EUS. It has previously been demonstrated in several studies that EUS has a high accuracy in diagnosing T1 cancers [16, 31]. However, its capability to distinguish between T1a and T1b carcinomas is debated. In a prospective study, including 372 patients with T1 esophageal cancer, it was concluded that EUS did not bring any extra value regarding the diagnostic accuracy of cancer invasion depth [12]. Since the treatment strategy (esophagectomy or ER) is based on the ability to distinguish submucosal from mucosal lesions, it is of the highest importance to highlight this. It is widely accepted that CT cannot be used in locoregional staging, and EUS is probably the best tool. Thus, it has been shown that within EUS, there is high interobserver variability between endoscopists [32], and its use as a standard diagnostic tool has been questioned [33]. Performed meta-analyses differ in their reporting; a meta-analysis from 2010 (including 12 studies) concluded that EUS was not sufficiently accurate in distinguishing between early tumors [18]. They recommend that when a superficial malignancy is suspected, an EUS should be performed to rule out deeper tumor invasion (stage T2 or higher) and lymph node involvement. This should be followed by a diagnostic ER. After histological examination, which allows for both assessment of cell differentiation and lymphovascular invasion, T1a tumors should be referred for endoscopic surveillance (if tumor-free resection margins are achieved), whereas the patients with T1b tumors should be referred for esophagectomy. By practicing this approach, the surgeon avoids referring patients with only T1a tumors for esophagectomy (where the risk of lymph node involvement is low), with all the risks entailed. There might be contraindications to ER, such as longer Barrett’s esophagus segments or larger lesions, and these patients should still be considered for esophagectomy. However, another meta-analysis (including 19 studies) from 2012 concluded that EUS was a good tool, and showed an area under the curve > 0.93 for both mucosal and submucosal lesions [34].
The question is: when aware of the limited accuracy of EUS to distinguish between T1a and T1b tumors, should we rely on the results from EUS and continue to refer patients for either esophagectomy or ER based upon it? From this dataset, it is tempting to conclude that we should not. Another alternative is to refer patients for diagnostic ER after the EUS has ruled out deeper tumor invasion. Hereafter, based on the specimen, a treatment strategy can be agreed upon by the multi-disciplinary team. A recently published Korean retrospective study [5] could demonstrate that patients with cT1a-stage esophageal cancer (evaluated from EUS), treated with endoscopic resection, did not have worse outcomes in terms of survival and disease-free survival (100% and 85%) compared with patients with cT1b stage disease treated with esophagectomy (78% and 77%). This is also confirmed in our data. These results imply that it is still safe to refer patients for ER, even though the results from EUS are not 100% reliable. A significantly lower complication rate was shown in the ESD group compared with patients undergoing esophagectomy in the same study. The risk of mortality and higher morbidity (anastomotic leak, stenosis, pneumonia, etc.) due to surgery alone versus the risk of local recurrence after ER must be considered. In our cohort, two patients treated with ER had local recurrence. Furthermore, the high interobserver variability, even when performed by experienced endoscopists (> 100 previous examinations), must be taken into count [32].
Regarding the prevalence of lymph node involvement, this study reported a prevalence of 15% among the 40 patients who underwent esophagectomy (pT1a: 0 patients, pT1b: 4 patients, pT2: 1 patient, and pT3: 1 patient). None of the malignant lymph nodes was acknowledged before surgery. However, only five patients with a cT1a tumor were referred for esophagectomy, which means there might be lymph node metastases we have overlooked. On the other hand, of the 12 patients who underwent esophagectomy and subsequently histologically verified pT1a tumor, none of them had lymph node metastases. This indicates that lymph node involvement in T1a tumors is rare, which is further confirmed by the low local recurrence rates. In this study, most patients (84%) had a PET-CT performed. However, in the analysis, it was not distinguished between CT and PET-CT. To improve the sensitivity of EUS regarding malignant lymph nodes, one can perform FNA biopsies from suspicious lymph nodes [35]. However, there is a risk of both false positive and false negative results [33]. FNAs were not commonly used in this cohort (only six patients), and none of them revealed malignant cells. These results, regarding both prevalence of lymph node metastases and the difficulty identifying them, are similar to other studies in the literature [23].
This study is limited by its retrospective nature. Only 68 patients were included; however, esophageal cancer in this early stage is rare. Furthermore, the cohort consisted of a heterogeneous group of patients, both regarding cancer types, but also treatment, and the three centers treated the patients slightly differently. The low patient number must be taken into account when the results are interpreted in a clinical setting, especially in patients with squamous cell carcinoma. Four patients were excluded due to neoadjuvant chemotherapy (all four patients were preoperatively staged as having lymph node involvement). This could potentially lower the incidence of malignant lymph nodes in our cohort. Patients with cT2 carcinomas were excluded, even though it appeared to be a pT1 tumor after surgery, since they were referred for neoadjuvant oncological treatment. Patients referred for ER due to high-grade dysplasia, but where the surgical specimen revealed malignant cells, were also excluded from the study. We hypothesized that the prevalence of malignant lymph nodes in pT1a tumors was low. However, the study was not powered to show this even; thus, no malignant lymph nodes were found in pT1a tumors. The study was neither powered to make conclusions regarding survival rates; however, the survival in this cohort is slightly lower than what would be expected from the literature. The strengths of this study are that only a few surgeons in each center did perform the EUS examinations, and all patients were evaluated by a multi-disciplinary team.
