Abstract
Mediastinal metastases represent an infrequent recurrence of breast carcinoma. Esophageal involvement by metastatic tissue is extremely rare. The situation means an unusual diagnostic and therapeutic challenge. Dignity of esophageal stricture is difficult to ascertain; endoscopy and picture giving methods might be conflicting. This study aimed to analyze the clinical characteristics and the therapeutic possibilities of the condition. A retrospective analysis of malignant esophageal stricture cases was performed from a prospectively collected database between 1984 and 2020. Out of 3996 cases with esophageal malignancy, 17 esophageal strictures were confirmed to be related to breast cancer metastasis. Surgical resection was feasible in 3 cases; endoprosthesis insertion was performed for palliation in 7 cases, and in 7 cases, only supportive care was available. Our incidence rate was 0.43%. Dysphagia indicating an affected esophagus presented on average 10.5 years after the primary tumor surgery. Mean duration between onset of symptoms achieving appropriate diagnosis was 6.4 months. Dignity of the malignancy was confirmed only retrospectively in one case. Morphologic findings showed an external esophageal compression in 52.9%, while in 35.3%, a destructive tumor growth affecting the mucosal layer could be found. Overall, survival was 7.6 months referring to 15 cases. The possible occurrence of mediastinal metastases involving the esophagus should be seriously considered in patients with previous breast cancer history. Biopsies obtained from the intact mucosal surface of the stenotic esophagus are often inefficient and misleading; therefore, repeated biopsies are necessary. Options for radical surgery are highly limited.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast carcinoma may give metastases to the mediastinal lymph nodes via the lymphatic vessels. These can asymptomatically persist even after the primary tumor excision and anticancer therapy. In some cases, malignancy recurs from the metastasis in the mediastinum, affecting the esophagus. The condition is difficult to diagnose. Most often, it is only detected in the autopsy findings [1,2,3]. A long tumor-free period is typical for these cases. Clinical signs of esophageal obstruction appear 8–17 years following the primary tumor surgery and the anti-cancer therapy. The course of the disease is rather different to primary esophageal tumor.
Materials and Methods
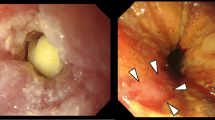
A total of 3996 cases treated at 1st Department of Surgery of Semmelweis University between 1984 and 2020 were diagnosed with malignant esophageal strictures. From them, 17 were proven having mediastinal metastasis from breast cancer. Patient demographics and symptomatic data are presented in Table 1. Table 2 shows clinicopathological characteristics. Diagnostic tools of the affected esophagus included barium swallow X-ray, endoscopy, endoscopic biopsy, histopathological tissue analysis, endoscopic ultrasound (EUS-guided FNAB), CT scan, MRI scan, PET-CT scan, bronchoscopy, and transbronchial biopsy (sampling, brush cytology). The area of the previous mastectomy was checked by diagnostic ultrasound scan and CT scan. The primary tumors of the patients were invasive adenocarcinoma. The origin of breast tumors in the mediastinal lesions was confirmed by immunohistochemical analysis (2nd Department of Pathology Semmelweis University). All patients were women whose anamneses included mastectomy, which was performed in other institutes. Primary tumor surgery was performed on every patient, followed by complex anti-cancer therapy (radiotherapy, chemotherapy) after which, the patients’ condition was considered as resolved. Preoperative evidence of breast cancer origin was successfully proven histologically in almost all but one esophageal stricture cases. In a case with progressing dysphagia presented 19 years after mastectomy, diagnostic procedures lasted 1 year. As a result, the short, funnel-like, and concentric stenosis covered with sound mucosa was thought to be benign. Supposed diagnoses were corrosive stricture or radiotherapy-induced lesion (Fig. 1). The stricture was dilated, which led to perforation. Acute transhiatal esophagectomy was performed upon detecting the perforation. Due to the promptly identified perforation, the mediastinal area was not inflamed, which enabled the acute orthotopic replacement with a gastric conduit. Histopathological tissue analysis of the resected esophagus confirmed the metastatic breast cancer origin. Esophagus exstirpation was a viable treatment in 3 out of the 17 cases (Table 3), perforated case included. All patients underwent transhiatal esophagectomies. In two cases a retrosternal route and in one case an orthotopic route for replacement procedure with cervical esophageal-gastric anastomosis were applied. No postoperative complication occurred. The tumor proved to be unresectable in 13 cases. Endoprosthesis implantation was performed in 7 cases as a form of palliative care. The following types of prostheses were used: Rüsch tube: 2 (Willy Rüsch AG, Kernen, Germany), Ultraflex self-expandable stent: 5 (Boston Scientific Corp. Watertown, USA). Supportive treatment only was applied in 7 cases despite a valid indication for prosthesis implantation. The inability of the stenotic segment to hold the prosthesis in situ hindered the intubation in 4 cases, the stricture emerging from the upper part of the esophagus was the reason in another, level of dysphagia of one patients did not needed any palliation, and one patient was not eligible for the treatment for her poor general condition. Data were collected and registered prospectively. Data analysis was performed with the SPSS 15.0 software (SPSS Inc. Chicago, Il, USA). The mean results are presented numerically, according to percentages; end values, the standard deviation (SD), and the 95% confidence interval are described.
