Abstract
Purpose
Data on prognostic factors and treatment outcomes in patients with acute myeloid leukemia (AML) are usually based on highly selected patient groups. We analysed a cohort of unselected consecutive patients with AML diagnosed more than 10 years at a single institution.
Patients and methods
Treatment outcome and prognostic factors were retrospectively analysed in 147 AML patients. Treatment was selected according to study protocols of the OSHO (East German Study Group for Hematology and Oncology) if patients were eligible.
Results
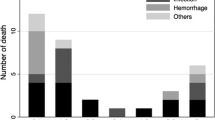
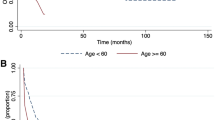
Median age at diagnosis was 68 years. Eighty-eight (59.9 %) patients were treated with curative intent, palliative treatment was given to 27.2 %, and supportive therapy only to 12.9 % of patients. Of patients aged £ 60 years, 97.7 % were treated with curative intent, versus only 43.7 % of those aged > 60 years. Curative treatment resulted in complete remission in 70 %, a median survival of 15.3 months, a significantly decreased early death rate (35 versus 68.4 %,P < 1 ´ 10− 8), and significantly prolonged survival compared to all other patients. This was also true for the sub-group of patients aged > 60 years. In multivariate analysis, age > 60 years, high cytogenetic risk, thrombocytopenia, leukocytosis and non-curative treatment intent emerged as risk factors for poor survival.
Conclusion
Outcome and prognostic parameters in unselected consecutive patients with AML treated in a single institution were found to be similar to those obtained in larger more selected patient cohorts. Our results confirmed that elderly patients should be treated with intensive treatment whenever possible to improve early death rate and overall survival.



Similar content being viewed by others
References
Ferlay J, Autier P, Boniol M, Heanue M, Colombet M, Boyle P. Estimates of the cancer incidence and mortality in Europe in 2006. Ann Oncol. 2007;18:581–92.
Leith CP, Kopecky KJ, Chen IM, Eijdems L, Slovak ML, McConnell TS, et al. Frequency and clinical significance of the expression of the multidrug resistance proteins MDR1/P-glycoprotein, MRP1, and LRP in acute myeloid leukemia: a southwest oncology group study. Blood. 1999;94:1086–99.
Appelbaum FR, Gundacker H, Head DR, Slovak ML, Willman CL, Godwin JE, et al. Age and acute myeloid leukemia. Blood. 2006;107:3481–5.
Hiddemann W, Kern W, Schoch C, Fonatsch C, Heinecke A, Wormann B, et al. Management of acute myeloid leukemia in elderly patients. J Clin Oncol. 1999;17:3569–76.
Burnett AK. The treatment of AML: current status and novel approaches. Hematology. 2005;10(Suppl 1): 50–3.
Lowenberg B, Zittoun R, Kerkhofs H, Jehn U, Abels J, Debusscher L, et al. On the value of intensive remission-induction chemotherapy in elderly patients of 65+ years with acute myeloid leukemia: a randomized phase III study of the European Organization for Research and Treatment of Cancer Leukemia Group. J Clin Oncol. 1989;7:1268–74.
Etienne A, Esterni B, Charbonnier A, Mozziconacci MJ, Arnoulet C, Coso D, et al. Comorbidity is an independent predictor of complete remission in elderly patients receiving induction chemotherapy for acute myeloid leukemia. Cancer. 2007;109:1376–83.
Baz R, Rodriguez C, Fu AZ, Jawde RA, Kalaycio M, Advani A, et al. Impact of remission induction chemotherapy on survival in older adults with acute myeloid leukemia. Cancer. 2007;110:1752–9.
Baudard M, Marie JP, Cadiou M, Viguie F, Zittoun R. Acute myelogenous leukaemia in the elderly: retrospective study of 235 consecutive patients. Br J Haematol. 1994;86:82–91.
Juliusson G, Antunovic P, Derolf A, Lehmann S, Mollgard L, Stockelberg D, et al. Age and acute myeloid leukemia: real world data on decision to treat and outcomes from the Swedish Acute Leukemia Registry. Blood. 2009;113:4179–87.
Menzin J, Boulanger L, Karsten V, Cahill A. Effects of initial treatment on survival among elderly AML patients: findings from the SEER-Medicare database. Blood. 2010;108:1973.