Conclusions
From this study, we can conclude that endoscopic ultrasound is not an accurate tool to distinguish mucosal from submucosal esophageal carcinomas. Furthermore, in early superficial esophageal cancer, lymph node involvement is rare, and rarely detected before surgery. No malignant lymph nodes were identified in pT1a tumors. Patients treated with endoscopic resection did not have a worsened survival outcome. Based upon this data, and other studies with similar findings, all patients with a cT1 esophageal cancer could be considered for a diagnostic endoscopic resection at first, and later patients with a pT1b tumor should be referred for esophagectomy (if deemed operable). This could potentially spare some patients a major surgical procedure.
Data Availability
The data supporting this study's findings are available from the corresponding author, [CE], upon reasonable request.
References
Dansk EsophagoGastrisk Cancer Gruppe database (DEGC), Årsrapport (2021). 2022. Accessed 13–07–2022
Obermannová R, Alsina M, Cervantes A, Leong T, Lordick F, Nilsson M, van Grieken NCT, Vogel A, Smyth EC (2022) Oesophageal cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. https://doi.org/10.1016/j.annonc.2022.07.003
Duan XF, Tang P, Shang XB, Jiang HJ (2018) Yu ZT (2018) The prevalence of lymph node metastasis for pathological T1 esophageal cancer: a retrospective study of 143 cases. Surg Oncol 27(1):1–6. https://doi.org/10.1016/j.suronc.2017.11.002
Dubecz A, Kern M, Solymosi N, Schweigert M, Stein HJ (2015) Predictors of lymph node metastasis in surgically resected T1 esophageal cancer. The Annals of thoracic surgery. 99(6):1879–85; discussion 1886. https://doi.org/10.1016/j.athoracsur.2015.02.112
Yang AJ, Choi SH, Byun HK, Kim HJ, Choi J, Lee YC, Lee SK, Park KR (2019) Lee CG (2019) Management of clinical T1N0M0 esophageal cancer. Gut Liver 13(3):315–324. https://doi.org/10.5009/gnl18254
Gamboa AM, Kim S, Force SD, Staley CA, Woods KE, Kooby DA, Maithel SK, Luke JA, Shaffer KM, Dacha S, Saba NF, Keilin SA, Cai Q, El-Rayes BF, Chen Z (2016) Willingham FF (2016) Treatment allocation in patients with early-stage esophageal adenocarcinoma: prevalence and predictors of lymph node involvement. Cancer 122(14):2150–2157. https://doi.org/10.1002/cncr.30040
Leers JM, DeMeester SR, Oezcelik A, Klipfel N, Ayazi S, Abate E, Zehetner J, Lipham JC, Chan L, Hagen JA (2011) DeMeester TR (2011) The prevalence of lymph node metastases in patients with T1 esophageal adenocarcinoma a retrospective review of esophagectomy specimens. Ann Surg 253(2):271–278. https://doi.org/10.1097/SLA.0b013e3181fbad42
Rice TW, Ishwaran H, Ferguson MK, Blackstone EH, Goldstraw P (2017) Cancer of the esophagus and esophagogastric junction an eighth edition staging primer. J Thorac Oncol 12(1):36–42. https://doi.org/10.1016/j.jtho.2016.10.016
Nigro JJ, Hagen JA, DeMeester TR, DeMeester SR, Peters JH, Oberg S, Theisen J, Kiyabu M, Crookes PF, Bremner CG (1999) Prevalence and location of nodal metastases in distal esophageal adenocarcinoma confined to the wall: implications for therapy. J Thorac Cardiovasc Surg. 117(1):16–23; discussion 23–5 https://doi.org/10.1016/s0022-5223(99)70464-2
Pech O, Bollschweiler E, Manner H, Leers J, Ell C, Hölscher AH (2011) Comparison between endoscopic and surgical resection of mucosal esophageal adenocarcinoma in Barrett’s esophagus at two high-volume centers. Ann Surg 254(1):67–72. https://doi.org/10.1097/SLA.0b013e31821d4bf6
Cao Y, Liao C, Tan A, Gao Y, Mo Z (2009) Gao F (2009) Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy 41(9):751–757. https://doi.org/10.1055/s0029-1215053
Ishihara R, Mizusawa J, Kushima R, Matsuura N, Yano T, Kataoka T, Fukuda H, Hanaoka N, Yoshio T, Abe S, Yamamoto Y, Nagata S, Ono H, Tamaoki M, Yoshida N, Takizawa K, Muto M (2021) Assessment of the diagnostic performance of endoscopic ultrasonography after conventional endoscopy for the evaluation of esophageal squamous cell carcinoma invasion depth. JAMA Netw Open. 4(9):e2125317