Results
Among the 3996 patients, metastatic mediastinal tumor as the etiological background of the esophageal stricture was suspected in 31 cases (0.77%). Breast cancer was the underlying disease in 17 patients (0.43%) including the one patient whose condition was identified retrospectively. The investigations (partially performed in other institutes) lasted longer than usual with repeated examinations, and a significant amount of time was wasted, which was implied by the presence of dysphagia (Table 1). The radio-morphological findings were characterized by short-segmented, externally compressed multifocal esophageal strictures covered with intact mucosa (Fig. 2; Table 2). In 6 out of 17 cases, the tumor was infiltrating the mucosal layer (35.3%). The use of endoscopic ultrasound and the EUS-guided FNAB was impossible by the inability to guide the instrument into the narrowed esophagus. Histopathological confirmation of the diagnosis was only possible with repeated biopsies. CT scan findings described an atypical wall thickening of the esophagus in 90% of the cases. The resectability rate was 3/17. Eligibility rate for prosthesis implantation was 7/13. As the complications of the prosthesis implantation, airway compression syndrome occurred in one case, and obstruction of the esophageal prosthesis by food bolus impactation was seen in another during the late time period. Two patients are still alive in the time of publication. Mean overall survival of the 15 patients was 7.6 months (0–24), SD: 7.9, CI: 4.39. The survival of two patients out of the 3 cases that underwent esophagectomy was 8 and 15 months, and one patient is still alive after 18 months. Mean survival of patients, who received a prosthetic esophagus was 8.0 months (0–21), SD: 8.0, CI: 7.47. Overall survival of the 6 patients treated with supportive care was 5.8 months (1–24), SD: 9.1, CI: 9.55; one patient treated with supportive care is still alive since 6 months.
Discussion
According to different statistics derived from breast cancer autopsy reports, the prevalence of mediastinal metastases affecting the esophagus was 0.4–6% [1,2,3,4,5,6]. In majority of cases, esophageal stricture remains for a long time an asymptomatic phenomenon of malignant recurrence [7]. Liu described dysphagia as the primary symptom of malignancy [8]. The leading symptom of the developing malignancy, in the recovery period following the primary tumor surgery, is the slowly progressing swallowing difficulty, but dysmotility mimicking achalasia, corrosive stenosis, and nonspecific signs had also been described [4, 5, 9, 10]. Presumably, the mediastinal metastasis develops during the progression of the primary breast tumor. The molecular pathogenesis of the silent (inactive) metastasis transforming into a progressing malignancy is not sufficiently elucidated. The silent period is described as 2–23 years [3, 4, 7, 9, 11]. Progressive growing of metastatic mediastinal lymph nodes primarily causes compression; thereafter, it infiltrates the surrounding tissues, including the esophageal wall (Fig. 3). Symptoms are rather individual and can occur in different stages of the progression explaining complexity of diagnose. Mean interval between the occurrence of the first swallowing symptom until the therapy received was 8 months in average [4, 7, 9]. The diagnostic difficulty lies in the specific morphological characteristics of the strictures. The stenosis manifests as an extrinsic compression on the narrowed esophageal segment, protrudes inwardly to the esophageal lumen, and is covered with normal mucosal layer. Biopsies obtained from this area are usually negative. Even an almost completely obstructed, concentrically narrowed esophagus can present with normal mucosa. On the radiologic and endoscopic findings, the alteration can appear with smooth contour of mucosa indicating a deceptively benign morphology and can also mimic corrosive or other scar tissue–forming changes. Usually, treatment strategy for benign stenoses is defined by the grade and the expansion of the narrowed segment with taking the patient’s general condition into consideration. Most often, first-line treatment consists of conservative management in a type of dilation. Rampado drew attention to the rigid nature of esophageal strictures due to mediastinal metastases from breast cancer; dilation therapy was complicated by perforation in 26.7% of the patients [4, 9]. We experienced the same in one of our cases. If the endoscopic biopsies, which are crucial to confirm the histopathological background, show negative results, endoscopic ultrasound scan can be suggested. The dilation of the lumen might be necessary. There is a significant risk for perforation; however, a clear diagnosis can be made if the examination is successfully performed [12,13,14]. Breast cancer origin can be confirmed by immunohistochemical analysis. Feasibility of surgical treatment is frequently restricted by the progression and proliferation of the disease. Sunada successfully performed an endoscopic mucosal resection of a breast cancer metastasis from the esophageal wall [7]. Koike reported of a successfully performed surgical resection in one of the two cases described [15], along with one case each reported by Shimada and Anaya [9, 16]. Treatment is mostly limited to the palliation of dysphagia. Erman reported of radio-chemotherapy [11]. The main intervention for palliation is the endoprosthesis implantation. Maintaining the position of the prosthesis might be challenging for the externally compressed strictures. Prostheses therefore have a high tendency for migration. A positive anamnesis for primary tumor is highly relevant, even if the patient reports of a long, tumor-free period. After collecting relevant cases, Rampado denoted the pathophysiology of the metastatic breast cancer that involves the esophagus as “breast-esophagus syndrome” [4].