Hutchins LF, Unger JM, Crowley JJ, Coltman CA Jr, Albain KS. Underrepresentation of patients 65 years of age or older in cancer-treatment trials. N Engl J Med. 1999;341:2061–7.
Pallisgaard N, Hokland P, Riishoj DC, Pedersen B, Jorgensen P. Multiplex reverse transcription-polymerase chain reaction for simultaneous screening of 29 translocations and chromosomal aberrations in acute leukemia. Blood. 1998;92:574–88.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116:354–65.
Kantarjian H, O’Brien S, Cortes J, Giles F, Faderl S, Jabbour E, et al. Results of intensive chemotherapy in 998 patients age 65 years or older with acute myeloid leukemia or high-risk myelodysplastic syndrome: predictive prognostic models for outcome. Cancer. 2006;106:1090–8.
Vey N, Coso D, Bardou VJ, Stoppa AM, Braud AC, Bouabdallah R, et al. The benefit of induction chemotherapy in patients age 1619; 75 years. Cancer. 2004;101:325–31.
Menzin J, Lang K, Earle CC, Kerney D, Mallick R. The outcomes and costs of acute myeloid leukemia among the elderly. Arch Intern Med. 2002;162:1597–603.
Wahlin A, Billstrom R, Bjor O, Ahlgren T, Hedenus M, Hoglund M, et al. Results of risk-adapted therapy in acute myeloid leukaemia. A long-term population-based follow-up study. Eur J Haematol. 2009;83:99–107.
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children’s Leukaemia Working Parties. Blood. 1998;92:2322–33.
Deschler B, de WT, Mertelsmann R, Lubbert M. Treatment decision-making for older patients with high-risk myelodysplastic syndrome or acute myeloid leukemia: problems and approaches. Haematologica. 2006;91:1513–22.
Wheatley K, Brookes CL, Howman AJ, Goldstone AH, Milligan DW, Prentice AG, et al. Prognostic factor analysis of the survival of elderly patients with AML in the MRC AML11 and LRF AML14 trials. Br J Haematol. 2009;145:598–605.
Grimwade D, Walker H, Harrison G, Oliver F, Chatters S, Harrison CJ, et al. The predictive value of hierarchical cytogenetic classification in older adults with acute myeloid leukemia (AML): analysis of 1065 patients entered into the United Kingdom Medical Research Council AML11 trial. Blood. 2001;98:1312–20.
Burnett AK, Milligan D, Goldstone A, Prentice A, McMullin MF, Dennis M, et al. The impact of dose escalation and resistance modulation in older patients with acute myeloid leukaemia and high risk myelodysplastic syndrome: the results of the LRF AML14 trial. Br J Haematol. 2009;145:318–32.
Farag SS, Archer KJ, Mrozek K, Ruppert AS, Carroll AJ, Vardiman JW, et al. Pretreatment cytogenetics add to other prognostic factors predicting complete remission and long-term outcome in patients 60 years of age or older with acute myeloid leukemia: results from Cancer and Leukemia Group B 8461. Blood. 2006;108:63–73.
Behringer B, Pitako JA, Kunzmann R, Schmoor C, Behringer D, Mertelsmann R, et al. Prognosis of older patients with acute myeloid leukemia receiving either induction or noncurative treatment: a single-center retrospective study. Ann Hematol. 2003;82:381–9.
Frohling S, Schlenk RF, Kayser S, Morhardt M, Benner A, Dohner K, et al. Cytogenetics and age are major determinants of outcome in intensively treated acute myeloid leukemia patients older than 60 years: results from AMLSG trial AML HD98-B. Blood. 2006;108:3280–8.
Itzykson R, Thepot S, Beyne-Rauze O, Quesnerl B, Ame S, Turlure P, et al. Prolonged survival without complete remission (CR) in AML patients (Pts) treated with adacitidine (AZA). Blood. 2010;116(22):2183.
Acknowledgments
We thank Brigitte Brixler for her support in collecting patient data and Prof. Dietger Niederwieser as principal investigator of the OSHO study group for permission to use data of patients treated within OSHO studies. The work was supported by the Austrian Forum against cancer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Strasser-Weippl, K., Schreder, M., Zojer, N. et al. Treatment outcome in AML: a single-centre experience in an unselected patient cohort. memo 5, 134–140 (2012). https://doi.org/10.1007/s12254-012-0011-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12254-012-0011-6