Kienle P, Buhl K, Kuntz C, Dux M, Hartmann C, Axel B, Herfarth C (2002) Lehnert T (2002) Prospective comparison of endoscopy, endosonography and computed tomography for staging of tumours of the oesophagus and gastric cardia. Digestion 66(4):230–236. https://doi.org/10.1159/000068360
Guo J, Wang Z, Qin J, Zhang H, Liu W, Zhao Y, Lu Y, Yan X, Zhang Z, Zhang T, Zhang S, Dominik NM, Kamel IR, Li H (2020) Qu J (2020) A prospective analysis of the diagnostic accuracy of 3 T MRI, CT and endoscopic ultrasound for preoperative T staging of potentially resectable esophageal cancer. Cancer Imaging 20(1):64. https://doi.org/10.1186/s40644-020-00343-w
Giganti F, Ambrosi A, Petrone MC, Canevari C, Chiari D, Salerno A, Arcidiacono PG, Nicoletti R, Albarello L, Mazza E, Gallivanone F, Gianolli L, Orsenigo E, Esposito A, Staudacher C, Del Maschio A (2016) De Cobelli F (2016) Prospective comparison of MR with diffusion-weighted imaging, endoscopic ultrasound, MDCT and positron emission tomography-CT in the pre-operative staging of oesophageal cancer: results from a pilot study. Br J Radiol 89(1068):20160087. https://doi.org/10.1259/bjr.20160087
He L-J, Shan H-B, Luo G-Y, Li Y, Zhang R, Gao X-Y, Wang G-B, Lin S-Y, Xu G-L (2014) Li J-J (2014) Endoscopic ultrasonography for staging of T1a and T1b esophageal squamous cell carcinoma. World J Gastroenterol 20(5):1340–1347. https://doi.org/10.3748/wjg.v20.i5.1340
Choi J, Kim SG, Kim JS, Jung HC (2010) Song IS (2010) Comparison of endoscopic ultrasonography (EUS), positron emission tomography (PET), and computed tomography (CT) in the preoperative locoregional staging of resectable esophageal cancer. Surg Endosc 24(6):1380–1386. https://doi.org/10.1007/s00464-009-0783-
Young PE, Gentry AB, Acosta RD, Greenwald BD (2010) Riddle M (2010) Endoscopic ultrasound does not accurately stage early adenocarcinoma or high-grade dysplasia of the esophagus. Clin Gastroenterol Hepatol 8(12):1037–1041. https://doi.org/10.1016/j.cgh.2010.08.020
Mocellin S (2015) Pasquali S (2015) Diagnostic accuracy of endoscopic ultrasonography (EUS) for the preoperative locoregional staging of primary gastric cancer. Cochrane Database Syst Rev 2:Cd009944. https://doi.org/10.1002/14651858.CD009944.pub2
Wang Y, Zhang X, Zhang X, Liu-Helmersson J, Zhang L, Xiao W, Jiang Y, Liu K (2021) Sang S (2021) Prognostic value of the extent of lymphadenectomy for esophageal cancer-specific survival among T1 patients. BMC Cancer 21(1):403–403. https://doi.org/10.1186/s12885-021-08080-4
Duan XF, Shang XB, Tang P, Jiang HJ, Gong L, Yue J, Ma MQ (2017) Yu ZT (2017) Lymph node metastasis and prognostic factors for T1 esophageal cancer. Zhonghua Wai Ke Za Zhi 55(9):690–695. https://doi.org/10.3760/cma.j.issn.0529-5815.2017.09.010
Rice TW, Ishwaran H, Hofstetter WL, Schipper PH, Kesler KA, Law S, Lerut EM, Denlinger CE, Salo JA, Scott WJ, Watson TJ, Allen MS, Chen LQ, Rusch VW, Cerfolio RJ, Luketich JD, Duranceau A, Darling GE, Pera M, Apperson-Hansen C (2017) Blackstone EH (2017) Esophageal cancer: associations with (pN+) lymph node metastases. Ann Surg 265(1):122–129. https://doi.org/10.1097/sla.0000000000001594
Aoyama J, Kawakubo H, Mayanagi S, Fukuda K, Irino T, Nakamura R, Wada N, Suzuki T, Kameyama K (2019) Kitagawa Y (2019) Discrepancy between the clinical and final pathological findings of lymph node metastasis in superficial esophageal cancer. Ann Surg Oncol 26(9):2874–2881. https://doi.org/10.1245/s10434-019-07498-2
Yokota T, Igaki H, Kato K, Tsubosa Y, Mizusawa J, Katayama H, Nakamura K, Fukuda H (2016) Kitagawa Y (2016) Accuracy of preoperative diagnosis of lymph node metastasis for thoracic esophageal cancer patients from JCOG9907 trial. Int J Clin Oncol 21(2):283–288. https://doi.org/10.1007/s10147-015-0899-z