Conclusions
Esophageal strictures due to mediastinal metastases from breast cancer mean a significant diagnostic and therapeutic challenge, since they are relatively rare and difficult to identify and to establish correct histology. Possible management options are surgery, endoprosthesis implantation, palliative radio-chemotherapy, and supportive treatment.
Abbreviations
- CT:
-
Computed tomography
- EUS:
-
Endoscopic ultrasound
- FNAB:
-
Fine needle aspiration biopsy
- MRI:
-
Magnetic resonance imaging
- PET-CT:
-
Positron emission tomography-computed tomography
References
Abrams HL, Spiro R, Goldstein N (1950) Metastases in carcinoma; analysis of 1000 autopsied cases. Cancer 3(1):74–85
Graham WP 3rd (1964) Gastro-intestinal metastases from carcinoma of the breast. Ann Surg 159:477–480
Anderson MF, Harell GS (1980) Secondary esophageal tumors. AJR Am J Roentgenol 135(6):1243–1246
Rampado S, Ruol A, Guido M, Zaninotto G, Battaglia G, Costantini M et al (2007) Mediastinal carcinosis involving the esophagus in breast cancer: the “breast-esophagus” syndrome: report on 25 cases and guidelines for diagnosis and treatment. Ann Surg 246(2):316–322
Ambroggi M, Stroppa EM, Mordenti P, Biasini C, Zangrandi A, Michieletti E et al (2012) Metastatic breast cancer to the gastrointestinal tract: report of five cases and review of the literature. Int J Breast Cancer 2012:439023
Borst MJ, Ingold JA (1993) Metastatic patterns of invasive lobular versus invasive ductal carcinoma of the breast. Surgery 114(4):637–41 (discussion 41-2)
Sunada F, Yamamoto H, Kita H, Hanatsuka K, Ajibe H, Masuda M et al (2005) A case of esophageal stricture due to metastatic breast cancer diagnosed by endoscopic mucosal resection. Jpn J Clin Oncol 35(8):483–486
Liu A, Feng Y, Chen B, Li L, Wu D, Qian J et al (2018) A case report of metastatic breast cancer initially presenting with esophageal dysphagia. Medicine (Baltimore) 97(45):e13184
Anaya DA, Yu M, Karmy-Jones R (2006) Esophageal perforation in a patient with metastatic breast cancer to esophagus. Ann Thorac Surg 81(3):1136–1138
Varanasi RV, Saltzman JR, Krims P, Crimaldi A, Colby J (1995) Breast carcinoma metastatic to the esophagus: clinicopathological and management features of four cases, and literature review. Am J Gastroenterol 90(9):1495–1499
Erman M, Karaoglu A, Oksuzoglu B, Aydingoz U, Ayhan A, Guler N (2002) Solitary esophageal metastasis of breast cancer after 11 years: a case report. Med Oncol 19(3):171–175
Wiersema MJ, Wiersema LM, Khusro Q, Cramer HM, Tao LC (1994) Combined endosonography and fine-needle aspiration cytology in the evaluation of gastrointestinal lesions. Gastrointest Endosc 40(2 Pt 1):199–206
Sobel JM, Lai R, Mallery S, Levy MJ, Wiersema MJ, Greenwald BD et al (2005) The utility of EUS-guided FNA in the diagnosis of metastatic breast cancer to the esophagus and the mediastinum. Gastrointest Endosc 61(3):416–420
Herrera JL (1991) Benign and metastatic tumors of the esophagus. Gastroenterol Clin North Am 20(4):775–789
Koike M, Akiyama S, Kodera Y, Nakao A (2005) Breast carcinoma metastasis to the esophagus: report of two cases. Hepatogastroenterology 52(64):1116–1118
Shimada Y, Imamura M, Tobe T (1989) Successful esophagectomy for metastatic carcinoma of the esophagus from breast cancer–a case report. Jpn J Surg 19(1):82–85
Funding
Open access funding provided by Semmelweis University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Balázs, Á., Vass, T. & Baranyai, Z. Esophageal Strictures due to Mediastinal Metastases from Breast Cancer. Indian J Surg 85, 16–20 (2023). https://doi.org/10.1007/s12262-022-03369-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03369-5