Puli S-R, Reddy J-B, Bechtold M-L, Antillon D, Ibdah J-A (2008) Antillon M-R (2008) Staging accuracy of esophageal cancer by endoscopic ultrasound: a meta-analysis and systematic review. World J Gastroenterol 14(10):1479–1490. https://doi.org/10.3748/wjg.14.1479
Plukker JTM, van Westreenen HL Staging in oesophageal cancer. Baillière’s best practice & research Clinical gastroenterology. 20 (5):877–891. https://doi.org/10.1016/j.bpg.2006.05.001
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN (2019) The REDCap consortium: building an international community of software platform partners. Journal of Biomedical Informatics. 95:103208. https://doi.org/10.1016/j.jbi.2019.103208
Lordick F, Mariette C, Haustermans K, Obermannová R (2016) Arnold D (2016) Oesophageal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 27(suppl 5):v50–v57. https://doi.org/10.1093/annonc/mdw329
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, Meyer L, Gress DM, Byrd DR, Winchester DP (2017) The Eighth Edition AJCC Cancer Staging Manual continuing to build a bridge from a population based to a more “personalized” approach to cancer staging. CA: Cancer J Clin 67(2):93–99. https://doi.org/10.3322/caac.21388
Rampado S, Bocus P, Battaglia G, Ruol A, Portale G (2008) Ancona E (2008) Endoscopic ultrasound: accuracy in staging superficial carcinomas of the esophagus. Ann Thorac Surg 85(1):251–256. https://doi.org/10.1016/j.athoracsur.2007.08.021
Meining A, Rösch T, Wolf A, Lorenz R, Allescher HD, Kauer W (2003) Dittler HJ (2003) High interobserver variability in endosonographic staging of upper gastrointestinal cancers. Z Gastroenterol 41(5):391–394. https://doi.org/10.1055/s-2003-39422
Pouw RE, Heldoorn N, Alvarez Herrero L, ten Kate FJ, Visser M, Busch OR, van Berge Henegouwen MI, Krishnadath KK, Weusten BL, Fockens P (2011) Bergman JJ (2011) Do we still need EUS in the workup of patients with early esophageal neoplasia? A retrospective analysis of 131 cases. Gastrointest Endosc 73(4):662–668. https://doi.org/10.1016/j.gie.2010.10.046
Thosani N, Singh H, Kapadia A, Ochi N, Lee JH, Ajani J, Swisher SG, Hofstetter WL, Guha S (2012) Bhutani MS (2012) Diagnostic accuracy of EUS in differentiating mucosal versus submucosal invasion of superficial esophageal cancers: a systematic review and meta-analysis. Gastrointest Endosc 75(2):242–253. https://doi.org/10.1016/j.gie.2011.09.016
Vazquez-Sequeiros E, Norton ID, Clain JE, Wang KK, Affi A, Allen M, Deschamps C, Miller D, Salomao D (2001) Wiersema MJ (2001) Impact of EUS-guided fine-needle aspiration on lymph node staging in patients with esophageal carcinoma. Gastrointest Endosc 53(7):751–757. https://doi.org/10.1067/mge.2001.112741
Acknowledgements
Thanks to Grace Konstantin for proofreading this paper.
Funding
Open access funding provided by Royal Danish Library
Author information
Authors and Affiliations
Contributions
Project planning—Charlotte Egeland, Daniel Kjaer, Sarunas Dikinis, Hanne Grossjohann, and Michael Patrick Achiam.
Protocol writing—Charlotte Egeland and Michael Patrick Achiam.
Data collection—Charlotte Egeland, Anne Sofie Grundahl, and Cecilie Hübner.
Data analysis—Charlotte Egeland.
Writing—original draft preparation—Charlotte Egeland.
Writing—reviewing and editing—Charlotte Egeland, Anne Sofie Grundahl, Cecilie Hübner, Daniel Kjaer, Sarunas Dikinis, Hanne Grossjohann, and Michael Patrick Achiam.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Egeland, C., Grundahl, A.S., Hübner, C. et al. Staging Accuracy and Lymph Node Involvement in Superficial Adenocarcinoma and Squamous Cell Carcinoma of the Esophagus—a Multicenter Case Series Analysis. Indian J Surg 86, 98–105 (2024). https://doi.org/10.1007/s12262-023-03789-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-023-03789-x